Myocardial infarction is an extremely dangerous condition, often leading to serious complications and death of the patient. Older people are especially at risk of developing it. The likelihood of a successful outcome directly depends on the speed of medical care. Patients with myocardial infarction require round-the-clock care during the acute period and long-term rehabilitation after discharge from the hospital. It is advisable that all this time the patient be under the supervision of a specialist with a medical education. The patient's relatives have to combine caring for him with work, family affairs, and personal needs. Because of this, the quality of care decreases and the risks of complications increase. The help of professional nurses in a hospital or rehabilitation center can solve this problem. Proper care after a heart attack speeds up the patient's return to normal life.
Who is at risk?
Myocardial infarction develops in people with coronary heart disease, which most often affects older people, especially men. Narrowing or blockage of the coronary arteries leads to impaired circulation and necrosis of areas of the myocardium.
The risk of heart attack is higher in patients:
- with a hereditary predisposition;
- diabetes mellitus;
- overweight;
- arterial hypertension;
- rheumatic carditis;
- bad habits (including passive smoking);
- atherosclerosis;
- inflammatory bowel diseases;
- exposed to frequent and prolonged stress.
The likelihood of relapse is especially high in people who have already had a myocardial infarction. It is advisable for an at-risk patient with coronary artery disease to be cared for by an experienced caregiver, for example in a nursing home. She will be able to recognize the signs of myocardial infarction in time, provide proper first aid and organize care after the attack.
Features of nursing care and monitoring of patients with myocardial infarction in a hospital
author: Guseva Maria Igorevna
Student of the specialty Nursing, Zh-32
Head: Maya Sergeevna Agadzhanova Teacher, State Budgetary Educational Institution “Krasnodar Regional Basic Medical College” Ministry of Health of the Krasnodar Territory
Features of nursing care and monitoring of patients with myocardial infarction in a hospital
FEATURES OF NURSING CARE AND MONITORING OF PATIENTS WITH MYOCARDIAL INFARCTION IN A HOSPITAL
Author of the work:
Guseva Maria, S/d Zh-32 gr.
Scientific adviser:
Agadzhanova Maya Sergeevna – State Budgetary Educational Institution “Krasnodar Regional Basic Medical College” of the Ministry of Health of the Krasnodar Territory
Cardiovascular diseases have long occupied first place in the structure of morbidity and mortality in the world - more than 17 million people die every year. Myocardial infarction is one of the most common clinical forms of coronary heart disease, which is the most common cause of sudden death. Myocardial infarction affects more than 1 million people worldwide every year. MI usually occurs at a young age (35-50 years) and is observed in men more often than in women. These factors determine the need for timely treatment and professional care for patients with myocardial infarction in a hospital. And the nurse plays a big role in this. Therefore, studying the characteristics of nursing care and monitoring of patients with myocardial infarction in a hospital is a relevant topic.
Field of study:
myocardial infarction.
Object of study:
Features of nursing care and monitoring of patients with myocardial infarction.
Subject of study:
regulatory documentation, job descriptions, statistical data on the incidence of myocardial infarction in the Russian Federation and the Krasnodar region, outpatient records, results of surveys of patients and nurses.
Research hypothesis:
The care and observation of a nurse during myocardial infarction will prevent complications and significantly improve the quality of life of patients with this disease.
Goal of the work:
analysis of the role of the nurse in working with patients with myocardial infarction in a hospital setting.
Research objectives:
- Analyze regulatory documentation and literature on the research topic.
- To consolidate, expand, systematize and deepen knowledge about the role of the nurse in organizing and providing nursing care and observation during myocardial infarction, confirm the mastery of the type of activity of general and professional competencies in accordance with the Federal State Educational Standard for Secondary Professional Education in the specialty 34.02.01. "Nursing"
- Perform an analysis of statistical data on the prevalence of myocardial infarction in the Russian Federation and the Krasnodar Territory.
- Identify and rank factors for the development of myocardial infarction.
- Develop materials for the health education work of nurses.
Research methods:
- method of theoretical analysis of literary sources and normative documentation;
- method of sociological survey (questioning);
- method of scientific research (analysis of the medical history of inpatients);
- observation method (analysis, synthesis, comparison);
- method of scientific modeling (drawing up a memo);
- statistical method (calculation of percentages).
During the study, an analysis of medical documentation and questioning of patients undergoing inpatient treatment in the cardiology department at the State Budgetary Healthcare Institution “KKB No. 2” in Krasnodar was carried out. A survey of 20 patients with myocardial infarction was completed. Among patients with myocardial infarction, 5 people are women (25%), 15 are men (75%). Most patients are in older age groups, aged 60-65 years.
The results of the survey showed that males suffer from myocardial infarction 3 times more often than women. This indicator may be due to the high prevalence of bad habits among men. Among patients with myocardial infarction in the cardiology department, more than half are elderly. This proves that the risk of developing the disease increases with age.
