Call the clinic +7 928 828 4001
Prices for services
| Service | Price |
| ECG | 500 ք |
| Echocardiography (ultrasound of the heart) | 2000 ք |
| Consultation with a gynecologist | 1350* ք |
| Electrocardiogram (ECG) | 500 ք |
| CARDIOTOCOGRAPHY | 500 ք |
| Cardiotocography | 500 ք |
| Consultation with a cardiologist-arrhythmologist | 1350* ք |
The presence of what symptoms is a reason to visit a cardiologist-arrhythmologist?
- Arrhythmia, which includes a slow or rapid heartbeat or skipped beats;
- Pain in the heart area. This symptom does not always specifically indicate heart problems, but it is still worth checking with a cardiologist-arrhythmologist;
- Weakness and fatigue that occur for no apparent reason;
- Unreasonable irritability;
- High sensitivity to temperature changes;
- Weak potency;
- Menstrual irregularities;
Cardiac ischemia
How does coronary heart disease occur?
The heart is the main organ of the human cardiovascular system. The contracting heart forces blood to circulate through the vessels, delivering oxygen and nutrients to organs and tissues. During the day, the heart makes about 100,000 beats and pumps up to 170 liters of blood!
Each heart cell must also constantly receive oxygen and nutrients. This process is ensured by continuous blood flow through the heart’s own arteries – the right and left coronary arteries.
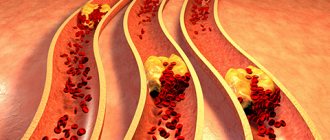
A normally functioning heart practically does not bother us. But if at least one artery narrows or becomes blocked, then the oxygen brought by the bloodstream becomes insufficient for the heart and ischemia occurs. The most common cause of narrowing in the coronary arteries is atherosclerotic plaques.
Coronary heart disease (CHD) develops as a result of the accumulation of atherosclerotic plaques in the coronary arteries, which causes an imbalance between coronary blood flow and the metabolic needs of the heart muscle (myocardium). In other words, the myocardium needs more oxygen than it can get from the blood.
Types of coronary heart disease. Angina pectoris
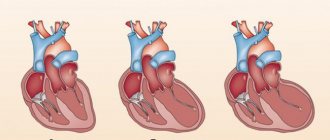
The course of IHD can be acute - in the form of myocardial infarction, a life-threatening condition requiring emergency treatment, or chronic - in the form of periodic attacks of angina.
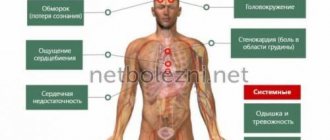
Angina is a clinical syndrome caused by myocardial ischemia and characterized by pain or discomfort in the chest, near the sternum, but can be felt anywhere from the upper abdomen to the lower jaw and shoulder blades. The pain may radiate to the arms and back. Most often, patients describe this pain as pressure, heaviness, burning or discomfort. This condition may be accompanied by weakness, a feeling of shortness of breath, anxiety and even fear of death. The duration of pain during angina is short, usually less than 10-15 minutes. Most often, the onset of pain is associated with physical or psycho-emotional stress, but in severe cases, pain can also occur in a state of complete rest. The pain usually goes away with rest or after taking nitroglycerin. In some cases, there may be an atypical or asymptomatic course of ischemia, which changes the clinical picture of the disease and sometimes misleads the patient himself.
Risk factors predisposing to the development of coronary artery disease
Biological factors:
- elderly age
- male
- family predisposition to ischemic heart disease
Genetic factors contributing to the occurrence of arterial hypertension, dyslipidemia, diabetes mellitus and obesity.
Pathophysiological and metabolic factors:
- hyperlipidemia – increased levels of lipids and lipoproteins in the blood
- arterial hypertension - an increase in systolic blood pressure up to 140 mm Hg. Art. and higher and diastolic blood pressure ≥ 90 mm Hg. Art.
- obesity - body mass index (BMI) greater than or equal to 30 kg/m2;
- diabetes
- menopause
- hyperuricemia – increased level of uric acid in the blood serum ≥360 µmol/l
Behavioral and social factors:
- eating habits, not healthy eating
- smoking
- physical inactivity – low physical activity
- alcohol consumption;
- stress
The likelihood of developing coronary heart disease increases proportionally as the number and severity of these risk factors increases.
