Arrhythmia is diagnosed when the regularity of contractions of the heart muscle is disrupted. The most common type of arrhythmia is tachycardia, which can be caused in the ventricles of the heart (ventricular arrhythmia) or in the atria (supraventricular arrhythmia). What are the symptoms of arrhythmia? What is the removal procedure? Arrhythmia is not an isolated disease. This term describes a heart rhythm disorder that can cause the heart to beat too fast, too slow, or irregularly. In other words, the heart rhythm may be disrupted. An abnormal heart rhythm can be a symptom of cardiovascular disease (coronary heart disease, heart valve disease, hypertension) or the effect of disorders such as hormonal or electrolyte imbalances. Therefore, the patient needs to find out the causes of the arrhythmia and, if they require treatment, undergo appropriate therapy.
How does arrhythmia occur?
To understand the mechanism of arrhythmia, it is necessary to recall basic information about the structure and function of the heart in the body. This organ consists of two atria and two ventricles, which contract and relax in a strictly defined rhythm. Thanks to these movements, blood is constantly pumped into every cell of the body, providing it with nutrients and oxygen. But what makes the heart beat so regularly? The heart is equipped with a natural "pacemaker", that is, the sinus node, located in the right atrium. It is thanks to him that the heart “beats” even when it is removed from the chest. The sinus node produces electrical impulses that move the entire muscle. The work of the heart is a series of complex bioelectrical processes that occur in each of its cells. Cardiac arrhythmias occur when abnormalities occur at some point in this complex process. The pulse source may fail or problems may arise at the conduction stage. In both cases, arrhythmia will occur.
Prevention
- Elimination of cardiac pathology.
- Exclusion of extracardiac factors of arrhythmia or blockade (intoxication, autonomic dysfunction, stress, etc.).
- Limit intake of caffeine-containing products and alcohol.
We will help make a diagnosis at an early stage of the development of blockade, tachycardia or other disorders and provide timely treatment for cardiac arrhythmia. Further observation will allow maintaining a good quality of life. For questions regarding the treatment of cardiac arrhythmia in Moscow, please contact us by dialing the number +7.
Types of arrhythmias
There are many types of arrhythmias, as well as divisions in medicine depending on the accepted classifications. The most common forms of cardiac arrhythmia include:
- sinus tachycardia,
- bradycardia,
- atrial fibrillation,
- ventricular fibrillation,
- additional supraventricular and ventricular contractions,
- tachycardia: supraventricular and ventricular.
Each of these disorders is actually a separate disease that has different causes and also requires different treatments.
REASONS FOR THE DEVELOPMENT OF PAROXYSMAL VENTRICULAR TACHYCARDIA
Reasons for the development of PVT:
1. severe diseases of the cardiovascular system:
- myocardial infarction
- cardiomyopathy
- heart defects
- heart failure
- myocarditis (severe)
2. toxic factors:
- frequent alcohol consumption in significant quantities
- inhalation of glue fumes
- narcotic substances
3. cardiac injury
4. medications: cardiac glycosides, antidepressants, flecainide, fluoroquinolones
5. congenital anomalies of the cardiac conduction system (Brugada syndrome)
6. idiopathic VT – the cause of development is unclear
Symptoms of arrhythmia
The most common symptoms of arrhythmia include:
- fast or irregular heartbeat,
- tachycardia,
- bradycardia,
- strong heartbeat,
- feeling of lumps in the chest,
- dyspnea,
- chest pain,
- heat,
- weakness,
- fainting.
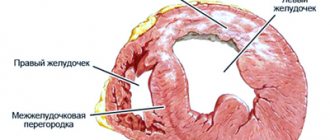
Ventricular arrhythmia
Ventricular arrhythmia is one of the most common. Their classification includes: ventricular tachycardia, flutter and ventricular fibrillation and accelerated ventricular rhythm. The older the patient and the more damaged the heart, the more often they occur.
Ventricular Arrhythmia - Cardiac Factors Factors that cause or exacerbate ventricular arrhythmia can be classified as cardiac or non-cardiac. When this type of arrhythmia occurs, the following cardiac factors are especially likely:
- cardiac ischemia,
- cardiomyopathy,
- congenital long QT syndrome,
- Brugada syndrome,
- mitral valve prolapse.