30% of the surveyed patients had a recurrent myocardial infarction, the rest had a primary one.
19 (95%) patients with a history of myocardial infarction had arterial hypertension (90%); 13 of them also suffer from atherosclerosis (65%), 11 patients have diabetes mellitus (55%), 2 patients have a history of rheumatic heart disease (10%).
Diseases such as arterial hypertension and atherosclerosis are the main risk factors for cardiovascular diseases, including myocardial infarction.
Analysis of medical records showed that 10 (50%) patients with myocardial infarction were taken to the hospital in the first 4 hours from the onset of the disease, 6 (30%) patients in the interval from 4 to 12 hours. The remaining patients were delivered within 12-24 hours. Early hospitalization of patients allows for timely treatment of the disease, which will avoid complications in the future.
Percutaneous transluminal coronary angioplasty was performed in 16 patients; recanalization of chronic coronary artery occlusions using a retrograde method was performed in 1 patient.
Every year, more and more new methods are used in the treatment of cardiovascular diseases. Currently, PTCA and recanalization are common surgical procedures with a low risk of complications.
In total, among the surveyed patients, 6 people are in serious condition on strict bed rest (30%). 4 patients (20%) developed complications of myocardial infarction such as disturbances in the rhythm and conduction of the heart (cardiac arrhythmia). 1 patient (5%) had chronic heart failure. Complications of myocardial infarction in the form of speech disorders—aphasia—developed in 5 patients (25%). Motor aphasia was detected in 3 patients, sensory aphasia in 1, and amnestic aphasia in one more patient.
85% of respondents (17 patients) are aware of possible complications after a myocardial infarction, 10 patients (50%) of them believe that the causes of complications are non-compliance with the prescriptions of medical personnel. 3 patients (15%) are inclined towards unhealthy diet. And 4 patients (20%) answered that the main causes of complications are stressful situations.
Most of the respondents know about the possible causes of complications of myocardial infarction. Prevention of complications allows you to reduce the risk of their occurrence by 2 times.
Most of the surveyed patients receive information about their disease from medical workers (60% - 12 patients). 5 patients trust the media (25%), 3 patients prefer to read leaflets and health bulletins (15%).
More than 50% of patients trust information received from medical professionals, which obliges medical personnel to present information competently and as accessible as possible.
During the study, a reminder was developed for patients with myocardial infarction to prevent complications and recurrent heart attacks.
Conclusions:
- The results of a patient survey showed that myocardial infarction affects mainly elderly people, in 75% of cases men.
- Of the 20 patients, 90% of cases have a history of arterial hypertension, of which 65% suffer from atherosclerosis, 55% from diabetes mellitus.
- 50% of patients were delivered within the first 4 hours, and percutaneous transluminal coronary angioplasty was performed in 80% of cases.
- Among those surveyed, 30% of patients were in serious condition; 20% developed complications of myocardial infarction such as cardiac rhythm and conduction disturbances.
- 85% of respondents were aware of possible complications after a myocardial infarction.
- 60% of patients with myocardial infarction receive information about their disease from medical workers, 25% from the media, 15% from leaflets and health bulletins.
Practical significance of the work.
The developed memo for patients with myocardial infarction on the prevention of complications and recurrent heart attacks is used as handouts when a nurse performs sanitary educational work in the cardiology department of a hospital.
The received materials can be used in the educational process of a medical college when studying the specialty “Nursing” PM.02 “Participation in treatment, diagnostic and rehabilitation processes”, MDK 02.01 “Nursing care for various diseases and conditions” R.1 “Nursing care for various diseases and conditions of therapeutic patients.”
Features of nursing care and monitoring of patients with myocardial infarction in a hospital
Symptoms of the disease
The main symptom is acute chest pain that does not go away after taking nitroglycerin. It occurs suddenly and gets worse quickly. The attack may be accompanied by shortness of breath, cough, and arrhythmia. If the pain lasts more than 15 minutes, you must call an ambulance. The sooner the blood supply to the heart is restored, the smaller the size of the dead area will be.
In a third of patients, myocardial infarction occurs in an atypical form, which significantly complicates early diagnosis and leads to the loss of precious time. Experienced caregivers know about this and can predict the development of an attack based on indirect symptoms. Patients with diabetes may not feel pain. In women, it is often localized in the arm or neck and is accompanied by fatigue. Atypical forms of heart attack also appear:
- pain in the abdomen, throat, lower jaw;
- nausea;
- dizziness;
- confusion;
- cold sweat;
- swelling;
- a sharp decrease in blood pressure.
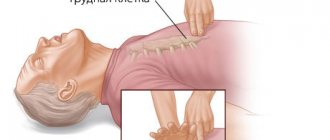
In many cases, the only symptom of a heart attack is sudden cardiac arrest. In such cases, only urgent resuscitation measures can save the patient.