How to assess your risk of cardiovascular disease
In order to assess cardiovascular risk, that is, to determine the likelihood of developing a particular adverse event from the cardiovascular system (including the development of cardiovascular diseases and their complications) over a certain period of time (for example, over a period of 10 years), you can use the SCORE scale.
The SCORE (Systematic COronary Risk Evaluation) scale is used to assess the risk of death from cardiovascular diseases over the next 10 years in people over 40 years of age. To determine risk, 4 indicators are needed: age, smoking, total cholesterol and systolic blood pressure. Before age 60, the cardiovascular risk of men is higher than that of women. After 60 years, the risks are almost the same.
To calculate risk on the SCORE scale, you need:
Select a column and row at the intersection of gender, age, smoking, as well as systolic blood pressure and total cholesterol levels.
The resulting cell will indicate the risk of developing cardiovascular disease over the next 10 years.
SCORE 2021. 10-year risk of fatal CVD.
How to decipher the result:
- If the rate is <1% - low risk
- From 1 to 5% – moderate risk
- From 5 to 10% – high risk
- Above 10% – very high risk
The risk assessment should be adjusted upward if the patient approaches the borderline values.
It is important to know that the SCORE scale is not intended for those who already have cardiovascular diseases: coronary artery disease, heart attacks, strokes, as well as diabetes mellitus with target organ damage, severe chronic kidney disease. Such patients are initially at high or very high risk and require medical supervision.
Risk assessment allows you to assess the patient's potential prognosis and take all necessary measures to reduce the risk as much as possible by modifying risk factors and timely changing approaches to treating the patient.
Diagnosis of coronary heart disease
If coronary artery disease is suspected, the cardiologist, depending on the patient’s condition, prescribes a basic or more in-depth examination necessary for a detailed understanding of the patient’s condition and prescribing the correct and most optimal treatment.
The basic diagnosis of IHD (1st line studies) includes standard laboratory biochemical tests, ECG recording at rest, if possible, ambulatory ECG monitoring, echocardiography at rest and, in some patients, chest x-ray.
More in-depth methods for diagnosing heart conditions, performed according to indications, include:
stress echocardiography (with physical activity or drug tests)
- radionuclide research methods
- magnetic resonance imaging and angiography
- multispiral computed angiography
- optical coherence tomography
- positron emission tomography
- coronary angiography, etc.
These techniques make it possible to assess the severity of myocardial damage and the degree of narrowing of the lumen of the coronary arteries. It is generally accepted that narrowing of the lumen of the coronary artery by more than 50% is one of the main indications for myocardial revascularization.
Modern approaches to the treatment of ischemic heart disease
The main goals of treatment for coronary artery disease include eliminating or minimizing angina attacks, reducing the risk of adverse disease outcomes (death, myocardial infarction, stroke), and increasing life expectancy. In most cases, achieving this goal is possible by modifying lifestyle and prescribing optimal drug therapy - therapy that allows you to achieve and maintain optimal blood lipid levels (total cholesterol, LDL, triglycerides, etc.), pulse, blood pressure, etc. over time) .
Non-drug treatment methods for ischemic heart disease include:
- dieting
- maintaining recommended physical activity
- body weight control
- complete cessation of smoking
- healthy eating
Healthy eating Today it has been proven that adherence to the Mediterranean diet leads to a significant reduction in cardiovascular mortality.
- High proportion of fresh fruits, vegetables, potatoes, beans, nuts, seeds.
- Bread, pasta and other grain-based products.
- Fruits are a daily dessert.
- Olive oil and other sources of fats that are not fatty acids are the main source of energy, providing 25-35% of all calories.
- Dairy products, mostly yogurt and cheese.
- Eggs are not consumed at all or no more than eggs per week.
- Fish and poultry are consumed in small to medium quantities.
- Animal meat is consumed in small quantities.
Moderate consumption of red wine, usually with food (except in Muslim countries).
Diet is inextricably linked with an active lifestyle.
