Kurganskaya Natalia Valerievna Doctor - obstetrician-gynecologist
✓ Article verified by a medical expert
Hot flashes are a strong sensation of heat that spreads throughout the body and is usually strongest in the head (face) and neck area. This condition can occur at any time of the day and is accompanied by a sharp rise in temperature, increased heart rate, redness of the skin and profuse sweating. Sometimes the listed symptoms are supplemented by flickering in the eyes, ringing in the ears, difficulty breathing and mental anxiety. The duration of hot flashes ranges from 30 seconds to several minutes.
The appearance of hot flashes can be observed both in women (a characteristic symptom of premenopause) and in men (as a result of a critical decrease in testosterone levels).
How to reduce hot flashes and how to deal with excessive sweating?
To reduce the negative consequences of hormonal disorders during menopause, you need to take appropriate medications, adjust your diet, and adjust your work and rest schedule. However, that's not all. There are some simple rules to reduce the unpleasant symptoms of attacks:
- Avoid going to the bathhouse and sauna. Hot air in steam rooms causes excessive sweating.
- Spend less time outside on hot days, and also stay as far as possible from heat sources - fireplaces, stoves, heaters, bonfires.
- Stop smoking, eating hot, fatty and spicy foods, coffee, alcohol and sweets.
- A woman's diet during menopause should include more fresh fruits and vegetables, dairy products, cereals, wheat bran, chicken eggs, and nuts.
These products have a beneficial effect on female hormonal levels, which helps reduce the symptoms of menopause. It is also worth including foods rich in so-called phytohormones in your diet. In their composition they are close to human hormones, but are not as effective. Eat: coconut, soybean and olive oil, lentils, flax seeds, garlic, chickpeas, beans, barley, rye. - Drink at least 1.5 liters of water per day. Due to increased sweating during menopause, the body quickly loses fluid, so it must be replenished in a timely manner.
- Do not wear synthetic clothing. It is better to give preference to cotton, silk and linen items. The exception is fleece clothing: this artificial material dries quickly and provides the necessary moisture removal.
- Avoid outfits with high collars. Choose clothes with a neckline and cutouts near the neck.
- Change synthetic bedding to natural ones. This will help you sweat less while you sleep.
- If you experience intense hot flashes, you can carry a spare set of clothes with you. If you get very sweaty, you will have the opportunity to change clothes.
- Observe personal hygiene rules. To avoid the unpleasant odor of sweat, it is recommended to use a high-quality antiperspirant that prevents the appearance of unpleasant odor.
- Make time for rest, try to be less nervous and engage in static sports - Pilates, yoga, stretching, callanetics. During this difficult period, regular seaside holidays are highly desirable for the female body, but it is important to avoid hot months (July, August) and choose more comfortable and cooler ones - May, June and September.
Treatment of hot flashes during menopause
Treatment of menopausal syndrome
The goal of treating the pathology of menopause is to reduce its manifestations and symptoms.
Antidepressants reduce the frequency of hot flashes during the pathological course of menopause.
To prevent osteoporosis during menopause, non-hormonal bisphosphonates are used; they reduce bone loss and the risk of fractures.
To reduce the manifestation of urogenital manifestations, local (vaginal) administration of estrogen in the form of cream or tablets is used.
The most effective method of treating menopausal syndrome during menopause is hormonal therapy individually prescribed by a doctor.
Hormone therapy as a treatment for menopause pathology is contraindicated in patients suffering from:
- endometrial, ovarian, breast cancer;
- coagulopathy (blood clotting disorder);
- liver dysfunction;
- thromboembolism, thrombophlebitis;
- uterine bleeding of unknown cause;
- renal failure.
In case of psycho-emotional manifestations, consultations with specialists in psychology are required every six months in order to monitor the condition and, if necessary, correct the emotional background.
What to take for hot flashes during menopause?
Most often, doctors prescribe menopausal hormone therapy (MHT) to patients. Normalizing hormonal levels by taking such drugs not only reduces sweating, but also improves psycho-emotional state, helps cope with mood swings, increases performance and optimizes concentration.
However, it must be taken into account that drugs that compensate for the lack of estrogen can activate the launch of developing oncological diseases - in particular, breast, endometrial or ovarian cancer and aggravate chronic diseases and the risk of thrombosis. Therefore, treatment with hormonal drugs should occur exclusively according to the regimen drawn up by the doctor.
In recent years, it has become possible to replace the use of traditional tablet medications with the use of hormonal patches, gel forms, and intrauterine complexes.
They are considered less dangerous in terms of the possibility of venous thrombosis.
Diagnosis of hot flashes
If you regularly experience even short-term flushes of blood, you should definitely consult a doctor, especially if the flushes are accompanied by dizziness, a sharp rise in temperature or severe chills. Diagnostic methods are designed to determine the main cause of the disease state and exclude (or identify) such serious and dangerous pathologies as malignant tumors. You will need to consult a gynecologist and endocrinologist. The doctor prescribes a pelvic ultrasound and other necessary examinations, and, after determining the cause and nature of the hot flashes, determines the course of treatment.
Hot flashes during menopause: treatment without hormones
Expert opinion
Many women cannot take hormonal medications due to certain health conditions. For example, if there is a risk of breast cancer, a tendency to form venous blood clots, cerebrovascular accident (stroke) and heart attack, hormone replacement therapy is not recommended, since the potential risks from it may be higher than the benefits.
