Mechanism of development of vertigo
If we consider dizziness from an anatomical point of view, the causes of this condition are quite simple. The vestibular apparatus, responsible for human balance and coordination in space, is located in the inner ear. Vision and muscle reflexes help a person navigate the environment. All received information enters the brain. And it is he who controls the functioning of the vestibular apparatus.
Sometimes the connection between the inner ear and the brain can become disrupted. A person loses the ability to navigate in space. Dizziness appears. To restore the lost connection, the brain immediately launches several reactions at once. Some of them may affect neighboring centers (for example, emetic). This leads to the appearance of unpleasant accompanying symptoms.
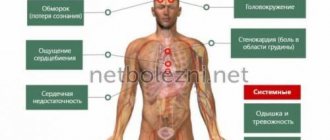
Symptoms of presyncope
There are not many signs of a pre-fainting state; it usually manifests itself in dizziness, sometimes nausea appears (vomiting almost never), the eyes become dark, orientation in space disappears and weakness appears in the muscles, which makes the person want to sit down or lie down. In some cases, there is noise or heat in the ears, and one’s own heartbeat is clearly registered. The blood drains from the face, causing the skin to appear very pale or take on a yellowish or greenish tint if the patient has any chronic diseases. Sometimes, against the background of a pale face, a cyanotic nasolabial triangle appears (with diseases of the heart and respiratory system). Attention! Usually, when a patient notices a faint state, he tends to take a safer position (sit or lie down). After a few minutes, blood flow is restored and the patient feels only residual weakness and, possibly, a headache. If you can’t get into a comfortable position, for example, while standing in a stuffy vehicle or at a meeting under the sun, full-blown fainting may develop. And fainting is dangerous not only because of the reasons that caused it, but also because of the consequences: head injuries when hitting the ground, getting hit by a car when fainting near the roadway, injuries of varying severity (and even lethal) when falling on surrounding objects: steps, sharp fences, corners of building plinths, etc.).
Sudden dizziness: 5 simple reasons
Typically, loss of communication between the brain and the vestibular system is rare and does not last long.
Dizziness that occurs is not considered a pathology in the following cases:
- Ride the carousel. Such entertainment creates a serious load on the vestibular apparatus. And if it is naturally weak and untrained, then it may well fail. Such dizziness usually occurs in women, since they also have psycho-emotional experiences added to the load.
- Stress, anxiety. If dizziness occurs during a speech in front of a large audience or after a reprimand from a boss, then the cause of vertigo is the production of a large amount of adrenaline. This hormone causes vasospasm. And this leads to a temporary deterioration in blood flow in the brain.
- Climbing to heights. In this case, the unpleasant phenomenon is also considered a physiological norm. When rising to a height, a person’s eyes cannot quickly focus on distant and close objects. Abrupt switching between objects causes dizziness.
- Hunger. Similar problems are common to all fans of strict diets. If a person does not receive enough nutrition, then a glucose deficiency occurs in his body. The absence of the main “fuel” leads to deterioration of brain function and the appearance of dizziness.
- Active exercises. Exercise enthusiasts should remember moderation. Excessive exercise can cause low blood pressure. This leads to dizziness and sometimes fainting. The unpleasant condition may be caused by unsuccessful sudden movements of the head, as a result of which the blood supply to the brain is disrupted.
An attack of dizziness may occur in response to taking certain medications. The most common sources of unpleasant symptoms are NSAIDs, antidepressants, antibiotics, and cancer medications. If your head is “turned” by medications, be sure to consult a doctor to change the drug.
Vestibular neuronitis
Why does it happen? The cause of the disease is considered to be an inflammatory process (probably of viral origin), selectively affecting the vestibular nerve.
Article on the topic
Movement therapy. How to regain coordination and balance
How it manifests itself. A single attack of dizziness, the intensity of which increases with changes in posture and may decrease when the patient tries to remain motionless and fixate his gaze on one point.
How to treat it. In the acute period, with the help of symptomatic therapy aimed at relieving dizziness, in the recovery period with the help of vestibular exercises.
Severe dizziness: 6 pathological causes
The causes of dizziness are not always harmless. Sometimes illnesses become sources of unpleasant conditions. In this case, dizziness occurs quite often and can last longer than a few seconds. To cope with this phenomenon, you need to consult a doctor. The severity of a symptom can be reduced (and sometimes completely eliminated) only through proper treatment of the underlying disease.
So, the causes of dizziness may include the following pathologies:
- Vegetovascular dystonia (VSD). A complex disorder in which a person experiences multiple impairments. All these symptoms are associated with malfunctions of the autonomic system. One of the common signs of VSD is dizziness. Such attacks are usually caused by sudden movements and rapid changes in posture. Dizziness does not last long. They go away on their own, without any intervention.
