Heart rate deviations occur as a result of pathological and natural physiological phenomena. Changes in the pulse rate can move in two directions. A decrease is called bradycardia, an increase in cardiac activity is called tachycardia.
A normal, adequate value is considered to be an interval of 70 to 80 beats per minute; this is recognized by both the World Health Organization and national cardiological societies.
Deviations of even 5-10 beats per minute are considered pathological and require prompt assessment under the supervision of a competent cardiologist.
The pulse is 90, so this is a mild tachycardia, which is not the norm. Regardless of gender, age, hormonal state, you need to go to the hospital for diagnostics.
You can help on your own to an extremely limited extent, and this must be done carefully so as not to cause harm.
Are these indicators normal?
As has already been clarified, no. A heart rate of 90 beats per minute is not normal. This abnormality is called tachycardia. This level should not occur in elderly patients, women, or the stronger sex.
The only exception is for younger people: in children, standard levels are several times higher than in adults, which is explained by the small size of the heart and the need for more active activity.
The heart rate stabilizes by the age of 15-18, by the age of 25 it remains at the same level, the heart rate reaches its peak by the age of 30, persists for 10 years, then falls again.
Physiological reasons for increased heart rate
There are not many of them. Natural factors can be determined by the absence of pronounced symptoms: pathological tachycardia makes itself felt by a feeling of chest pain, shortness of breath, sweating, darkening in the eyes.
There are also vegetative symptoms in the absence of pathologies, but their duration is no more than a couple of minutes.
What reasons can explain a high pulse:
- Long-term stress. Characterized by increasing phenomena. Within tens of minutes, the concentration of corticosteroids and catecholamines increases, reaching a maximum after several hours.
Vegetative manifestations are minimal or completely absent. In most cases, a person does not feel such tachycardia; it is detected only through electrocardiography and other methods.
- Jar of Hearts. Of a momentary nature. A classic situation, accompanied by a sharp release of specific hormones of the pituitary gland and adrenal glands, an increase in blood pressure and heart rate.
Since the concentration of substances increases in a short period of time, the manifestations are noticeable. Possible development of fainting and disturbances of consciousness.
- Nightmares. Vegetative elements, including heartbeat, headache and others, and other symptoms appear for 2-3 minutes, everything returns to normal after the end of the process.
There is no need to do anything, it is permissible to wash your face with cold water, take a tablet of a mild sedative based on motherwort or valerian.
- Intense physical activity. Especially if an untrained patient is active. The more familiar the body is, the less likely it is that the heart will skip a beat.
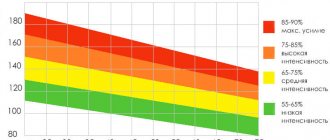
In an underdeveloped person, the muscular organ begins to work to the limit, and, having reached 180 beats per minute, the heart changes the nature of its activity.
Blood pressure begins to drop to critical levels. Everything can end in cardiogenic shock or even more severe conditions, potentially fatal.
Therefore, it is not recommended to overload; you need to increase physical activity gradually as you train your body.
If a person plays sports, he should do it under the supervision of an instructor, or at least purchase a special manual.
- Abuse of caffeinated drinks. You cannot drink more than a cup a day. If you have hypertension, coffee is generally contraindicated.
Physiological reasons carry risks only in the latter case. In other situations there are no dangers and no special assistance is required.
A pulse of 88-91 develops as a result of stress, nervous shock, sleep disturbances or problems with the body's fitness.
Why is a high pulse dangerous at normal blood pressure levels?
The manifestation of a specific symptom indicates a lack of timely treatment or ignoring the advice of medical professionals. The problem with this disease does not heal itself and the patient’s health condition may deteriorate significantly over time.
As the disease progresses, the functioning of the basic systems in patients deteriorates:
Advertising:
- heart pathologies;
- thyroid gland;
- hematopoietic organs (liver, spleen);
- respiratory system.
Their tendency to relapse of diseases and transition to chronic phases increases. A patient suffering from a high-frequency pulse with normal pressure suffers
:
- arrhythmic shock;
- swelling of the lungs;
- increased frequency of short-term fainting;
- cardiac asthma;
- periodic pain in the heart area;
- darkening of the eyes, with a feeling of discomfort;
- dizziness and states of weakness developing against the background of impaired activity of the circulatory system.