Obstetrician-gynecologist of the highest category Oksana Anatolyevna Gartleb
To mitigate the intensity of menopause symptoms, not only hormone replacement therapy, but also other drugs are used. Instead of hormones, you can use the following:
Drugs that normalize blood pressure
During menopause, changes in the water-salt balance occur, resulting in fluid retention in the body and an increase in blood volume. This leads to increased blood pressure during hot flashes. Taking medications that lower blood pressure helps reduce sweating and the feeling of heat during such conditions.
Sedatives and antidepressants
These medications, given in small doses, help reduce the stress caused by hot flashes. In addition, taking antidepressants and sedatives in some cases reduces the frequency and intensity of hot flashes by normalizing the condition of blood vessels.
Expert opinion
Remember that antidepressants can be quite harsh on your health and may cause some side effects. Therefore, their prescription and selection of the appropriate dosage should be handled exclusively by a specialized specialist.
Obstetrician-gynecologist of the highest category Oksana Anatolyevna Gartleb
Vitamin and mineral complexes, dietary supplements
During menopause, it is recommended to take complexes rich in retinol, tocopherol, ascorbic acid, B vitamins, vitamin D, calcium, magnesium, boron.
Dietary supplements based on phytoestrogens. Phytohormones include coconut oil, chamomile, calendula, ginseng root, grapes, dates, pomegranates, red clover, alfalfa, flax, licorice, etc.
Signs, symptoms and sensations during male menopause
Most men during menopause experience erectile dysfunction and decreased libido, but in 20%, andropause is accompanied by other serious problems. Observed:
- Dizziness.
- Numbness of legs, arms.
- Sleep problems.
- Irritability, anxiety, even depression.
- Sweating.
- Headaches, heart pain.
- Hot flashes.
- Increase in body weight.
- Increased bone fragility.
These symptoms cause discomfort and significantly reduce the quality of life. In addition, they increase the risk of developing diabetes mellitus, coronary heart disease, and myocardial infarction.
Hot flashes during menopause: treatment with folk remedies
Not only traditional medicines, but also traditional medicine methods help to cope with fever and sweating during menopause. They should not be considered as the main means of therapy, but they can act as effective additional means.
Various herbs are used to combat the unpleasant symptoms of menopause. You can prepare decoctions and infusions from them, for example:
- Hawthorn fruits and flowers. Rinse 5 g of prepared raw materials, place in a thermos and pour a glass of boiling water. Leave for an hour. Take half a glass 2 times a day before meals. The infusion not only reduces the frequency and intensity of hot flashes, but also improves heart function and vascular condition.
- Red clover. Red clover belongs to the category of phytoestrogens, so this plant is actively used to reduce hot flashes. To prepare the infusion you need to take 2 tbsp. dry crushed red clover herb, place in a thermos and pour a glass of boiling water, leave to infuse for 10 hours. Take the resulting infusion before meals, 50 ml.
- Sage. It is useful to take a decoction. To prepare it, you need to take 1 tbsp. dry sage, pour 1.5 tbsp. boiling water and simmer for 5 minutes over low heat. Then cool the broth, strain and drink as tea throughout the day.
- Red brush root (rhodiola tetrapartite). Before taking products based on red brush, you should consult your doctor, as this plant is contraindicated for women suffering from hypertension. Pour the dried crushed root (1 tbsp) into a glass of water and boil for a quarter of an hour. Cool the broth, strain and take 100 ml before meals three times a day.
- Borovaya uterus.
This plant helps to compensate for the lack of estrogen, as it belongs to the category of phytohormones.To prepare a decoction of boron uterus, you need to take a tablespoon of the dry plant, pour a glass of boiling water over it and simmer over low heat for 5 minutes. Then strain, cool the broth and drink 100 ml before meals three times a day.
- Dry rosemary. To prepare the decoction, take 1 tbsp. raw materials, pour a glass of boiling water and boil for a quarter of an hour. Then strain, cool and take the resulting product before meals three times a day.
Menopause in a woman without hot flashes
Hot flashes in menopause: a compelling alternative to hormone replacement therapy
Hot flashes, according to patients and medical specialists, are the most characteristic and unpleasant menopausal symptom [1, 2]. Depending on the severity, hot flashes can have a negative impact on women's quality of life for 5–7 years [3, 4].
Hot flashes, as a vasomotor symptom, are accompanied by increased vascular reactivity and are characterized by an initial significant dilation of blood vessels and their subsequent narrowing. The pathogenetic mechanisms of hot flashes are still being studied. Presumably the symptom is the result of a violation of the temperature regulation mechanism in the hypothalamus due to a decrease in estrogen levels after preliminary sensitization to it.
The first line of treatment for hot flashes today is hormone replacement therapy (HRT), which has proven to be effective and have a positive impact on quality of life for many women [5, 6]. However, recent studies, including data from the Women's Health Initiative (WHI) [7, 8], show the unsafety of HRT in some cases. Selective estrogen receptor modulators (SERMs) that have antiestrogenic effects, such as tamoxifen and raloxifene, can also cause hot flashes, which are especially severe in women undergoing treatment for breast cancer [9].
Due to the high need for non-hormonal treatments for vasomotor symptoms, today the possibilities of using non-pharmaceutical methods and drugs from other groups are being actively studied. Specifically, a review of the literature shows that treatment with selective serotonin reuptake inhibitors (SSRIs) or serotonin and norepinephrine (SNRIs) reduces the frequency and severity of hot flashes in menopausal and postmenopausal women. Studies have demonstrated the high effectiveness of SSRIs such as paroxetine, citalopram and escitolapram, as well as the SNRI venlafaxine.