A delay in treatment of myocardial infarction can cause complications such as:
- cardiogenic shock,
- acute and chronic heart failure,
- arrhythmia,
- arterial hypotension,
- heart aneurysm.
If you suspect an attack, the patient must first be seated and removed from constricting clothing. Then you need to measure his pressure, give crushed aspirin or nitroglycerin (for high blood pressure) and call an ambulance. The services of a nurse significantly increase the chances of patients undergoing surgical treatment. Regular care after a heart attack reduces the likelihood of a recurrence.
Stages of treatment and rehabilitation
| Period | Treatment methods | Features of care |
| Rehabilitation (up to 28 days) | The patient is transferred to the infarction department and then to a cardiology sanatorium. The patient is prescribed medications that normalize blood circulation and strengthen the heart muscle. | The nurse teaches the ward how to sit down and stand up correctly and helps restore self-care skills. |
| Rehabilitation (up to 28 days) | The patient is transferred to the infarction department and then to a cardiology sanatorium. The patient is prescribed medications that normalize blood circulation and strengthen the heart muscle. | The nurse teaches the ward how to sit down and stand up correctly and helps restore self-care skills. |
| Outpatient (up to 1 year) | The patient is seen by a doctor in a clinic or boarding house, takes medications to prevent a heart attack, and does physical therapy. | The caregiver’s task is to help the recovering person adjust his diet and daily routine to avoid a relapse. |
Rehabilitation of patients who have suffered an acute myocardial infarction affects all aspects of the patient's life. In addition to medication and physiotherapeutic treatment, it includes moderate physical activity and work with emotions.
Specifics of care in the acute period
This is the most important step in the treatment of myocardial infarction. Any physical activity, anxiety, or skipping medications can lead to irreversible consequences. Since the patient after a myocardial infarction must strictly adhere to bed rest, he finds himself completely helpless and needs round-the-clock care.
The nurse should:
- feed him and give him medicine on time,
- periodically measure blood pressure and pulse,
- maintain body hygiene,
- change underwear and bed linen,
- turn over several times a day to prevent bedsores and thrombosis,
- provide psychological support.
A patient with myocardial infarction is prescribed diet No. 10. It does not contain products that cause gas and limits salt intake. The patient receives food in small portions 5-6 times a day. The last dose should be at least 3 hours before bedtime.
To prevent diaper rash from occurring on the skin, the patient should be dressed in light but warm clothing that allows air to pass through and removes moisture from the body.
In the acute period, many patients are characterized by a strong fear of death, a hypochondriacal or hysterical reaction, which negatively affects health and prevents the body from recovering. If these conditions are not corrected in a timely manner, changes in the psyche can become entrenched in character. The nurse helps the patient cope with the fear of death, focuses his attention on improvements and positive prognoses, monitors the adequacy of reactions and immediately informs the doctor if the patient shows signs of psychosis.
Rehabilitation conditions for patients who have suffered a myocardial infarction
Bed rest in the acute period is due to the need to reduce the load on the heart muscle and reduce its need for oxygen. However, prolonged refusal to move increases the risk of congestion in the lungs and the formation of blood clots, impairs the functioning of the digestive system, and causes muscle weakness. To avoid this, the patient is given moderate physical activity as he recovers.
If the acute period passes without complications, the patient is allowed to sit down, stand up, and go to the toilet independently. The nurse helps perform movements smoothly, without sudden effort, and makes sure that the patient does not become ill. It measures your heart rate before and after physical activity. After about 2 weeks, short walks around the hospital grounds are allowed.
The transition from one activity level to the next is permitted after an intermediate diagnosis. The patient's blood pressure is measured, a cardiogram is taken, and individual exercise tolerance is checked. Light exercise should be done in bed before getting up to prepare the cardiovascular system after sleep for daytime activity.
After discharge from the hospital, the patient is recommended to undergo rehabilitation in a sanatorium or boarding house. Here a therapeutic diet is prepared for him, rich in potassium and maintaining a balance of proteins, fats, and carbohydrates. Benefits for the patient:
- lean meat,
- fish,
- fresh vegetables and fruits,
- whole grain cereals,
- eggs,
- greenery,
- cottage cheese,
- potato.
Upon admission to the rehabilitation department, the patient takes exercise tests. The results show the functioning of the cardiovascular and respiratory systems. Based on them, a system of exercises is developed in a gentle or training mode. The patient is recommended to engage in physical therapy 3-4 times a day with a gradual increase in load. The exercise therapy complex may include:
- general strengthening workout,
- balance exercises,
- exercises with ball and stick,
- walking at a calm and fast pace,
- swimming,
- exercise classes,
- breathing exercises.