During pregnancy, manifestations of tachycardia are a common occurrence.
In what cases is 90 beats per minute an indication of pathology?
Possible diseases include:
- Hyperthyroidism. Excessive synthesis of thyroid hormones (T3, T4), as well as the thyroid-stimulating substance TSH, it is of pituitary origin.
Symptoms: palpitations, headache, vertigo, shortness of breath, fatigue, fatigue at any time of the day, problems sleeping, increased body temperature.
The causes of the disease-causing condition are improper diet, tumor pathologies.
- Hypercorticism. Excessive production of adrenal hormones, primarily cortisol. Neoplasia affects the organ itself or in the pituitary region.
The main clinical variant of the pathological process is Itsenko-Cushing syndrome. Accompanied by back pain, problems with the musculoskeletal system, sudden weight gain, fat deposition on the face like the moon.
The condition can be normalized surgically. Drugs are also used to neutralize the negative effects of cortisol (decreasing the sensitivity of specific receptors).
- Pathologies of the cardiovascular system. Including mitral valve stenosis, cardiosclerosis, myocardial infarction and consequences after the end of the acute period, pulmonary hypertension, and other processes of a similar kind.
The clinical picture is common: suffocation, shortness of breath, chest pain, low tolerance to physical activity and other manifestations. They require an assessment by a cardiologist; it is better not to delay visiting a doctor.
- Atherosclerosis of the aorta and its branches. It should be mentioned separately. The disease is accompanied by deposition of lipids (cholesterol) on the walls of blood vessels or acute narrowing of the lumen.
The inability to overcome resistance leads to increased cardiac activity.
We have to work more actively to provide the tissues with the necessary substances.
- Brain tumors. Usually the chiasmal-sellar region is affected. If they are large in size, they create a mass effect (compression), increase the pressure of the cerebrospinal fluid, which affects the condition of the cranial nerves. Treatment is surgical, and diuretics are also used to prevent compression.
- Kidney problems. Accompanied by lower back pain, urination disorders such as an increase in urine volume or frequent unsuccessful urge to empty the bladder. The properties of excrement change: color, smell.
- Diabetes. Deserves special attention. Destroys the entire body, including the cardiovascular system.
Finally, the heart rate increases due to the hypertensive process. A long-term illness is accompanied by severe, constant tachycardia.
A pulse of 92-95 and higher is the result of pathologies of the cardiovascular, excretory, and nervous systems. The cause can only be determined based on the results of special diagnostics.
Will it be possible to reduce the rate at home?
It is worth taking some actions, the main thing is not to go too far and “work” strictly according to the instructions.
The algorithm is as follows:
- Measure blood pressure and heart rate. This will be needed to assess the effectiveness of first aid. If necessary, baseline data is reported to the emergency team.
- Take 1 beta blocker tablet. Anaprilin (preferably) or Carvedilol will do. Violation of the dosage can lead to cardiac arrest or heart attack.
- Use a mild sedative based on motherwort or valerian. Just not in the form of an alcohol tincture. Ethanol excites the nervous system.
- Drink 20-30 drops of a drug based on phenobarbital. Corvalol or Valocordin. Exceeding the dosage is also unacceptable. In the case of organic origin of tachycardia, the effect of such a measure will be minimal.
- Brew tea based on chamomile, St. John's wort, peppermint, motherwort, valerian and anise. Drink at one time, in one gulp. You can eat a tablespoon of lemon, grated with honey.
- Take a horizontal position. Do not make unnecessary movements, especially do not engage in physical activity.
- Use breathing techniques: inhale for 5 seconds, exhale for the same amount. For 10 minutes.
Now it is important to look at the condition. If the heartbeat does not return to normal within 20 minutes, you need to call an ambulance.
It is not recommended to engage in amateur activities, it is dangerous. Cardiac arrest, heart attack, stroke and other “delights” are possible.
The absolute indications for seeking medical help are the symptoms described below.