Two papers, “Hot flashes and night sweats in menopause: the current state of the issue” by D. F. Archer et al. [10], and “Do SSRIs and SNRIs Reduce the Frequency and/or Severity of Hot Flashes in Menopause” by Chris Stubbs et al.[11] They comprehensively consider the features of the pathogenesis of vasomotor symptoms, the limitations of classical therapy and the possibility of using other methods as its alternative.
Prevalence and general characteristics of hot flashes
As noted in the work of Chris Stubbs, between 80% and 90% of women experience hot flashes during perimenopause and menopause. Archer et al. They also claim that vasomotor symptoms during menopause are recorded in all regions of the world. However, the distribution of symptoms and the need for treatment varies significantly among women of different ethnic backgrounds and from different cultural backgrounds [12, 13]. Vasomotor symptoms are multidimensional and reflect a combination of heredity, diet, physical changes, medications, cultural influences, and individual experiences and expectations. [13]
Hot flashes can occur at any time of the day, they can be spontaneous or triggered by a variety of common factors such as embarrassment, sudden changes in ambient temperature, stress, alcohol, caffeine or any warm drink. Hot flashes usually begin with a sudden sensation of heat or warmth and are often accompanied by sweating, some redness of the skin, and sometimes a feeling of palpitations. The duration varies from 30 seconds to 60 minutes, with an average of 3 to 4 minutes [10].
For most women, hot flashes continue for more than 1 year and last about 4 years on average. Some women continue to experience hot flashes 20 years or more after their last menstrual period [2]. Hot flashes can interfere with work and daily activities, as well as sleep, causing subsequent fatigue, loss of concentration and symptoms of depression, which together interfere with family life, as well as sexual function and relationships between partners.
Mechanisms of the occurrence of tides
Dr. Archer et al. in their work they consider the modern theory of the pathogenesis of hot flashes.
Vasomotor symptoms result from disruption of thermoregulatory function in which normal heat dissipation mechanisms are inappropriately activated. It is generally accepted that the most important region of the brain for thermoregulatory balance is the preoptic area of the hypothalamus [14]. Core body temperature is usually maintained within the thermoneutral zone. When body temperature exceeds a certain limit, afferent pathways are activated in the preoptic zone, dilating blood vessels and increasing sweating [14-16]. When body temperature drops below a certain limit, peripheral blood flow is reduced and shivering occurs [17]. According to the current hypothesis, in women with vasomotor symptoms, the thermoneutral zone is significantly reduced, and afferent pathways are activated even with minor changes in core body temperature.
The most effective treatment for vasomotor symptoms is estrogen therapy. Estrogen is thought to correct the disruption of thermoregulatory function that occurs as a result of fluctuations and decreases in endogenous estrogen during the menopausal transition. Estrogen increases the sweat limit and expands the thermoneutral zone [18].
Scientific evidence suggests that serotonin and norepinephrine play an important role in the pathogenesis of vasomotor symptoms. Fluctuations in estrogen levels alter the levels of norepinephrine and/or serotonin involved in neurotransmission, leading to inappropriate sweating and hot flashes, characteristic of vasomotor symptoms [19-21]. Administration of estradiol results in an overall increase in the synthesis and availability of norepinephrine and serotonin, and also decreases the number, density, or sensitivity of receptors in animal models. Preclinical studies have shown that changes in monoamine neurotransmission can alter the limits of sweating and shivering and narrow the thermoneutral zone.
Hormone replacement therapy (HRT)
As noted by the authors of the paper “Hot flashes and night sweats in menopause: the current state of the issue,” hormonal therapy can effectively control hot flashes and many other common symptoms caused by menopause [22, 23]. Double-blind randomized controlled trials show that no other medical or alternative treatment provides greater relief of vasomotor symptoms than HRT. The effect develops within a month, and within 3 months therapy eliminates up to 90% of all vasomotor symptoms [24]. It is common clinical practice to adjust the dose of HRT to achieve greater effect and minimize side effects such as breast pain or uterine bleeding.
There is an increased risk of thromboembolism with oral HRT, but it has not yet been determined whether non-oral routes of administration such as patches and gels are associated with an increased risk. The type of progestin may also influence risk [25]. However, for those patients who have risk factors (eg, obesity or a history of thromboembolism), the use of non-oral HRT should be considered [6, 25].
There has not been extensive research into the long-term safety and effectiveness of so-called “bioidentical” or “natural” steroid hormones and should be avoided [6]. Locally produced “bioidentical” hormones are not subject to scrutiny by pharmaceutical regulators in many countries, and manufacturers may avoid having to test their products for quality, safety and effectiveness.
Selective estrogen receptor modulators
Selective estrogen receptor modulators (SERMs) have a broad spectrum of activity as estrogen receptor agonists or antagonists, depending on the level of expression of coregulator proteins present in the target tissue. As a class, all recent SERMs share the inability to suppress vasomotor symptoms and may even enhance them compared to placebo. In a recent report, more patients treated with bazedoxifene (23%) experienced hot flashes compared to placebo (6.6%). In most cases, hot flashes were mild or moderate in severity and did not lead to study discontinuation [26]. These results limit the use of SERMs to patients with severe vasomotor symptoms.
Bazedoxifene provides greater endometrial protection than other SERMs. This allows this drug to be used in conjunction with CEE to avoid the negative effects of estrogen on the endometrium and mammary glands, while at the same time suppressing vasomotor symptoms and maintaining normal vaginal health and normal bone mineral density [27].