- Disorders in the cervical spine. Various injuries, osteochondrosis, intervertebral hernias can periodically remind you of themselves with sudden attacks of dizziness. They usually appear after active neck movements. The attack is accompanied by pain in the affected area, sometimes a crunching or crackling sound is heard.
- Anemia. Dizziness may occur due to iron deficiency. Most often this pathology is observed in children and women. With anemia, attacks are accompanied by high fatigue, weakness, pale skin, and pre-fainting conditions.
- Psychogenic dizziness. The reason for this pathology lies in the patient’s increased anxiety (people with an unstable psyche) or in the stress they have endured. Such people usually complain of poor sleep, fear of losing consciousness, a periodic feeling of shortness of breath, and increased heart rate.
- Vertebrobasilar insufficiency. This is a pathology in which blood flow in the vertebral or basilar arteries is weakened. Such problems lead to disruption of brain function. The pathology is characterized by regular attacks of dizziness, which can last up to an hour. In addition, patients complain of nausea, vomiting, and visual disturbances may occur. I often have a headache.
- Hypotension. A decrease in blood pressure is often accompanied by attacks of dizziness. Sometimes lightheadedness may occur.
Types of dizziness
If a patient consults a doctor with such a complaint, it is not always a case of true (vestibular) dizziness. But since most people mention this particular word, it has also entered medical terminology. There are 4 types of dizziness, which differ in origin and symptoms. Out of 100 people who came to the neurologist, the doctor states:
- systemic dizziness – 60 patients;
- impaired coordination – 15 patients;
- presyncope – 15 patients;
- “fog” in the head and blurred vision – 10 patients.
Three of the four symptom groups are not actually dizziness. This is the result of not only neurological, but also vascular, ophthalmological, orthopedic, and mental diseases. Certain types of dizziness are observed with migraine, cardiac arrhythmia, arterial hypertension, osteochondrosis, glaucoma, anxiety disorders, multiple sclerosis and many other diseases.
Severe dizziness: 6 dangerous reasons
In some cases, vertigo signals the development of severe conditions that require immediate medical attention. Causes of severe dizziness may include:
- Labyrinthitis (internal otitis). A viral infection in the inner ear may be asymptomatic at first. The only sign of otitis media is dizziness, which lasts for several minutes. Such attacks are repeated quite often. In the future, the viral process can affect the nervous system or brain.
- Concussion. Sometimes after a head injury, only dizziness appears. This symptom should not be ignored. It serves as direct evidence of a concussion. To eliminate the risk of swelling or serious brain damage, you should immediately seek medical help.
- Stroke. If dizziness is accompanied by sudden weakness, complaints of numbness of a body part, visual impairment, speech disturbances, then the risk of stroke is high. This is a severe pathology in which blood circulation in the brain is disrupted.
- Migraine. Dizziness accompanied by a severe headache may indicate a migraine. Many people believe that this condition is harmless. But doctors say that migraine, especially in an advanced state, can lead to severe damage (sometimes even to a heart attack or stroke).
- Cardiovascular diseases. Such pathologies are characterized by the appearance of dizziness every time a person gets up. It is caused by a sharp decrease in pressure. Symptoms like these may indicate dehydration, which is causing your blood to thicken. But if the problem is not fluid deficiency, then it may be the development of arrhythmia or heart failure.
- Tumors. Regular attacks of vertigo combined with headaches, usually in one side of the head, can signal the development of a tumor in the brain.
Dizziness - symptoms and treatment
Diagnosis of dizziness is based primarily on the collection of complaints, anamnesis (history) of the disease and clinical examination.
Collection of complaints and anamnesis
Basic questions that can be asked to a patient with acute dizziness:
- How and when did the dizziness start?
- How long does it last?
- What character, in the patient’s opinion, is dizziness (systemic, non-systemic, presyncope).
- Are there certain factors that provoke dizziness (turning the head or body, standing from a horizontal to a vertical position, being in crowded or noisy places, etc.).
- Is dizziness accompanied by pain (headache, chest pain, ear pain), hearing loss, noise in the ears or in the head.
- Are there any accompanying symptoms (double vision, difficulty swallowing, speech disorders, weakness in the limbs, nausea and vomiting) [1].
Physical examination
When examining a patient, the presence and characteristics of nystagmus, the presence of gait disturbances, the performance of coordination tests and stability in the Romberg position (standing with feet together, eyes closed and arms extended in front of you) are first assessed.
Evaluation of nystagmus. In order to correctly distinguish peripheral from central vertigo during the diagnostic process, it is important to determine the nature of the nystagmus. For this purpose, special Frenzel glasses are used: in them, it is difficult for the patient to fix his gaze on any object, which allows him to determine without distortion exactly how nystagmus manifests itself.