The duration of classes is 10-25 minutes. At the rehabilitation stage, patients who have suffered a myocardial infarction no longer require physical care, but still need psychological support. Many of them do not adequately assess their capabilities and either avoid the required load or increase it excessively. The nurse’s task during this period is to monitor compliance with the recommended schedule of activities and rest, work with the negative emotions of the ward and help him adapt to normal life.
Associate Professor V. K. Milkamanovich
Belarusian State University
Myocardial infarction (MI) is a severe form of coronary heart disease (CHD), in fact, its dangerous complication. The danger of MI to life is emphasized by the unofficial synonym for the diagnosis - “cardiovascular accident”. This is necrosis (death) of one or more areas of the heart muscle as a result of an acute deficiency of its blood supply, which persists for more than 20 minutes (Fig. 1). Necrosis finally forms within 2–4 hours or more, depending on the collateral (bypass) blood flow and the sensitivity of cardiac muscle cells to decreased blood supply.
IHD is an independent heart disease that can manifest as MI, angina pectoris, post-infarction cardiosclerosis, cardiac arrhythmia, heart failure, and sudden death. The term “ischemia” (from the Latin ischemia - I delay, stop the blood) means a local deterioration in blood supply, most often caused by a narrowing or complete blockage of the lumen of the artery, leading to temporary dysfunction or permanent damage to the tissue or organ.
The main cause of IHD is atherosclerosis of the coronary arteries. Atherosclerosis (from the Greek athera - gruel and sclerosis - hardening) is a systemic chronic disease of large and medium-sized arteries, resulting from persistent chronic inflammation and dysfunction of the endothelium of the vascular wall, local accumulation of lipids in the area of inflammation, as well as blood components and compaction of the connective tissue tissue in its inner and middle layers.
Externally, an artery affected by atherosclerosis resembles a metal pipe corroded by rust. Throughout its entire internal surface, numerous atherosclerotic plaques of various shapes and sizes, clots of blood clots on the surface of atherosclerotic plaques, fatty spots and stripes, ulcerations, deposits of calcium salts (calcinosis), etc. are visible.
There are two phases in the development of the atherosclerotic process.
The first phase is atherogenic. The lipid plaque grows (up to about 40 years of age). Atherosclerotic plaques are accumulations of cholesterol endothelial cells - the inner lining of blood vessels, responsible for their elasticity. As it is deposited, cholesterol mixes with calcium to form dense plaques that increase in size and rise above the surface of the artery wall (Figure 2). Over time, this leads to blocking of the lumen of the vessel.
The second phase is thrombogenic. It is characterized by the presence of an atherosclerotic plaque, prone to the formation of thrombotic masses on its surface.
Under certain conditions (for example, a sudden increase in blood pressure), the morphological structure of the surface layers of the atherosclerotic plaque may be disrupted, and then the preconditions are created for a rapid disruption of blood flow in the coronary artery, which leads to a complete or partial cessation of blood supply to the area of the myocardium that this line supplies. Rupture of an atherosclerotic plaque and/or thrombus formation in the lumen of a coronary artery are the most common causes of MI.
Atherosclerosis is characterized by a slowly progressive cyclic course: periods of activity of the process are replaced by periods of calm.
The left coronary artery, having a diameter of 3.4–4.9 mm (usually 3.9), supplies blood to the bulk of the left ventricle, the left atrium, part of the anterior wall of the right ventricle, and the anterior part of the interventricular septum. Therefore, interruptions in the supply of cardiac muscle cells with oxygen during circulatory disorders in the left coronary artery lead to dystrophic, necrotic and sclerotic changes in large areas of the myocardium, clinically manifested by a decrease in myocardial contractility, chronic heart failure, detraining of the patient and psychological disorders.
Most often with MI, the left ventricle of the heart suffers. The right ventricle is very rarely affected in isolation.
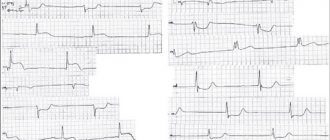
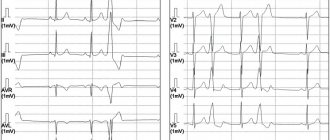
The diagnosis of “myocardial infarction” is established on the basis of characteristic complaints, objective clinical signs of heart damage, as well as electrocardiography, echocardiography and markers of myocardial necrosis.
The diagnostic problem of acute MI lies in the fact that in 50% of cases it develops suddenly, without any previous clinical symptoms, in a person in the prime of life, outwardly completely healthy and without bad habits.
Subjective clinical signs of myocardial infarction
Pain in the chest for more than 15–20 minutes, which spreads along the inner surface of the left arm with a tingling sensation in the wrist and fingers. Other possible areas of pain distribution (irradiation) are the shoulder girdle, neck, jaw, interscapular space (also mainly on the left).
The pain during a heart attack is very strong, perceived as dagger-like, tearing, burning, “a stake in the chest.” This feeling can be so unbearable that the person screams.