Non-hormonal therapy for hot flashes
Although hormone replacement therapy is considered the gold standard for the treatment of hot flashes, it is associated with an increased risk of developing estrogen-related pathologies, including breast cancer, endometrial cancer, cardiovascular disease and thromboembolism, Dr. Stubbs notes in his work [11].
Patients with hot flashes who are either unable or unwilling to take HRT turn to non-hormonal treatments. Non-hormonal therapy includes non-pharmaceutical and pharmaceutical agents.
Non-pharmaceutical treatments
- Cognitive behavioral therapy. Psychological interventions for menopause aim to relieve symptoms by influencing behavior, understanding, cognition (memory, beliefs) or emotions [28]. Behavioral intervention techniques include paced breathing (slow, deep breathing), muscle relaxation, and biofeedback. A comparative study showed that paced breathing significantly reduced the frequency of hot flashes, but muscle relaxation and biofeedback did not have such an effect [29]. This effect of paced breathing was confirmed by the same researchers in a placebo-controlled study.
- Acupuncture. The effects of the method on vasomotor symptoms have been studied extensively, but the quality of the studies varies. Randomized controlled trials have found no evidence of effectiveness [30]. A multicenter randomized controlled trial of 267 women showed significant improvements in vasomotor, somatic, and sleep symptoms in women treated with acupuncture plus self-help counseling compared with self-help alone [31]. In summary, acupuncture may reduce menopausal symptoms, but robust clinical studies are needed.
- Blockade of the stellate ganglion. The stellate ganglion is a sympathetic ganglion located directly beneath the subclavian artery, and its intervention has various clinical applications. The ganglion is directly connected to the insular region of the brain, which has high activity during hot flashes [32]. A 12-week pilot study of 13 breast cancer patients experiencing severe hot flashes showed a significant and rapid reduction in the frequency of hot flashes, with very severe hot flashes reduced to virtually nothing. Complications associated with MH block include oculosympathetic paralysis (Horner's syndrome), the need for arterial or venous injection of anesthetic, pneumothorax, and vocal cord paralysis. Pulsed radiofrequency may provide more permanent damage to the stellate ganglion and is not associated with Horner's syndrome [33]. MH blockade may be useful for treating hot flashes in extreme cases where hormonal therapy is contraindicated.
- Yoga. A systematic study of yoga [34] in relation to menopausal symptoms showed that there is insufficient evidence to suggest that yoga is an effective treatment for menopause.
- Phytoestrogens. Large randomized controlled trials have not confirmed that phytoestrogens, red clover isoflavone, and black cohosh are superior to placebo in reducing hot flashes [35]. All major scientific, clinical, and women's health regulatory agencies do not recommend the prescription or use of these hormones.
Archer et al. Their paper summarizes that there is little evidence that changes in diet, acupuncture or exercise reduce hot flashes, but they may improve mood and quality of life. Regular exercise, weight loss, and eliminating triggers of hot flashes (such as caffeine or direct exposure to heat) can help minimize hot flashes and their impact [36]. Meditation, relaxation, controlled breathing, and cognitive behavioral therapy show promising results in reducing hot flashes. Recent level 1 evidence suggests that mindfulness-based therapy may be an effective and well-tolerated treatment for hot flashes [37].
Stubbs et al. confirm that, although potentially effective, non-pharmaceutical methods may not be the best option for women with severe hot flashes or those seeking immediate relief.
Placebo
Interestingly, the use of placebo for menopausal hot flashes has a fairly high subjective effectiveness. The work of Archer et al. reports the results of various studies, according to which the placebo effect ranges from 10 to 63% [35]. However, studies that used outpatient skin conductance sensors to objectively measure physiological hot flashes show that in outpatient settings, women underestimated their true number of hot flashes by 50% [38, 39]. This result calls into question the validity of patient-reported hot flashes as an indicator of the frequency of physiological hot flashes. Although subjective hot flashes may be considered to be more clinically significant than objective hot flashes, one clinical study reported improvements in quality of life, sleep, and fatigue only in women who experienced at least a 50% reduction in objective hot flashes [40].
Pharmaceutical non-hormonal treatments for hot flashes
Many women refuse to use HRT for hot flashes or have contraindications to HRT. Insufficient understanding of the mechanisms underlying menopausal vasomotor symptoms limits the development of new targeted treatments. Existing non-hormonal agents have come to the attention of clinicians due to anecdotal observations of a reduction in the severity of hot flashes as a “side” effect of a drug prescribed for other indications.
Prospective randomized controlled trials have shown that a number of drugs are superior to placebo in the treatment of vasomotor symptoms. In general, these drugs reduce the frequency and severity of hot flashes by 50–60%. This effectiveness is acceptable for most women who do not want to use hormones. In comparison, a standard dose of estrogen reduces hot flashes by 80–90% [10].
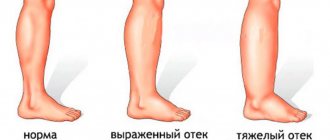
As reported by Stubbs et al., several nonestrogenic pharmaceutical or prescription medications have been considered for the treatment of hot flashes. These include the alpha-adrenergic agonist clonidine, the anticonvulsant gabapentin, selective serotonin reuptake inhibitors (SSRIs), and serotonin-norepinephrine reuptake inhibitors (SNRIs). Clonidine and gabapentin have shown some effectiveness, but each has serious side effects that may make them impractical for many women. Gabapentin causes dizziness, drowsiness, peripheral edema, loss of balance, and suicidal ideation. Side effects from clonidine are similar and include dizziness, sedation, and headache. SSRIs and SNRIs have shown promise in reducing both the frequency and severity of hot flashes without the serious risks associated with HRT or the more serious side effects of other prescription medications studied.