Treatment and ways to alleviate (reduce) the condition of an accelerated pulse
Treatment of emerging tachycardia
directly depends on the main reasons for its occurrence. To reduce the high pulse rate that occurs after physical exercise, or emotional tension after stressful situations, you need to urgently stop their impact and the pulse will return to normal levels on its own.
Advertising:
An increased number of heartbeats in a state of absolute (conditional) rest requires immediate medical diagnosis to identify the causes of its occurrence and select appropriate treatment.
Frequent pulse with normal blood pressure
, the causes of which have been identified, requires urgent treatment.
The most common treatments for high heart rate include:
- against the background of anemia (low hemoglobin level) - medications that increase the level of iron in the patient’s blood;
- reduction in temperature associated with colds and infectious diseases;
- disruption (dysfunction) of the thyroid gland requires normalization of hormonal levels in the patient’s body;
- a number of neurological disorders involve increased stabilization in the functioning of the nervous system.
Medicines aimed at artificially reducing high heart rates, if taken uncontrolled, can pose a threat to the patient’s life.
Depending on the general condition of the body and the symptomatic manifestations of the disease, the following medications are prescribed:
- against the background of hormonal dysfunctions - Atenolol, Propranolol (beta blockers);
- with increased productivity of adrenaline - Phentolamine (adrenoblocker);
- preparations of plant origin for vegetative-vascular dystonia or obvious disorders of the nervous system - Persen, Novopassit, valerian or artificial (synthetic) origin - Diazepam, Phenobarbital tablets;
- against the background of cardiac arrhythmias - Propranolol, Flecainide, Adenosine, Verapamil;
- to stabilize the heart rate during tachycardia - Propranolol.
Advertising:
If your health worsens - with a high heart rate, you must:
- an influx of fresh air - you need to go outside or breathe near an open window;
- remove tight clothes - unbutton the collar, take off a thick sweater;
- apply a towel moistened with cold water, a bottle filled with chilled water, and wash;
- While holding your breath, drink at least 1 glass of water (below room temperature).
If these measures do not produce the required therapeutic effect, it is necessary to call emergency help (especially at night, when the patient is in a state of absolute rest).
Under no circumstances should you self-medicate (take medications) - this is fraught with the development of complications from the cardiovascular system.
When should you go to the doctor?
A visit to your doctor is required if the following symptoms occur:
- Shortness of breath for no apparent reason. Even in a calm state, with minimal physical activity.
- Headache.
- Feeling of heartbeat. Normally, a person does not notice such physiological processes.
- Dull, pressing discomfort in the chest. Appears suddenly. It's important to say. Acute, stabbing pain extremely rarely accompanies heart attacks and emergency conditions; more often it is a manifestation of intercostal neuralgia or angina. Which, however, is also quite dangerous.
- Fainting or pre-syncope. Darkness in the eyes, ringing in the ears, weakness in the legs.
The following signs are especially alarming:
- Sharp headache, pounding in nature.
- Suffocation.
- Focal neurological manifestations: decreased vision, hearing, speech dysfunction.
- The discomfort in the chest is unbearable: it presses, radiates to the back, arms.
- Paralysis, paresis, decreased sensitivity.
These are grounds for calling an ambulance. Another point that makes it necessary to go to the emergency room is tachycardia at rest, at night, after taking medications. You won't be able to cope on your own.
Symptoms
A physiological increase in heart rate should not be accompanied by any discomfort. And if symptoms arise that are unusual for a person, this serves as a good reason to contact medical institutions.
Signs that should alert you include:
- dizziness;
- “cloudness” in the eyes, double vision, flickering of “midges”;
- pain in the chest and chest area;
- shortness of breath, intermittent breathing;
- sudden profuse appearance of cold sweat;
- sudden weakness and trembling of the limbs;
- feeling of coldness in the hands and feet.
These signs, if you do not pay attention to them, can lead to serious consequences: disruption of the functioning of vital body systems and the development of severe pathologies.
What needs to be examined
The functioning of the cardiovascular, excretory, nervous, and endocrine systems is subject to assessment. Relevant specialists. The main one is a cardiologist, the rest are connected as needed.