Sometimes the sensations may resemble an attack of angina pectoris, that is, instead of severe pain - discomfort in the chest, a feeling of strong compression, squeezing, a feeling of heaviness (“pulled with a hoop,” “squeezed in a vice,” “crushed with a heavy slab,” etc.).
Some people experience only a dull ache or numbness in the wrists combined with severe and prolonged chest pain or chest discomfort.
Pain in acute MI occurs suddenly, often at night or in the early morning hours. Painful sensations develop in waves, periodically decreasing, but not stopping completely. With each new wave, the pain (discomfort) in the chest intensifies, quickly reaches a maximum, then weakens.
Unlike an attack of angina, pain during MI does not stop and does not decrease at rest, or when taking nitroglycerin (even repeatedly).
Objective clinical signs of myocardial infarction
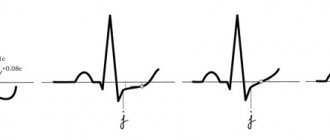
ECG changes that indicate acute myocardial ischemia (ST-T changes or complete block of the left bundle branch, the appearance of pathological Q waves).
Changes in the echocardiogram, which record the loss of viability of a section of the myocardium (thinned and not contracting), or disturbances in its local contractility.
Increase and/or decrease in the level of cardiac-specific cardiac biomarkers - cardiac troponins I and T, cardiac form of creatine phosphokinase (CF-CPK). Cardiac troponin reflects even minimal myocardial necrosis weighing less than 1 g, which is not detected by other diagnostic methods.
According to the size of the damage to the heart muscle, MI can be microscopic (focal or point damage), small (damage involves less than 10% of the muscle mass of the left ventricle), medium-sized (10–30% of the left ventricular myocardium) and large (damage occupies more than 30% of the left ventricular myocardium). ventricle).
Echocardiography is usually used to determine the size of the infarction.
MI is classified according to the nature of its course:
- acute (primary) – in the absence of signs of a previous MI;
- repeated – when a patient who has already suffered an MI in the past develops new foci of necrosis.
Depending on the clinical consequences, MI can be uncomplicated or complicated by acute left ventricular failure (pulmonary edema), cardiogenic shock, rhythm and conduction disturbances, acute left ventricular aneurysm, etc.
The entire healing process of an MI usually takes about 5–6 weeks.
In modern conditions, control over the process of restoration of damaged myocardium is carried out using the following imaging methods:
- echocardiography;
- radionuclide ventriculography;
- myocardial perfusion scintigraphy;
- single photon emission computed tomography;
- magnetic resonance imaging;
- positron emission tomography;
- computed tomography.
The basis of treatment for acute MI is the destruction of a thrombus in the coronary artery by any available methods. Typically, a thrombolytic drug is administered as early as possible (eg, 1.5 million IU streptokinase intravenously over 30 minutes).
If there are contraindications to thrombolytic therapy, highly effective methods of percutaneous coronary interventions are used - balloon angioplasty and coronary artery stenting, which account for 95% in the treatment of acute MI in a number of advanced countries. Angioplasty and stenting of the coronary arteries is the removal of obstructions to blood flow by expanding the artery from the inside with an air balloon or a stent, a device that prevents the artery from collapsing.
The optimal result can be obtained by combining these treatment methods.
To “save” the myocardium, the time window is approximately 6 hours from the onset of a pain attack. In this case, the first hour of the disease is considered the golden hour for successful recanalization of the infarct-related coronary artery, which can prevent further development of MI.
The drug of choice for pain relief is narcotic analgesics, in particular morphine hydrochloride.
In the absence of narcotic analgesics, you can resort to neuroleptanalgesia. For this purpose, the combined administration of the narcotic analgesic fentanyl and the neuroleptic droperidol is used.
In order to reduce the heart rate to 50 per minute, β-blockers are prescribed.
IHD plays a leading role among the causes of morbidity and mortality due to diseases of the circulatory system. The problem of the incidence of myocardial infarction, which is one of the main causes of mortality and disability and reduces the quality of life of patients with coronary artery disease, deserves special attention.
In recent years, the main age of onset of MI is 40–70 years, but 30-year-olds are also often found among patients. At a younger age, men suffer from MI much more often than women, but people over 70 years of age get sick equally often.
According to foreign and domestic data, after suffering an MI during the first year of illness, every tenth sick person dies.
Recurrent MI develops in 32–40% of patients. The prognosis for repeated MI is more severe than for acute MI, due to the more pronounced development of heart failure and cardiac arrhythmias. Repeated MI more often than acute MI leads to disability, temporary and permanent loss of ability to work, and higher mortality. This makes the issue of rehabilitation of patients after acute MI particularly relevant. Preventing recurrent myocardial infarction is a vitally important goal of care for the patient and his relatives.
It is important for all participants in the adaptation and rehabilitation process to realize that recurrent MI can be prevented in most cases. The fact is that a patient who has suffered an acute MI is already very well aware of his disease and the high risk of its recurrence if the basic principles of prevention are not followed.