Clinical efficacy of SSRIs and SSRIs in the treatment of vasomotor symptoms
In the work “Hot flashes and night sweats in menopause: the current state of the issue,” D. F. Archer et al. present the results of recent studies of the use of SSRIs, SNRIs and gabapentin to reduce the frequency and severity of vasomotor symptoms [41].
- Prospective, randomized, placebo-controlled trials assessed the effectiveness of the SNRI desvenlafaxine and the results were submitted for regulatory approval [42–44]. With desvenlafaxine 100 mg/day, a 65% reduction in the incidence of vasomotor symptoms was observed at 12 weeks. Of the 75% of patients who achieved remission and improvement, 50% were on desvenlafaxine compared with 29% on placebo, which was statistically significant [43].
- A small comparative study of subcutaneous gabapentin and estradiol found that both drugs reduced the frequency of hot flashes, with no difference between the two study arms [45]. Gabapentin (300 mg three times daily) was as effective as low-dose estrogen in reducing the frequency and severity of vasomotor symptoms. Venlafaxine extended release (75 mg) was not directly compared with estrogen, but was as effective as gabapentin in treating vasomotor symptoms and was better tolerated in one crossover study [46].
- In one prospective study [47], fluoxetine and citalopram did not reduce hot flashes compared with placebo, while in another study [48], paroxetine, venlafaxine, fluoxetine, and sertraline were more effective than placebo.
Drugs that affect serotonin and norepinephrine levels in the brain have demonstrated modest effects on vasomotor symptoms. Desvenlafaxine, which is approved in Mexico and Thailand for the treatment of vasomotor symptoms at a dose of 100 mg/day, is recommended to titrate with a gradual increase in dose to minimize adverse events (nausea, vomiting, dizziness) in the first week after initiation of therapy and with a decrease in dose to minimize withdrawal symptoms (anxiety, depression and sudden mood swings).
The authors of the paper “Do SSRIs and SNRIs Reduce the Frequency and/or Severity of Hot Flashes in Menopause” by Chris Stubbs cite the results of several large-scale reviews:
In 2013, Shams et al. published a systematic review and meta-analysis assessing the effectiveness of five SSRIs—escitalopram, paroxetine, sertraline, citalopram, and fluoxetine—for reducing vasomotor symptoms (hot flashes) in healthy perimenopausal women. An analysis of 11 randomized controlled trials (RCTs) involving a group of 2069 women aged 36 to 76 years showed that treatment with SSRIs led to a significant reduction in the average number of daily hot flashes over 4-8 weeks from 10 per day to 9 compared with placebo. In this study, escitolapram was the most effective SSRI for reducing the daily frequency of hot flashes. The researchers concluded that SSRIs are a reasonable replacement for HRT. [49]
A 2015 systematic review by Handley and Williams analyzed 18 RCTs examining the effectiveness of SSRIs/SNRIs compared with placebo. Participants were healthy women aged 27 to 78 years who reported experiencing an average of 46 to 76 hot flashes per week. SSRIs/SSRIs reduced hot flash symptoms by 65% compared with placebo. Potential first-line SSRIs included paroxetine, extended-release paroxetine, citalopram and escitalopram). Venlafaxine has been identified as a potential first-line SNRI. Extended-release paroxetine showed the greatest statistically significant reduction in hot flashes. Venlafaxine provided more rapid symptom relief than SSRIs, but had a higher incidence of side effects , most notably nausea and constipation. [50]
In 2015, the North American Menopause Society (NAMS) published a statement on non-hormonal management of vasomotor symptoms associated with menopause [23]. Team members searched five databases for high-quality evidence articles (RCTs or systematic reviews) on non-hormonal treatments for hot flashes. One such study reported that the SNRI venlafaxine extended-release formulation demonstrated similar efficacy to low-dose estradiol in reducing vasomotor symptoms. After assessing the evidence, the NAMS panel concluded that non-hormonal treatments are appropriate treatments for hot flashes in menopause and postmenopause.
NAMS recommendations include the following SSRIs and SNRIs: paroxetine salt 7.5 mg/day; paroxetine or delayed-release paroxetine 10-25 mg/day; escitalopram 10-20 mg/day; citalopram 10-20 mg/day; desvenlafaxine 50-150 mg/day; and venlafaxine in extended-release form 37.5–150 mg/day. Paroxetine salt is only available in a 7.5 mg dosage and is currently the only FDA-approved medication for hot flashes [23].
Women with a history of breast cancer taking tamoxifen should avoid SSRIs. Studies have shown that some SSRIs inhibit the activity of the CYP2D6 enzyme, which may result in decreased therapeutic levels of tamoxifen. The SNRIs venlafaxine and desvenlafaxine appear to have little or no effect on the activity of tamoxifen and should be considered as first-line therapy in these patients. [eleven]
Conclusion
Vasomotor symptoms occur in all women, regardless of their cultural and ethnic background, and often negatively affect the quality of life of patients.
HRT is still considered the most effective treatment for reducing hot flashes in menopausal and postmenopausal women. However, concerns that hormonal therapy may increase the risk of estrogen-related pathologies have led to research into the possibility of using other agents to treat this pathology. Non-pharmaceutical methods and some pharmaceutical drugs, in particular the SERM group, do not convincingly demonstrate their effectiveness.