Ventricular arrhythmia - non-cardiac factors Non-cardiac factors include disorders such as:
- polymyositis,
- sarcoidosis,
- amyloidosis,
- diseases of the nervous system,
- hormonal disorders,
- metabolic disorders,
- electrolyte disturbances.
In addition, the condition is affected by the use of stimulants (coffee, smoking, alcohol).
What are the symptoms of ventricular arrhythmia?
Symptoms of ventricular arrhythmia depend on the type of arrhythmia. In mild forms, patients may not experience arrhythmias. Palpitations may be accompanied by chest discomfort and anxiety. In complex disorders (ventricular tachycardia, ventricular flutter, ventricular fibrillation), shortness of breath, loss of consciousness and sudden cardiac arrest occur.
Clinical case
A 56-year-old patient called the emergency medical team.
Complaints: headache and chest discomfort. This state lasts several hours before the call. There is a history of hypertension, but the patient does not undergo regular treatment. Sometimes, when blood pressure rises above 200/120, she takes Captopril at a dose of 25-50 mg. Before the complaints arose, I consumed about 1 liter of wine. According to him, he periodically abuses alcoholic beverages. At the time of inspection, productive contact is available. Skin, breathing, abdomen - without any features. Cardiac activity is rhythmic, tones are muffled. BP 160/90, heart rate=Ps 90 per minute. The abdomen is soft and painless. The “tapping” symptom is negative on both sides. Physiological functions are normal. The patient's ECG is presented below:
During the recording of the tape, the patient stated that she began to feel very bad and dizzy. The ECG shows pirouette tachycardia, which immediately turned into large-wave atrial fibrillation.
The patient's condition is extremely serious: clinical death was diagnosed. Pulse and pressure are not determined. Our team immediately moved the patient to a hard surface (floor) with resuscitation measures: mechanical ventilation, chest compressions, administration of Atropine, Adrenaline, magnesia; Two defibrillations were performed. Peripheral vein catheterization and hospitalization to the cardiac intensive care unit are provided directly, bypassing the emergency room. At the time of admission to the hospital, the patient was conscious and had no complaints. BP 130/90, heart rate=Ps 90 beats per minute. Breathing on your own.
What tests should be taken for ventricular arrhythmia?
To correctly identify ventricular arrhythmia and accurately differentiate the type of ventricular arrhythmia, it is necessary to perform an ECG. If arrhythmia occurs intermittently, perform a Holter test (24-hour ECG recording). You can also monitor your heart rate for longer, such as three days or even 2-3 weeks. In this case, it is necessary to wear an Event-Holter device, which the patient activates only when symptoms appear, such as:
- cardiopalmus,
- deterioration of health,
- dizziness.
An invasive electrophysiological study is performed when the site of ventricular arrhythmia is identified and an attempt is made to destroy the arrhythmogenic focus. The following methods are used in the treatment of ventricular arrhythmias:
- antiarrhythmic drugs,
- percutaneous high-frequency ablation,
- implantation of a cardioverter-defibrillator.
The doctor decides what treatment to take when he determines what type of ventricular arrhythmia the patient has.
Treatment of rhythm and conduction disorders at the prehospital stage
Acute arrhythmias and blockades, which can complicate the course of diseases of the cardiovascular system - ischemic heart disease (including myocardial infarction, post-infarction cardiosclerosis), rheumatic heart defects, primary and secondary cardiomyopathies, sometimes develop as a result of congenital abnormalities of the conduction system (Wolf-Parkinson-White syndromes - WPW , Launa-Genong-Levaina - LGL). Arrhythmias often occur against the background of arterial hypertension, congestive heart failure, and electrolyte disorders (for example, hypokalemia, hypomagnesemia). Their appearance can be triggered by taking medications (cardiac glycosides, theophylline; drugs that prolong the QT interval - terfenadine, cisapride), alcohol, as well as excessive consumption of caffeine-containing drinks.
At the prehospital stage, it is advisable to identify those rhythm disturbances for which emergency therapy is indicated (see table).
Paroxysmal supraventricular tachycardia
Medical tactics for paroxysmal supraventricular tachycardia (PSVT) are determined by the patient’s hemodynamic stability. A drop in blood pressure (BP) with the development of syncope, an attack of cardiac asthma, pulmonary edema, and the development of a severe anginal attack against the background of tachycardia are indications for immediate electrical pulse therapy.
With relatively stable hemodynamics, the choice of drug depends on the electrocardiographic picture (Fig. 1).