Basic principles of prevention of complications and recurrent myocardial infarction at the outpatient stage
The outpatient-polyclinic stage of rehabilitation of persons who have suffered an MI begins after completion of treatment in a hospital or department of a cardiological sanatorium and continues for almost the rest of their lives. It includes a number of activities whose task is to prevent complications of acute MI, prevent recurrent MI, maintain physical condition at a satisfactory level and return to normal life.
The basic directions of the restoration process are:
- formation of adherence to treatment of coronary artery disease and self-monitoring of the cardiovascular system;
- restoration and maintenance of necessary physical activity;
- assistance in psychological adaptation to new living conditions (teaching the ward to help himself in stressful situations, emotional states such as fear and/or depression, developing the ability to psychologically adapt to the consequences of the disease);
- healthy and healthy lifestyle (fight against smoking, balanced nutrition, etc.).
Formation of adherence to treatment of coronary heart disease and self-monitoring of the cardiovascular system
Adherence to treatment is a disciplined and responsible approach to fulfilling the prescriptions of a medical professional and the person’s attitude towards regular self-assessment of the clinical condition. If necessary, family members should be involved in this work.
The presence of chronic ischemic heart disease, against the background of which MI developed, requires constant or periodic medication to prevent possible complications and recurrent MI.
The dosage of drugs should be selected individually for each patient, especially for antihypertensive drugs. An excessive decrease in blood pressure in a patient who has had an MI may be the cause of an ischemic stroke.
With great caution, a patient after an MI should consume nitrates, which will only help ease and temporarily muffle the pain. An overdose of nitrates can cause recurrent MI. They are mainly used as adjuvant drugs in suspected stressful situations or unexpected angina.
When women reach menopause, replacement therapy, including estrogen, can be prescribed. In this case, the specific treatment regimen must be agreed upon with an endocrinologist and gynecologist.
A sick person after suffering an acute MI should be able to independently measure the respiratory rate, pulse and blood pressure level, which will allow timely detection of signs of a pathological reaction to physical activity, psychogenic factor, etc.
Heart rate is a very significant indicator. Both a frequent pulse and a rare one are dangerous, since the heart muscle cannot fully fill with blood with such a pulse.
All deviations in physiological parameters must be recorded in a personal diary. For example, before performing physical activity, a sick person counts the pulse on the radial artery for 15 seconds at rest. Then he counts the pulse every 5 minutes during the exercise, before the exercise on the simulator, immediately after it and 5 minutes after the end of the exercise; All data and unpleasant sensations that appeared during the load are recorded in a diary.
At the moment of a heart attack, the ward is obliged to immediately provide himself with help, without waiting for it from the outside.
So, if pain occurs during physical activity, you must immediately stop it, sit more comfortably, and place your feet on the floor. If pain occurs at rest, in a lying position, you should immediately sit comfortably. Provide access to fresh air (open a window, unbutton clothing that makes breathing difficult). Take a nitroglycerin tablet under the tongue or spray one dose of nitroglycerin aerosol under the tongue (without inhaling). If there is no effect, repeat taking the tablet after 3 minutes, and the aerosol after 1 minute. Call an ambulance and chew 0.25 g of aspirin before it arrives.
Restoration and maintenance of necessary physical activity
It has been established that people who maintain the necessary physical activity after an acute MI suffer repeated MIs 5–7 times less often and die 5–6 times less often than sick people leading an inactive lifestyle.
The famous Belarusian physiologist Academician Nikolai Ivanovich Arinchin proved that skeletal muscles are, first of all, suction-discharge micropumps that self-supply with blood. These are peculiar peripheral hearts, effective helpers of the heart.
When the muscles perform this or that physical work, the micropumps contained in them are activated, which suck in arterial blood and then return venous blood to the heart, increasing its filling.
If a person moves little, his skeletal muscles work poorly as pumps, so the heart does not receive proper help from them.
A sick person after an acute MI should adhere to such physical activity in which the relationship between the heart and its many assistants will be most favorable.
That is why patients who have suffered an MI or simply suffer from angina pectoris should, at a minimum, perform various household activities that are not contraindicated for them.
Patients on an outpatient basis are usually prescribed exercise therapy, exercise on an exercise bike, walking and skiing, climbing stairs, swimming in a pool, cycling, etc. Ideally, sick people should undergo exercise therapy courses under a physical rehabilitation program in special centers. The purpose of this or that load is determined by the physical therapy doctor. The higher the load, the more control is required over the conduct of classes.
In the process of conducting individual physical training and home exercises, at least once every 3–4 months, it is necessary to evaluate resistance (tolerance) to physical activity in order to determine the further level of activity and its optimal pace. This is done in special conditions under the supervision of a cardiologist during a test with a dosed load. Bicycle ergometry is most widely used.