SSRIs and SNRIs reduce the frequency and severity of vasomotor symptoms associated with menopause by 10% to 64%, depending on the study. Side effects from SSRIs and SNRIs, including nausea, constipation and dry mouth, were not severe and often resolved within the first week. [4, 23]
From the SSRI group, escitalopram and prolonged-release paroxetine show the greatest activity, from the SNRI group - venlafaxine in a prolonged form.
Although SSRIs and SNRIs are less effective than HRT, they significantly reduce the frequency and severity of hot flashes and may be recommended for women who are not willing to accept the risks of hormonal therapy. Additional placebo-controlled studies are needed to evaluate benefits, safety, and dosing in more detail.
Literature:
- Voda AM. Climacteric hot flash. Maturitas 1981;3:73–90
- Politi MC, Schleinitz MD, Col NF. Revisiting the duration of vasomotor symptoms of menopause: a meta-analysis. J Gen Intern Med 2008; 23:1507-13
- Freedman RR. Menopausal hot flashes: mechanisms, endocrinology, treatment. J Steroid Biochem Mol Biol. 2014; 142:115–20. [PubMed: 24012626]
- Imai A, Matsunami K, Takagi H, Ichigo S. New generation nonhormonal management for hot flashes. Gynecol Endocrinol. 2013; 29(1):63–6. [PubMed: 22809093]
- Santen RJ, Allred DC, Ardoin SP, et al. Postmenopausal hormone therapy: an Endocrine Society scientific statement. J Clin Endocrinol Metab 2010;95:s1–66
- Sturdee DW, Pines A, on behalf of the International Menopause Society Writing Group. Updated IMS recommendations on postmenopausal hormone therapy and preventive strategies for midlife health. Climacteric 2011;14:302–20
- LaCroix AZ, Chlebowski RT, Manson JE, et al. Health outcomes after stopping conjugated equine estrogens among postmenopausal women with prior hysterectomy: a randomized controlled trial. JAMA 2011;305:1305–14
- Rossouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women's Health Initiative randomized controlled trial. JAMA 2002;288:321–33
- Gupta P, Sturdee DW, Palin SL, et al. Menopausal symptoms in women treated for breast cancer: the prevalence and severity of symptoms and their perceived effects on quality of life. Climacteric 2006;9:49–58
- Archer DF, Sturdee DW, Baber R, et al. Menopausal hot flushes and night sweats: where are we now?. Climacteric. 2011;14(5):515-528. doi:10.3109/13697137.2011.608596
- Stubbs, Chris & Mattingly, Lisa & Crawford, Steven & Wickersham, Elizabeth & Brockhaus, Jessica & McCarthy, Laine. (2017). Do SSRIs and SNRIs reduce the frequency and/or severity of hot flashes in menopausal women. The Journal of the Oklahoma State Medical Association. 110. 272-274.
- Freeman EW, Sherif K. Prevalence of hot flushes and night sweats around the world: a systematic review. Climacteric 2007;10:197–214
- Palacios S, Henderson VW, Siseles N, Tan D, Villaseca P. Age of menopause and impact of climacteric symptoms by geographical region. Climacteric 2010;13:419–28
- Romanovsky A.A. Thermoregulation: some concepts have changed. Functional architecture of the thermoregulatory system. Am J Physiol Regul Integr Comp Physiol 2007;292:R37–46
- Boulant JA. Role of the preoptic-anterior hypothalamus in thermoregulation and fever. Clin Infect Dis 2000;31(Suppl 5):S157–61
- Zhang YH, Yamada K, Hosono T, Chen XM, Shiosaka S, Kanosue K. Efferent neuronal organization of thermoregulatory vasomotor control. Ann NY Acad Sci 1997;813:117–22
- Charkoudian N. Skin blood flow in adult human thermoregulation: how it works, when it does not, and why. Mayo Clin Proc 2003;78:603–12
- Freedman RR, Blacker CM. Estrogen raises the sweating threshold in postmenopausal women with hot flashes. Fertil Steril 2002;77:487–90
- Berendsen HH. The role of serotonin in hot flushes. Maturitas 2000;36:155–64
- Quan N, Xin L, Blatteis CM. Microdialysis of norepinephrine into preoptic area of guinea pigs: characteristics of hypothermic effect. Am J Physiol 1991;261:R378–85
- Freedman RR. Pathophysiology and treatment of menopausal hot flashes. Semin Reprod Med 2005;23:117–25
- MacLennan AH. Evidence-based review of therapies at the menopause. Int J Evid Based Healthc 2009;7:112–23
- Nonhormonal management of menopause-associated vasomotor symptoms: 2015 position statement of The North American Menopause Society. Menopause. 2015; 22(11):1–18. [PubMed: 25490113]
- MacLennan AH, Broadbent JL, Lester S, Moore V. Oral oestrogen and combined oestrogen/progestogen therapy versus placebo for hot flushes. Cochrane Database of Systematic Reviews (Online) 2004:CD002978
- Olié V, Canonico M, Scarabin PY. Postmenopausal hormone therapy and venous thromboembolism. Thromb Res 2011;127(Suppl 3):S26–9