Tachycardia with “narrow” QRS complexes (unchanged QRS no more than 0.1 s) is stopped by administration of the calcium antagonist verapamil (isoptin), which lengthens the refractory period in the atrioventricular node. The drug is administered intravenously as a bolus at a dose of 2.5-5 mg over 2-4 minutes (to avoid the development of collapse or severe bradycardia) with possible repeated administration of 5-10 mg after 15-30 minutes if tachycardia persists and there is no hypotension.
Side effects of verapamil include: bradycardia (up to asystole with rapid intravenous administration due to suppression of the automatism of the sinus node); AV blockade (up to complete transverse with rapid intravenous administration); transient ventricular extrasystole (self-limited); arterial hypotension due to peripheral vasodilation and negative inotropic effects (up to collapse with rapid intravenous administration); increase or appearance of signs of heart failure (due to negative inotropic effects); pulmonary edema. From the central nervous system, dizziness, headache, nervousness, lethargy, facial redness, peripheral edema, feeling of lack of air, shortness of breath, allergic reactions are noted.
Verapamil should only be used for disorders of the QRS complex. In case of a “wide” QRS complex and suspected Wolff-Parkinson-White syndrome (WPW syndrome), the drug is contraindicated, as it shortens the refractory period of additional conduction pathways and can cause an increase in heart rate and ventricular fibrillation. Diagnosis of WPW syndrome is possible with appropriate anamnestic indications and/or by evaluating previous ECGs with sinus rhythm (PQ interval less than 0.12 s, QRS complex widened, delta wave detected). Other contraindications to the use of verapamil are:
- absolute: severe bradycardia, sick sinus syndrome, AV block II and III degrees, cardiogenic shock, chronic and acute heart failure, hypersensitivity to the drug;
- relative: bradycardia with a heart rate less than 50 per minute, AV block of the first degree, ventricular tachycardia, arterial hypotension (SBP less than 90 mm Hg).
In addition, verapamil is contraindicated in patients who have used any beta-blocker within the last two hours.
An alternative to verapamil is procainamide (procainamide); it can also be used in case of ineffectiveness of verapamil, but not earlier than 15 minutes after the administration of the latter and provided that stable hemodynamics are maintained. Procainamide is effective for reciprocal tachycardia in patients with WPW syndrome (in cases where verapamil is contraindicated). Procainamide is administered intravenously slowly at a dose of 1000 mg over 8-10 minutes (10 ml of a 10% solution, adjusted to 20 ml with isotonic sodium chloride solution) with constant monitoring of blood pressure, heart rate and ECG (in case of sharp expansion of QRS complexes, administration must be stopped). When sinus rhythm is restored, the drug administration is stopped. Due to the possibility of lowering blood pressure when administering procainamide, the patient should be in a horizontal position; it is also necessary to prepare a syringe with 0.1 mg of phenylephrine (mesatone).
Side effects of procainamide include arrhythmogenic effects, ventricular arrhythmias due to prolongation of the QT interval, slowing of atrioventricular and intraventricular conduction, arterial hypotension, dizziness, weakness, disturbances of consciousness, depression, delirium, hallucinations, allergic reactions.
Contraindications to the use of procainamide are arterial hypotension, cardiogenic shock, chronic heart failure, sinoatrial and AV blockades of the second and third degrees, intraventricular conduction disorders, prolongation of the QT interval and indications of episodes of torsade de pointes in the anamnesis, severe renal failure, systemic lupus erythematosus , hypersensitivity to the drug. The toxic effect of novocainamide is eliminated by intravenous injection of 100 ml of 5% sodium bicarbonate solution.
It is also possible to use beta-blockers (propranolol) and cardiac glycosides (digoxin), but their effectiveness in paroxysmal supraventricular tachycardia is only 40-55%. If the patient has already been administered verapamil, then propranolol (obzidan, anaprilin) can be used no earlier than 30 minutes sublingually at a dose of 10-20 mg. The drug is contraindicated in cases of arterial hypotension and bronchial obstruction syndrome. IV administration of propranolol in a dose of up to 0.15 mg/kg at a rate of no more than 1 mg/min should preferably be carried out under the control of an ECG monitor in a cardiac block. Propranolol is highly effective for paroxysmal tachycardia caused by a re-entry circle in the sinus or atrioventricular node; in other types of tachycardia, its use can reduce heart rate. Digoxin in an initial dose of 0.25-0.5 mg is effective for nodal reciprocal tachycardia, in other cases it only reduces heart rate. Digoxin is not indicated for WPW syndrome for the same reasons as verapamil.