Physical activity
According to the latest recommendations, a patient with coronary artery disease is recommended to do up to 150 minutes per week of moderate physical activity and at least 30 minutes per day of static exercise.
Physical activity reduces mortality in patients with stable coronary artery disease, especially those leading a sedentary lifestyle. Static loads are carried out strictly under the control of well-being (they should be limited in case of severe IHD).
Body weight control
Both overweight and obesity are associated with an increased risk of death due to coronary artery disease. Losing body weight allows you to optimize the results of treatment not only for coronary artery disease, but also for arterial hypertension, diabetes mellitus, dyslipidemia, etc.
Drug treatment of chronic ischemic heart disease
includes the prescription of drugs that have proven their ability to eliminate angina attacks, reduce the risk of complications and increase life expectancy. These include statins, antiplatelet drugs, beta blockers, angiotensin converting enzyme inhibitors, calcium antagonists, nitrates, etc.
In case of ineffectiveness of drug treatment or in the presence of a high or extremely high risk of developing cardiovascular complications, the need for surgical treatment of coronary artery disease - myocardial revascularization - should be considered.
Surgical treatment of ischemic heart disease
Myocardial revascularization can effectively relieve symptoms of angina, reduce the use of antianginal drugs, and improve exercise capacity and quality of life.
The purpose of performing myocardial revascularization is to relieve the symptoms of angina pectoris, prevent the development of acute myocardial infarction and improve the prognosis of the disease. Methods of myocardial revascularization include:
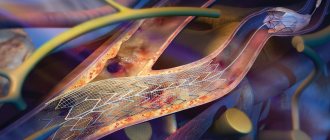
- Angioplasty of the coronary arteries with stenting is a type of minimally invasive operation that allows you to expand the narrowed area of the coronary artery using a special balloon (the balloon is carried to the heart through a puncture in the femoral artery in the leg or the radial artery in the arm) and install a stent in the narrowed area - a design that allows you to keep it patent lumen of the corona artery. After the intervention, medications are required to reduce the risk of stent thrombosis. a type of minimally invasive operation that allows you to expand the narrowed area of the coronary artery using a special balloon (the balloon is passed to the heart through a puncture in the femoral artery in the leg or the radial artery in the arm) and install a stent in the narrowed area - a design that allows you to keep the lumen of the coronary artery patent. After the intervention, medications are required to reduce the risk of stent thrombosis.
- Coronary artery bypass surgery is a heart operation that allows you to restore blood flow in the arteries of the heart by creating bypass blood flow paths - shunts. The operation can be performed either with artificial circulation (with cardiac arrest) or on a beating heart (without stopping). In the classic version, CABG is performed through a median sternotomy, which is access to the heart through the sternum. However, in some cases it is also possible to use alternative approaches to preserve the integrity of the sternum and reduce the invasiveness of the operation. In this case, a small incision is made on the side wall of the chest and with the help of special surgical instruments the required coronary arteries are bypassed. The decision to choose a method of surgical intervention remains with the surgeon, who takes into account all the functional and anatomical features of the patient.
During coronary artery bypass surgery, the patient's own arteries and veins are used as shunts (conduits). The internal mammary artery is traditionally used to bypass the anterior interventricular artery (the “main” artery of the heart). Also, arteries from the arms (radial arteries), veins of the lower extremities (superficial veins of the thigh), etc. are used as conduits. The number of applied conduits depends on the number of affected coronary arteries requiring bypass surgery.
A special group of patients with coronary artery disease consists of patients with concomitant damage to the heart valves, rhythm disturbances and damage to other arterial systems (arteries supplying the brain; abdominal aorta; arteries of the lower extremities). This is the most severe group of patients because in addition to surgical treatment of coronary artery disease, they require surgical treatment of concomitant cardiac or vascular pathology. Depending on the clinical condition of the patient, the degree of damage to the structures of the heart and various vascular beds, different tactics of surgical treatment can be used - simultaneous intervention (several operations are performed during one surgical intervention); staged treatment (operations are performed sequentially with intervals between stages). Recently, hybrid interventions have been used in clinical practice, combining standard surgery and angioplasty with stenting.