Differential diagnosis of peripheral and central dizziness:
- With a peripheral origin, nystagmus is usually horizontal or horizontal with rotational movements of the eyeballs, unidirectional and directed towards a more active labyrinth. When the gaze is fixed, the nystagmus decreases.
- In the case of central origin, nystagmus can be horizontal bidirectional (left-sided when looking to the left and right-sided when looking to the right), vertical or rotational. When fixing your gaze, it may decrease slightly, but, as a rule, does not change.
Positional tests are carried out at the appointment and help determine the cause of systemic vertigo and differentiate positional nystagmus from central nystagmus. The most commonly performed test is the Dix-Halpike test. The patient, who is sitting on the couch, is turned 45° to one side and quickly placed on the couch so that the head is thrown back over the edge of the couch. The doctor monitors the appearance of nystagmus, and the patient reports on his well-being. In the same way, the test is repeated with the head turned in the other direction.
If the answer is positive, it is possible to identify the most common cause of true dizziness, BPPV, and determine in which of the semicircular canals the otoliths causing dizziness are located [18]. With the appearance of nystagmus and dizziness, the most common localization of otoliths is revealed - the posterior semicircular canal.
Assessment of the vestibulo-ocular reflex (VOR). In the work of the vestibular system, the VOR is of utmost importance: thanks to it, a person can keep the object of observation in the field of view during various movements of the head. This is possible due to the fact that when the head is turned to the side, the eyes make a movement of the same amplitude and speed in the opposite direction.
VOR is assessed using the head rotation test (Halmagi-Kertoiz test): the patient is asked to fix his gaze on an object (for example, the doctor’s nose), then the doctor clasps his hands around the patient’s head in the temporal regions and sharply turns the patient’s head to the right and left by 10-20 °.
Normally, when turning the head, the gaze remains fixed on the object. The same thing is observed with damage to the central part of the vestibular analyzer. When the peripheral part is affected, when the head is turned, the eyes first move in the direction of the turn, after which the gaze is again fixed on the object.
Marching test (Fukuda test). To carry out the test, the patient closes his eyes, stretches his arms forward and begins to walk in place, raising his knees high. After 50 steps, the doctor assesses how much the patient has deviated from the initial position; normally, the angle of deviation should not exceed 30-45°. If there is a unilateral peripheral lesion, the patient turns towards the affected labyrinth. In case of damage to the central department, there is a lack of coordination, deviation in different directions, sometimes the patient falls or turns towards the pathological process when the cerebellum is damaged [28].
Postural reflexes , which make it possible to maintain a stable body position, are examined by gently pushing the patient into the upper torso. At the same time, the doctor is behind his back so that the patient does not see when and in what direction he will be pushed. With vestibular disorders, instability is possible, but in general the person maintains the posture.
Gait assessment (with eyes open and then closed). When observing a patient's gait, a balance disorder is often diagnosed. Many diseases of the peripheral and central nervous system are accompanied by typical gait changes, but in most patients with vestibular disorders it is not impaired, except in the acute stage of the disease.
An orthostatic test involves measuring blood pressure while lying down, immediately after moving to an upright position, and then over the next three minutes. The test is considered positive if systolic blood pressure decreases by 20 mmHg. Art. or more or diastolic pressure decreases by 10 mm Hg. Art. and more. The method allows you to identify pre-fainting conditions associated with orthostatic hypertension.
Instrumental examination
In most cases, data from a detailed survey, analysis of complaints and examination of the patient are sufficient to make a diagnosis. Instrumental methods are necessary if a central lesion of the vestibular analyzer is suspected and in the presence of concomitant diseases (for example, previous acute cerebrovascular accidents, the presence of space-occupying lesions or vascular anomalies in the past or present).
The need for computed or magnetic resonance imaging (CT/MRI) may arise if objective data are detected that require further examination. For example, vertical nystagmus, multidirectional, beating down or up may indicate damage to the stem structures of the brain or cerebellum [1].
Most often, CT and MRI can diagnose cerebral infarction, cerebral hemorrhage, multiple sclerosis, tumors of the brain stem and cerebellopontine angle, anomalies and other diseases accompanied by dizziness.
Ultrasound examination of extracranial and intracranial arteries is indicated if cerebrovascular disease is suspected with an appropriate history and the presence of risk factors (arterial hypertension, diabetes mellitus, obesity, hypercholesterolemia, heredity for cardiovascular diseases, previous acute cardiovascular diseases).
For dizziness that is accompanied by noise in the ear or hearing loss, pure tone threshold audiometry to determine auditory sensitivity to sounds of different frequencies. During this examination, the auditory threshold of bone and air conduction is compared, and if deviations from the norm are detected, the probable cause is determined (cerumen plug, otosclerosis, labyrinthitis, Meniere's disease, etc.).