Therapy of paroxysmal supraventricular tachycardia in a specialized cardiac intensive care unit and in a hospital can be carried out by intravenous administration of ATP (or adenosine), interrupting the circle of “re-entry”: 10 mg (1 ml of 1% solution) ATP is administered intravenously over 5 -10 s, if there is no effect, another 20 mg (2 ml of 1% solution) is reintroduced after 2-3 minutes. When using adenosine (adenocor), the initial dose is 3 mg (1 ml). The effectiveness of the drug for this type of rhythm disturbance is 90-100%. As a rule, it is possible to stop paroxysmal supraventricular tachycardia within 20-40 s after ATP administration.
IV administration of adenosine also makes it possible to differentiate between atrial flutter with 1:1 conduction and supraventricular tachycardia; inhibition of AV conduction makes it possible to identify characteristic flutter waves, but the rhythm is not restored.
Contraindications to the use of the drug are AV block of the second and third degree, sick sinus syndrome (in the absence of an artificial pacemaker), increased sensitivity to adenosine. It should also be taken into account that the administration of ATP or adenosine can provoke an attack in patients with bronchial asthma.
It must be taken into account that intravenous administration of a bolus of adenosine (ATP) during supraventricular paroxysms in approximately 50% of cases leads to 5-15 second asystole, and in 0.2-3% of cases asystole can last for more than 15 s, which can require a precordial blow and even chest compressions (only a few massage movements are required). Due to the risk of developing such complications, the use of adenosine (ATP) is permissible only in a specialized intensive care unit or in a hospital.
Atrial fibrillation and flutter
When treating patients with atrial fibrillation and flutter at the prehospital stage, the feasibility of restoring sinus rhythm should be assessed.
The absolute indication for restoration of sinus rhythm during the development of paroxysm of atrial fibrillation is the development of pulmonary edema or arrhythmogenic shock; in this case, emergency cardioversion should be performed prehospital.
Contraindications to the restoration of sinus rhythm at the prehospital stage include the duration of paroxysm of atrial fibrillation for more than two days, proven dilatation of the left atrium (antero-posterior size 4.5 cm, according to echocardiography), the presence of blood clots in the atria or a history of thromboembolic complications, the development of paroxysm on background of acute coronary syndrome (in the presence of stable hemodynamics), development of paroxysm against the background of severe electrolyte disturbances, decompensation of thyrotoxicosis. If you refuse to restore sinus rhythm, it is necessary to establish control over the heart rate in order to maintain it within 60-90 beats per minute.
The drug of choice for controlling heart rate is cardiac glycosides: 0.25 mg of digoxin (1 ml of 0.025% solution) in 20 ml of isotonic sodium chloride solution is administered intravenously as a slow bolus. Further tactics are determined in the hospital. A permanent normosystolic form of atrial fibrillation without signs of heart failure does not require antiarrhythmic therapy at all (Fig. 2). Side effects of digoxin (manifestations of digitalis intoxication) - bradycardia, AV block, atrial tachycardia, ventricular extrasystole, anorexia, nausea, vomiting, diarrhea, headache, dizziness, blurred vision, syncope, agitation, euphoria, drowsiness, depression, sleep disturbances , confusion.
Contraindications to the use of digoxin:
- absolute: glycoside intoxication, hypersensitivity to the drug;
- relative: severe bradycardia (negative chronotropic effect); AV blockade of II and III degrees (negative dromotropic effect); isolated mitral stenosis and normo- or bradycardia (danger of dilatation of the left atrium with worsening left ventricular failure due to increased pressure in its cavity; risk of developing pulmonary edema due to increased contractile activity of the right ventricle and increased pulmonary hypertension); idiopathic hypertrophic subaortic stenosis (possibility of increasing obstruction of the left ventricular outlet due to reduction of the hypertrophied interventricular septum); unstable angina and acute myocardial infarction (the danger of increasing myocardial oxygen demand, as well as the possibility of myocardial rupture during transmural myocardial infarction due to increased pressure in the cavity of the left ventricle); WPW syndrome (improves conduction along accessory pathways), frequent or polytopic ventricular extrasystole, jogging ventricular tachycardia.