- de Villiers TJ, Chines AA, Palacios S, et al. Safety and tolerability of bazedoxifene in postmenopausal women with osteoporosis: results of a 5-year, randomized, placebocontrolled phase 3 trial. Osteoporos Int 2011;22:567–76
- Lobo RA, Pinkerton JV, Gass ML, et al. Evaluation of bazedoxifene/conjugated estrogens for the treatment of menopausal symptoms and effects on metabolic parameters and overall safety profile. Fertil Steril 2009;92:1025–38
- Towey M, Bundy C, Cordingley L. Psychological and social interventions in the menopause. Curr Opin Obstet Gynecol 2006;18:413–17
- Freedman RR, Woodward S. Behavioral treatment of menopausal hot flushes: evaluation by ambulatory monitoring. Am J Obstet Gynecol 1992;167:436–9
- Lee MS, Shin BC, Ernst E. Acupuncture for treating menopausal hot flushes: a systematic review. Climacteric 2009;12:16–25
- Borud EK, Alraek T, White A, et al. The acupuncture on hot flushes among menopausal women (ACUFLASH) study, a randomized controlled trial. Menopause 2009;16:484–93
- Freedman RR, Benton MD, Genik RJ, et al. Cortical activation during menopausal hot flashes. Fertil Steril 2006;85:674–678
- van Boxem K, van Eerd M, Brinkhuize T, et al. Radiofrequency and pulsed radiofrequency treatment of chronic pain syndromes: the available evidence. Pain Pract 2008;8:385–93
- Lee MS, Kim JI, Ha JY, Boddy K, Ernst E. Yoga for menopausal symptoms: a systematic review. Menopause 2009;16:602–8
- Geller SE, Shulman LP, van Breemen RB, et al. Safety and efficacy of black cohosh and red clover for the management of vasomotor symptoms: a randomized controlled trial. Menopause 2009;16:1156–66
- Borrelli F, Ernst E. Alternative and complementary therapies for the menopause. Maturitas 2010;66:333–43
- Carmody JF, Crawford S, Salmoirago-Blotcher E, Leung K, Churchill L, Olendzki N. Mindfulness training for coping with hot flashes: results of a randomized trial. Menopause 2011;18:611–20
- Carpenter JS, Elam JL, Ridner SH, Carney PH, Cherry GJ, Cucullu HL. Sleep, fatigue, and depressive symptoms in breast cancer survivors and matched healthy women experiencing hot flashes. Oncol Nurs Forum 2004;31:591–8
- Carpenter J, Azzouz F, Monahan P, Storniolo A, Ridner S. Is external skin conductance monitoring a valid measure of hot flash intensity or distress? Menopause 2005;12:512–19
- Carpenter JS, Storniolo AM, Johns S, et al. Randomized, double-blind, placebocontrolled crossover trials of venlafaxine for hot flashes after breast cancer. Oncologist 2007;12:124–35
- Albertazzi P. Non-estrogenic approaches for the treatment of climacteric symptoms. Climacteric 2007;10(Suppl 2):115–20
- Archer DF, Seidman L, Constantine GD, Pickar JH, Olivier S. A double-blind, randomly assigned, placebo-controlled study of desvenlafaxine efficacy and safety for the treatment of vasomotor symptoms associated with menopause. Am J Obstet Gynecol 2009;200:172 e1–10
- Speroff L, Gass M, Constantine G, Olivier S. Efficacy and tolerability of desvenlafaxine succinate treatment for menopausal vasomotor symptoms: a randomized controlled trial. Obstet Gynecol 2008;111:77–87
- Archer DF, Dupont CM, Constantine GD, Pickar JH, Olivier S. Desvenlafaxine for the treatment of vasomotor symptoms associated with menopause: a double-blind, 35 randomized, placebo-controlled trial of efficacy and safety. Am J Obstet Gynecol 2009;200:238 e1–10
- Aguirre W, Chedraui P, Mendoza J, Ruilova I. Gabapentin vs. low-dose transdermal estradiol for treating post-menopausal women with moderate to very severe hot flushes. Gynecol Endocrinol 2010;26:333–7
- Loprinzi CL, Sloan J, Stearns V, et al. Newer antidepressants and gabapentin for hot flashes: an individual patient pooled analysis. J Clin Oncol 2009;27:2831–7
- Suvanto-Luukkonen E, Koivunen R, Sundstrom H, et al. Citalopram and fluoxetine in the treatment of postmenopausal symptoms: a prospective, randomized, 9-month, placebocontrolled, double-blind study. Menopause 2005;12:18–26
- Loprinzi CL, Sloan J, Stearns V, Iyengar M, et al. Newer antidepressants and gabapentin for hot flashes: an individual patient pooled analysis. J Clin Oncol 2009;27:2831– 7
- Shams T, Firwana B, Habib F, et al. SSRIs for hot flashes: a systematic review and meta analysis of randomized trials. J Gen Intern Med. 2013; 29(1):204–13. [PubMed: 23888328]
- Handley A, Williams M. The efficacy and tolerability of SSRI/SNRIs in the treatment of vasomotor symptoms in menopausal women: a systematic review. J Am Assoc Nurse Pract. 2015; 27(1):54–61. [PubMed: 24944075]
Menopause without hot flashes: reality or dream?
Unfortunately, most women experience the unpleasant symptoms of menopause firsthand. However, each of them has a choice: to come to terms with the manifestations of this condition or to alleviate it by taking the right medications.
One of the best remedies for hot flashes during menopause is Klimafemin.