A cardiac examination (ECG, ECHO-CG, Holter monitoring) is indicated if a cardiogenic cause of dizziness is suspected [5][8].
Stabilography is the study of balance using a moving platform. Using this method, it is possible to quantify involuntary postural reflexes, thanks to which a person does not fall, and also determine what role information from various senses plays in maintaining balance.
What to do?
It is almost impossible to independently determine the causes of frequent attacks of dizziness. Therefore, those who regularly experience vertigo are advised to go to an appointment with a therapist, or a neurologist. The specialist will carefully examine the patient’s complaints and prescribe diagnostic tests. If necessary, the doctor will refer the patient for consultations with an ENT specialist, an ophthalmologist, a cardiologist, or an endocrinologist.
To identify the causes of vertigo, the patient may be prescribed the following tests:
- Neurological tests. They allow you to assess the functionality of the vestibular apparatus.
- MRI or CT. Such brain studies reveal various disorders (hemorrhages, tumors, vascular pathologies).
- Ultrasound Doppler. Using Doppler ultrasound, the condition of the vessels of the head and neck is studied.
- Audiometry. Diagnostics allows us to assess hearing function.
- EEG. To study the activity of the cerebral cortex, the doctor will prescribe electroencephalography.
To quickly cope with dizziness (of course, if it is not caused by dangerous reasons), you can sit on any surface, relax a little and take 5-6 deep breaths. Be sure to open the window (if you are indoors) to provide fresh air. If the causes of vertigo are harmless, then such actions are quite enough for the dizziness to disappear without a trace.
VSD in faces
This page contains excerpts from patient histories, covering the main complaints with which people turn to us for help. This is done with the goal of showing how different and “complex” the symptoms of vegetative-vascular dystonia can be. And how closely it is sometimes “fused” with disturbances in the functioning of organs and systems. How it “disguises” itself as “heart”, “pulmonary”, “stomach”, “gynecological” and even “psychiatric” problems that people have to live with for years...
To learn more
Vestibular migraine
Why does it happen? According to one theory, during a migraine attack, changes in the activity of neurons in the cerebral cortex can reach the parietotemporal region, where the centers responsible for the sense of balance are located. According to another theory, during a migraine attack, biologically active substances are released in those areas of the brain stem that are related to the vestibular system.
How it manifests itself . An attack of rotational dizziness. In this case, there may not be a headache.
How to treat it. Antidepressants, anticonvulsants, beta-blockers.
Head spin! What herbs will help with dizziness Read more
BPPV
BPPV is diagnosed in 17% of patients complaining of dizziness and is the most common cause of its occurrence. Moreover, the frequency of its occurrence increases in proportion to age, and in women it occurs 2 times more often. This is a disease in which otoliths move into the semicircular canals of the inner ear.
Otoliths are calcium carbonate crystals normally located in the otolithic membrane of the inner ear.
With BPPV, attacks are usually triggered by head movements, especially at night, when the patient cannot control himself. There are frequent situations when dizziness occurs after turning in a dream or getting up/getting out of bed. In this case, dizziness begins acutely, but lasts less than a minute, although it may be accompanied by nausea and vomiting, nystagmus. It is not associated with hearing loss, noise, or ringing in the ears.
The duration of the attack usually does not exceed several minutes.
In most cases, the causes of BPPV cannot be determined. Only in certain situations is its development associated with head injuries, ear surgeries, or previous diseases of the inner ear.
But on the other hand, BPPV does not require specific treatment and, as a rule, goes away on its own in a few weeks or months. Patients are only taught special maneuvers to facilitate the release of particles from the affected semicircular canal to eliminate dizziness. But before they are carried out, it is imperative to consult a doctor who will confirm or deny the presence of BPPV and determine its type. Otherwise, as well as if the technique is violated, your condition may worsen.
There are more than 5 different maneuvers to relieve an attack of dizziness due to BPPV. The choice of which one will be most effective for an individual patient depends on which part of the labyrinthitis his otoliths move to. In most cases, the Eple maneuver is recommended. Its essence is as follows:
- turn the head 45° towards the affected ear and lie on your back (this may be accompanied by increased dizziness);
- the head is turned sharply towards the healthy ear so that it is at an angle of 45°;
- continue turning to the healthy side with the whole body so that at the end point the face is directed downward;
- rise to a sitting position, maintaining a head tilt of 45°.
You should remain in each position for about 1 minute, and change them as abruptly as possible.
In half of the cases, correct implementation of therapeutic maneuvers allows for long-term elimination of BPPV symptoms. Although 25-50% of patients experience relapses. In such situations, repeated maneuvers are indicated.