The drug of choice for restoring sinus rhythm in stable hemodynamics is procainamide.
In some cases, verapamil can serve as an alternative to procainamide. It does not always restore sinus rhythm, but effectively reduces heart rate by blocking the atrioventricular node. We must not, however, forget that for atrial fibrillation in patients with WPW syndrome, the use of verapamil is not indicated (the drug improves conduction along additional pathways).
In case of magnesium-dependent atrial fibrillation (proven hypomagnesemia or the presence of a prolonged QT interval), the drug of choice is magnesium sulfate (cormagnesin), which in other cases is an additional agent for slowing down (reducing the frequency of contractions) the rhythm.
If one antiarrhythmic drug is ineffective, drug therapy at the prehospital stage is stopped; in case of complications (see above), electrical pulse therapy is performed.
Atrial flutter with low atrioventricular conduction leading to mild tachycardia, and in the absence of complications, does not require emergency treatment.
In case of unstable hemodynamics, the development of complications due to atrial flutter with a high heart rate (AV conduction 1:1), emergency electropulse therapy is indicated.
Uncomplicated atrial flutter with a high ventricular rate in the prehospital phase requires only slowing the heart rate, for which digoxin or verapamil is used. The use of beta-blockers in this case is least advisable, although possible.
Ventricular arrhythmias
In most cases, both ventricular and supraventricular extrasystole are not “malignant” rhythm disturbances and do not require immediate therapeutic intervention (the exception is frequent and/or polytopic ventricular extrasystole during myocardial infarction). In this case, oral beta blockers may be an option. From today's perspective, it is optimal to prescribe selective drugs with lipophilic properties. The most studied drug in this group is metoprolol, the use of which in a daily dose of 50–200 mg (in two doses) is recommended primarily for patients in whom extrasystole is a manifestation of coronary artery disease and/or accompanies arterial hypertension.
In acute myocardial infarction, the drug of choice for stopping ventricular arrhythmias is lidocaine (Fig. 3).
In conditions of stable hemodynamics, the drug of choice for stopping ventricular tachycardia (VT) is lidocaine, administered intravenously as a bolus at a dose of 1-2 mg/kg (80-100 mg) over 3-5 minutes, followed by a maintenance drip infusion for up to 24 minutes. 36 hours at a rate of 20-55 mcg/kg/min (maximum 4 mg/min). If necessary, during the infusion, an additional jet injection of lidocaine at a dose of 40 mg is acceptable 10-30 minutes after the first bolus. Prolongation of the QT interval and increase in its dispersion are indications for intensifying maintenance therapy by drip administration of cormagnesin (magnesium sulfate) at a rate of 3-20 mg/min. In the future, it is possible to switch to prophylactic intramuscular administration of lidocaine at a dose of 2-4 mg/kg (160-200 mg, maximum 600 mg, and in case of myocardial infarction no more than 300 mg) every 4-6 hours.
If lidocaine is ineffective, the use of other antiarrhythmics to stop VT is indicated if stable hemodynamics are maintained and there are no adverse reactions (risk of collapse and potentiation of the arrhythmogenic effect of antiarrhythmic drugs) or when electrical pulse therapy is impossible. In these cases, the second most important drug is procainamide (procainamide), administered with appropriate precautions intravenously in fractional doses of 100 mg/5 min until sinus rhythm is restored or a saturating dose is reached (500-1000 mg).
The effectiveness of procainamide in all paroxysmal tachycardias makes it the drug of choice for the treatment of tachycardia of unknown origin with a wide QRS complex (ventricular or supraventricular with conduction aberration).
The drug of choice for ventricular tachycardia of the “pirouette” type and an additional drug for other types of ventricular tachycardia (including those refractory to therapy with lidocaine and procainamide) is magnesium sulfate (cormagnesin), administered intravenously over 10-15 minutes at a dose of 400-800 mg of magnesium (20-40 ml of 10% or 10-20 ml of 20% solution). If there is no effect, the drug is re-administered after 30 minutes. Once the effect is achieved, maintenance therapy consists of drip administration of cormagnesin (magnesium sulfate) at a rate of 3-20 mg/min for 2-5 hours.
Ventricular tachycardia with unstable hemodynamics requires immediate electrical impulse therapy (Fig. 4).