The simplest and most accessible type of systematic training is measured walking at a moderate pace for 30 minutes 3-5 times a week. This is not just a walk, but a physical training session that must be performed as a medical procedure.
For walking, choose calm weather, without precipitation. If you can determine the number of steps per minute, after which there will be no unpleasant sensations, then it is better to adhere to the appropriate framework.
It is better to start with 80 steps/min, if this amount does not cause pain in the chest, severe shortness of breath, suffocation or difficulty breathing in the sick person; Only the slightest shortness of breath is acceptable. Then, gradually adding steps, you need to bring their number to 130 per minute. This usually takes about 2–3 months. Frequency
Observation, rehabilitation and care 13
3’2019
MEDICAL KNOWLEDGE
heart rate during physical activity should increase by no more than 10–15 beats/min.
The distance a sick person travels should be increased very carefully. After increasing the load, the patient must measure blood pressure and pulse. If the indicators differ from the norm, the load needs to be reduced.
In second place in terms of frequency of use is therapeutic exercises, in third place are sedentary or active games.
Ways to train your peripheral hearts daily
- Learn to wiggle your toes non-stop, make cycling movements with your legs without lifting them off the floor. Contracting muscles will lift venous blood to the heart, facilitating its work.
- Contract the gluteal muscles and anus to avoid stagnation of venous blood in the pelvis.
- Contract the abdominal muscles, thereby massaging the internal organs.
- Make various movements with your body.
- Periodically do deep breathing movements. In this case, the descending diaphragm presses on the internal organs of the abdominal cavity, squeezing venous blood from them into the chest cavity, and then to the heart, while simultaneously massaging the internal organs. The expansion of the chest straightens the lungs, blood flows to them, which also facilitates the work of the heart. In this way, the thoracic, abdominal and diaphragmatic pumps are trained - assistants to the heart, eliminating blood stagnation in the internal organs.
- Move your right and left shoulders alternately or together. Contract the muscles of the back and shoulder blades, bringing them closer and apart.
- Work with your fingers, clench your hands into a fist, contract the muscles of the shoulder and forearm.
- Contract the neck muscles with deviation and rotation of the head in different directions. Do self-massage of the muscles of the neck, base of the skull and head.
- Massage the ear canal and ears, which increases blood supply to the brain and hearing.
These movements, invisible to others, can be diversified, performed while sitting in the cinema and during work breaks, making them automatic, as necessary as breathing, blinking, etc.
It is advisable to perform these exercises at least 3 times a day (before breakfast, before lunch and before dinner), and be sure to monitor the sensations in the heart area.
Help in psychological adaptation to new living conditions after myocardial infarction
In most cases, the psychological state of sick people improves several months after the development of MI and is practically no different from their usual state before MI.
A variant of normal psychological adaptation is a general satisfactory psychological state with periodically recurring, not sharply expressed pathological phenomena (depressed mood, anxiety with increased frequency of angina attacks, etc.).
In a certain proportion of people who have suffered an MI, at the outpatient stage, irritability, mood instability, sleep disturbances, often pronounced fear for the heart (cardiophobia), and fear of sudden death are observed. This can change the behavior of a sick person: he is afraid to go out unaccompanied, to take a trip out of town where there may not be a doctor nearby, etc. In some cases, hypochondria develops (increased concern for one’s health). A sick person “goes into illness”, convinced that he has a serious and incurable disease that requires round-the-clock medical supervision.
Unfortunately, after an MI, the patient’s relatives often begin to consider him disabled, surround him with excessive care and try to limit his physical activity. This attitude has a bad effect on the psychological state of a sick person and makes it difficult for him to return to a full life.
The most accessible form of working with relatives is group or individual classes and conversations, during which they are given the necessary medical and hygienic information. During classes, it is advisable to explain the principles and methods of rehabilitation, the role of exercise therapy, psychological aspects, hygiene of sexual life after an MI, preparation for the return of a sick person to work, lifestyle after an MI, the need to quit smoking, diet, etc.
Autogenic training is considered an effective means of psychological rehabilitation, for which patients with MI are taught self-hypnosis techniques against the background of muscle and mental relaxation. It is important to note that when conducting classes with patients with coronary artery disease, significant attention should be paid to developing in them the correct attitudes towards disease prevention. As a result of mastering autogenic training, patients gain the opportunity to inspire themselves with everything that is reasonable, useful and necessary for health. Under the influence of such training, the patient’s mood improves, sleep normalizes, and various pain sensations decrease. Classes are conducted individually or in groups of up to 10 people using tape recording, preferably after lunch.
Anti-smoking
The primary goal at all stages of patient management after acute MI is smoking cessation. This is a long and complex process. The nurse should make every effort to motivate the patient to permanently stop smoking all types of tobacco. She must
Observation, rehabilitation and care 14
3’2019
MEDICAL KNOWLEDGE
give patients practical advice in a simple and personalized way: don’t smoke or even try. The risk from secondhand smoke should also be discussed.