The choice of treatment tactics (angioplasty with stenting or coronary bypass surgery; staged or one-stage surgery) is determined by the cardiac team (cardiologist, cardiovascular surgeon, x-ray endovascular surgeon, anesthesiologist and other specialists) based on an assessment of the condition of each individual patient, the characteristics of the damage to his coronary arteries (using SyntaxScore I and II) and the presence of other concomitant pathology. In some patients, angioplasty with stenting has advantages (for example, with single-vessel lesions); in other patients, on the contrary, coronary artery bypass grafting is more effective (for example, with multi-vessel lesions of the coronary arteries in a patient with diabetes mellitus).
Mortality (mortality) from CABG depends on the severity of the patient’s condition and the presence of concomitant pathologies, which together determine the risk of the operation. The risk level is determined initially for each patient using the EUROScore-2 scale. Thus, for a “standard” patient without significant concomitant diseases, the predicted mortality from CABG surgery in the world ranges from 1 to 3%. However, this figure may increase depending on the severity of the condition.
NMITs SSH im. A.N. Bakuleva of the Ministry of Health of the Russian Federation has unique experience in performing all kinds of heart surgeries. Thus, the first coronary bypass operation at the National Medical Research Center for Cardiovascular Surgery named after. A.N. Bakulev Ministry of Health of the Russian Federation was carried out in 1970 by prof. Pokrovsky A.V. Since then, tens of thousands of patients have passed through the hands of our Center’s doctors.
To date, at the National Medical Research Center of Sports Sciences named after. A.N. Bakulev Ministry of Health of the Russian Federation performs about 1,800 coronary bypass operations per year (the largest number of operations among clinics in the Russian Federation) and about 1,700 angioplasties with stenting. The Center performs all types of surgical interventions for ischemic heart disease existing in the world: coronary artery bypass grafting on a beating heart and with artificial circulation; repeat coronary bypass surgery; multiple coronary bypass grafting through alternative mini-approaches (without median sternotomy); coronary bypass surgery with the simultaneous use of laser revascularization of the myocardium (for patients with poor distal coronary arteries); coronary bypass surgery in patients with low contractility of the myocardium of the left ventricle of the heart, including in combination with resection of a left ventricular aneurysm; combined coronary artery bypass surgery with reconstructive operations on heart valves and other arterial systems, in combination with cardiac arrhythmias; endovascular interventions on coronary and peripheral arteries using drug-eluting stents.
A unique feature of the National Medical Research Center of Sports Sciences named after. A.N. Bakulev Ministry of Health of the Russian Federation is to perform intraoperative shuntography for all patients who have undergone coronary artery bypass surgery. This allows you to fully verify on the operating table that all applied shunts are working adequately. NMITs SSH im. A.N. Bakulev Ministry of Health of the Russian Federation is the only center in the world where such “quality control” is applied. In this regard, the percentage of postoperative complications corresponds to the global indicators of the world's leading clinics specializing in such operations.
How is diagnosis carried out by a cardiologist-arrhythmologist?
Diagnosis of diseases treated by a cardiologist-arrhythmologist is usually carried out using the following tests and studies:
- ECG - atropine tests;
- Phonocardiography;
- ECG;
- ECG in a state of physical activity;
- ECG - monitoring for 24 hours;
- Ultrasound of the heart;
- General urine and blood tests;
- Diagnostics for atherosclerosis;
- Analyzes for the degree of development of cardiac risks, such as high cholesterol and others;
Types of heart pathology
Diseases can have a wide variety of causes and clinical forms. Several groups can be roughly defined:
- heart defects, vascular defects (congenital and acquired);
- inflammatory diseases (myocarditis, endocarditis, pericarditis);
- cardiac ischemia;
- dystrophic diseases of the heart muscle.
The pathology is so diverse that within a specialty such as cardiology, narrower specializations of doctors have emerged who deal with specific problems, for example , a cardiorheumatologist is a specialist in inflammatory diseases, a cardiac surgeon performs operations on the heart and blood vessels, which are necessary in the development of anatomical defects (malformations). , trauma) and impaired blood supply to the myocardium (ischemic disease).