Bradyarrhythmias
Bradyarrhythmias (sinus bradycardia, sinoauricular block, slow atrioventricular replacement rhythm, atrioventricular conduction disturbances of degree II and III) require treatment in cases where these conditions are accompanied by unstable hemodynamics and arise as a complication of organic heart damage or develop during resuscitation measures, as well as during the appearance of frequent attacks of Morgagni-Edams-Stokes. To restore hemodynamics, it may be sufficient to increase the heart rate intravenously by administering a 0.1% solution of atropine sulfate in a dose of 0.3-1.0 ml, repeating the initial dose (if effective) after 4-5 hours.
Side effects of atropine include dry mouth, thirst, nausea, vomiting, intestinal atony and constipation, increased cough in patients with bronchial asthma, urination disorders, mydriasis, photophobia, paralysis of accommodation, tachycardia, anxiety, tremor, headache, psychomotor agitation.
Contraindications to the use of atropine are glaucoma, chronic urinary retention, intestinal atony, tachycardia, severe heart failure, severe atherosclerosis, and hypersensitivity to the drug. For bradyarrhythmias and AV blockades, it is permissible to use atropine for vital indications, even in case of myocardial ischemia, intestinal obstruction, intestinal atony, liver and kidney diseases, and angle-closure glaucoma.
The ineffectiveness of atropine therapy is an indication for temporary cardiac pacing, and if it is impossible for health reasons, orciprenaline is used (at a dose of 10-30 mcg/min under heart rate control, intravenous drip until a therapeutic effect appears).
O. B. Talibov, Candidate of Medical Sciences A. V. Topolyansky, Candidate of Medical Sciences
Supraventricular arrhythmia
Atrial fibrillation and atrial flutter is one of the types of supraventricular arrhythmia. The most common symptoms include rapid heartbeat, shortness of breath, and even fainting. The best results are achieved by combining pharmacological treatment with diagnostic procedures. Supraventricular cardiac rhythm disturbances are caused by electrical impulses originating in the sinus node or atrioventricular focus.
Supraventricular arrhythmia - types
Supraventricular arrhythmias include:
- additional, single stimulation,
- supraventricular tachycardia,
- pre-excitation syndromes,
- atrial tachycardia,
- atrial fibrillation,
- atrial flutter,
- sinus tachyarrhythmias.
Supraventricular arrhythmia - symptoms
Each of the arrhythmias listed above has different causes and symptoms. Each of them is treated differently. First of all, it is necessary to determine what diseases cause supraventricular arrhythmia, what symptoms accompany it, what is the patient's prognosis and how to treat it. Symptoms that are typical of supraventricular arrhythmia include:
- cardiopalmus,
- fatigue,
- dyspnea,
- fainting,
- dizziness,
- chest discomfort.
There are often no symptoms with supraventricular accessory beats.
Consequences and complications
In the absence of timely treatment, arrhythmias and heart block provoke attacks of angina, pulmonary edema, and thromboembolism. Acute heart failure and even cardiac arrest are possible. According to statistics, in 10-15% of cases, blockades and other types of arrhythmia lead to death. Pathological tachycardia can provoke myocardial infarction. Complete atrioventricular block or asystole can provoke loss of consciousness, which is associated with a decrease in blood supply to the brain. Every sixth case of thromboembolic complications of atrial fibrillation leads to stroke. For arrhythmias caused by different causes, treatment is selected individually.
Treatment of supraventricular arrhythmias
First of all, it is important to have a detailed history of not only heart disease, but also general, rheumatological, metabolic and endocrine diseases. This usually starts with non-invasive tests such as: morphology, ECG, cardiac ECHO and Holter study. If necessary, invasive and complex tests such as electrophysiological studies are performed. Supraventricular arrhythmias are usually treated with medications. When this doesn't work, you can introduce ablation, for example. These two treatments can also effectively complement each other.
The article is for informational purposes only, self-medication is not acceptable. Be sure to consult with your healthcare provider.
Diagnostics
The primary stage of diagnosing arrhythmia and heart block is carried out by a therapist or cardiologist. Based on the patient’s complaints and examination results, the following examinations may be prescribed:
- electrocardiography (including 24-hour Holter monitoring);
- transesophageal/intracardiac electrophysiological study;
- treadmill test (diagnosis of arrhythmias with imitation of conditions causing blockade or other disorders).
If necessary, the doctor prescribes auxiliary diagnostic studies and tests. The accuracy of the results affects the effectiveness of treatment of the blockade or arrhythmia.