Anti-smoking policies will be more effective if they are aimed at the entire family as a whole, rather than at an individual. In addressing the issue of effectively combating smoking, a nurse can use the European principle of “5 A”.
- Ask (survey): systematically identify all smokers at every opportunity.
The nurse should ask the patient about the patient's smoking habits (whether he smokes or whether anyone close to him smokes) and be sure to keep appropriate medical records.
- Assess (situation assessment): limit the extent of the habit and encourage the patient's tendency to quit smoking.
To ensure that a smoking cessation intervention is effective, the nurse should:
- strengthen the positive image of non-smoking;
- advise all smokers to quit smoking;
- explore the patient's attitude towards smoking and correct misperceptions (for example, that it is too late to start);
- support the patient's motivation and prepare him to take action, but do not force him if he is not yet ready for this.
- Advise (discussion, consultation): strongly encourage people to quit smoking.
To immediately combat a dangerous habit, the nurse must:
- at every consultation, meeting with a patient or home visit, look for an opportunity to raise and discuss issues related to smoking, the patient’s attitude towards smoking and the health status of all smokers; give a complete, clear, specific and personalized statement about the risks and harm caused by smoking to health, repeat and reinforce it;
- Help patients who are ready to quit smoking by drawing up an individual strategy plan: giving advice, distributing self-help booklets and brochures and providing the necessary support (set a specific date, involve a spouse and friends, avoid “smoking situations”, etc.);
- provide constant monitoring, in case of resumption of smoking, try to convince the patient to quit again.
- Assist: Arrange for smoking cessation to implement a strategy that includes behavioral counseling, nicotine replacement therapy, and/or pharmacological assistance.
First, it is necessary to determine the form of tobacco addiction in order to choose the most effective way to quit smoking. Conventionally, there are two main forms of smoking addiction – psychosocial (non-pharmacological) and nicotine (pharmacological).
It is almost impossible to get rid of the psychosocial form of tobacco smoking on your own. Therefore, such a patient should be provided with regular psychological assistance and support in quitting smoking.
With nicotine (pharmacological) dependence, the body gets used to it and requires maintaining a certain concentration of nicotine in the blood. Smokers regulate it by the depth and frequency of puffs. Therefore, they should be recommended replacement therapy with drugs containing nicotine. The main purpose of their use is to prevent withdrawal symptoms.
You can reduce your dependence on tobacco with the help of calming and mobilizing breathing exercises, manipulating various objects (fingering a rosary, squeezing a wrist expander, etc.).
- Arrange (coordination): agree on a program of subsequent visits.
Nursing care is provided as follows:
- a short one-on-one consultation regarding smoking cessation, during which the patient may be given explanatory brochures or leaflets;
- repeated consultations or invitations to a series of meetings at regular intervals (after 1, 3, 6 months), during which the anti-smoking attitude is strengthened.
Balanced diet
In the process of restoring a patient’s health after an acute MI, great importance is given to proper nutrition. Diets may be different, but they all have common principles:
- reducing the calorie content of food;
- limiting fatty, flour and sweet foods;
- avoidance of hot and spicy foods;
- minimum salt consumption – no more than 5 g per day;
- the amount of fluid consumed is about 1.5 liters daily;
- eating frequently, but in small portions.
The diet must include foods containing fiber, vitamins C and P, polyunsaturated fatty acids, and potassium.
The following foods are allowed: low-fat meat, fruits and vegetables (except spinach, sorrel, radish), vegetable oils, vegetable soups, compotes and juices without sugar, weakly brewed tea, bran and rye bread, cereals, low-fat fish, low-fat dairy products fat content, omelette.
It is advisable to refrain from fatty meat, sausages, smoked foods, fried foods, mushrooms, legumes, fresh bread, any baked goods, confectionery, spicy dishes (marinades, pickles, canned food, etc.), and alcoholic beverages.
It is necessary to strictly control the caloric content of food. The daily norm should not exceed 2500–3000 kcal. If you are overweight, caloric intake should be reduced to 1800–2000 kcal. However, you need to change your diet very carefully, since rapid weight loss is a new stress for the body. It is very important to avoid fasting. First, you need to try to reduce the intake of fast carbohydrates into the body, that is, give up sweets (cakes, chocolate, pastries, etc.). Fasting days are recommended (for example, eat only apples or cucumbers, or a lean piece of meat with a vegetable side dish).
An example of a light diet for a sick person after an MI:
- two light breakfasts (cocoa, milk, cabbage salad);
- lunch (cabbage soup, lean meat, peas, apples);
- afternoon snack (cottage cheese and rosehip decoction);
- first dinner (boiled fish and vegetable stew);
- second dinner (yogurt and rye bread).