Among the techniques:
- Collection of medical history and complaints of the patient about his own condition. Objectification of symptoms plays a key role in diagnosis and determining its directions.
- Measurement of blood pressure, heart rate. Using an automatic device.
- Listening to heart sounds.
- Electrocardiography. Profile research. They resort to him first of all. Allows you to identify subtle changes in the functional activity of a muscle organ. Deciphering requires a highly qualified cardiologist.
- Echocardiography. Ultrasound examination of the condition of the heart muscle.
- Assessment of neurological and nephrological status.
- Blood and urine tests.
Specialists whose consultation may be required, in addition to the cardiologist: endocrinologist (hormonal levels), neurologist (CNS), nephrologist (excretory system, kidneys). In other situations, a neurosurgeon (identified brain tumors), an oncologist.
Risks and consequences
An elevated heart rate with certain symptoms can be very dangerous and require immediate medical attention. If neglected, there is a very high risk of developing dangerous conditions such as arrhythmia, tachyarrhythmia, thromboembolism and even heart attack. In addition, very low blood pressure along with a rapid pulse may indicate internal bleeding, chemical poisoning, or an attack of hyperthyroidism.
A constant low heart rate can be dangerous for the heart, since there is a constant heavy load on this organ, and this creates favorable conditions for early wear of the myocardium, insufficient blood supply to the ventricles and oxygen to the body.
As a result, ischemia develops and the risk of early heart attack increases.
Treatment methods
Therapeutic measures are divided into several groups:
- Use of medications.
- Folk recipes.
- Surgical intervention.
- Lifestyle changes.
Medicines. The following groups of pharmaceuticals are used as a primary method:
- Beta blockers. To reduce the sensitivity of special receptors in the body. Carvedilol or Anaprilin, Metoprolol.
- Sedative drugs. Herbal (motherwort, valerian in tablet form). Accelerate inhibition of the nervous system.
- Tranquilizers. They influence in the same way. Diazepam, Sibazon, Relanium are used.
- Calcium channel blockers. Prevents the penetration of element ions into blood vessels and tissues. Thus, the blood supply structures are not narrowed, and the third reflex zone of the heart is not stimulated. Diltiazem and Verapamil are suitable.
Cardiac glycosides are used a little less frequently: Digoxin and tincture of lily of the valley.
Traditional methods:
- Honey and lemon (2 tablespoons of the mixture 3 times a day). St. John's wort, motherwort, valerian, anise, peppermint in tea form. Take 2 glasses
- once a day
- Chokeberry tincture (200 berries per 400 ml of vodka, prepared in 21 days). Take 2 teaspoons 2 times a day.
Before use, it is better to consult with a naturopath or, at a minimum, a cardiologist.
Surgery. Indicated in extreme cases: in case of heart defects, it is aimed at creating an anatomical defect, in case of a tumor process, excision of neoplasm, in case of stable tachycardia, installation of an artificial pacemaker (pacemaker), and in case of destruction of the atria as a result of infectious pathologies, through prosthetics.
Lifestyle changes.
- Quitting smoking and alcohol.
- Normalization of sleep. 8 hours per night, most of the rest should occur before 23.00.
- Drinking regime. 2 liters per day.
- Salt. No more than 7 grams.
- Physical activity. 2 hours, light walks or exercise therapy.
- Breathing exercises (not according to Strelnikova). The program is selected individually.
Diet correction.
Can:
- Vegetables and fruits without restrictions.
- Juices.
- Cereal porridge with water and milk.
- Lean meat, soups.
- Coarse bread.
- Berries, natural sweets.
- Eggs.
- Butter, vegetable oils.
It is forbidden:
- Fat meat.
- I'll bake it.
- Fried pies.
- Smoked meats.
- Salt more than 7 grams.
- Coffee and tea.
- Canned food, semi-finished products.
Treatment tables No. 3 and No. 10 are shown. The menu is compiled independently or on the advice of a nutritionist. Cooking methods: boiling, steaming, baking. Compliance with the principle of fractional meals (3-5 times a day); you cannot eat at night.