This drug was developed by specialists from the pharmaceutical company VERTEX and has the necessary documents and certificates. The product is distinguished by a balanced composition, which includes natural components: phytoestrogen genistein, coenzyme Q10, grape seed extract and vitamin E. As a result of the use of “Climafemin”, the frequency and intensity of hot flashes decreases, sweating decreases, and the emotional background improves. Sources:
- Menopausal syndrome. Smetnik V.P., Tkachenko N.M., Glezer G.A. and others // M. - 1988. - P. 286.
- Depressive disorders in peri- and postmenopausal women. Yureneva S.V., Kamenetskaya T.Ya. // Journal of gynecology. - 2007. - 9(2). pp. 5-12.
- Mental disorders in women during menopause. Tyuvina N.A. // M.: Kronpress. - 1996. - P. 237.
- https://cyberleninka.ru/article/n/myagkiy-klimaks
- https://cyberleninka.ru/article/n/ispolzovanie-bad-dlya-korrektsii-klinicheskih-proyavleniy-perimeno…
- https://cyberleninka.ru/article/n/sovremennye-podhody-k-diagnostike-prognozirovaniyu-techeniya-i-lec…
How does andropause affect the reproductive system?
A decrease in testosterone levels primarily affects the reproductive system:
- Decreased libido. Testosterone is the driving force of sexual desire. If the level of this hormone drops, then the desire for intimacy also fades away.
- Weakening of erection. Low testosterone levels lead to decreased blood supply to the male reproductive organ.
- Testicular atrophy. The testicles decrease in size, lose their ability to contract, and the process of sperm production is disrupted.
- Deterioration in sperm quality. A decrease in the concentration of the hormone leads to a decrease in sperm volume and quality, and the number and motility of sperm decreases.
The result of this is depression, loss of strength, and problems with fertility, that is, the ability to conceive a child.
Popular questions
Hello!
Constant hot flashes tormented me. I started drinking Gynocomfort Klimafemin. It helped right away. But it turned out that it was not available in any pharmacy! It was difficult to buy only one package. Has this product been discontinued? Hello! Gynocomfort climafemin continues to be produced. You can purchase it in pharmacies that sell other VERTEX products.
Hello, I have up to 10 hot flashes per day, more at night. A year ago I took the drug Femoston 2 for three months, it helped, everything was fine for six months, but it all started again. Is it possible to correct this condition without hormonal drugs?
Hello! The Ginocomfort line of drugs includes the drug Climafemin. It contains antioxidants and phytoestrogens, which will correct the vegetative manifestations of menopause. If there is no effect after 1 month of use, you should consult your doctor again.
Hot flashes, insomnia, what to do? I take Klimanalin, it doesn’t help.
Hello! Vivid vegetative manifestations in the menopause are caused not only by hormonal changes, but also by a possible combination of thyroid pathology - hypothyroidism, vertebrobasilar insufficiency. Therefore, it is advisable: consultation with an endocrinologist or neurologist. OMT ultrasound, flora smear, cytology, which will allow prescribing menopausal hormone therapy in the absence of contraindications. At this stage, pending examination results, you can add Gynocomfort climafemin to treatment. The drug contains phytoestrogens and antioxidants, which has a beneficial effect on well-being and eliminates the symptoms of menopause. The drug is taken 1 t once a day for 3 months.
I am 49 years old and suffered from frequent hot flashes. How to prevent them?
Hello!
These are manifestations of menopausal syndrome associated with the extinction of ovarian function. At this stage, I recommend using a herbal-based drug that allows you to stop bursts of vegetative reactions - Ginocomfort Klimafemin 1 t once a day for 3 months. During this time, conduct an examination: ultrasound OMT, they say. glands, flora smear, oncocytology, oak, lipid spectrum, FSH, TSH levels. Consult a therapist and other related specialists if you have chronic diseases that would be a contraindication for prescribing menopausal hormone therapy. This will help the obstetrician-gynecologist correctly select further treatment. For an accurate diagnosis, contact a specialist
Interpretation of results
Although "double the risk" sounds scary, the overall increase in heart risk in women associated with hot flashes remained relatively low.
So what should women take away from this discovery? Dr. Rexrode recommends taking heart health seriously and using menopause as a time to reassess your risks. She recommends the following important steps:
Identify your risk factors.
Dr. Rexrode noted that it is always important to review risk factors for cardiovascular disease in midlife. The likelihood of a heart attack or stroke increases in women during and after menopause. Although researchers have found a link between hot flashes and heart risks, it is too early to do anything with this information. Instead, women should continue to focus on established risk factors for cardiovascular disease, such as high cholesterol, high blood pressure and diabetes.
Let's look at some risk factors for women only.
Dr. Rexrode. identified the following two factors:
- early menopause (before 40 years)
- an episode of preeclampsia (a potentially life-threatening complication of pregnancy accompanied by high blood pressure and protein in the urine).
If you're not at high risk for heart disease, but you have one or both of these factors, it may increase your risk level, she says. “Additional risk factors include other pregnancy complications, gestational diabetes and hot flashes.” If additional evidence becomes available, it may be added to this list.
Hot flashes are common during menopause, but frequent or persistent episodes may be a sign of a higher risk of heart attack or stroke.
Scientists are paying more attention to women-specific risk factors for heart disease, and in the coming years, more will be known about how these factors can affect your health.
Causes of menopause
This condition is considered physiological and occurs due to natural age-related changes.
The fact is that, unlike male sperm, the number of eggs that mature in a woman’s ovaries is limited and is determined at birth. With each menstrual cycle there are fewer and fewer of them. When there are no eggs left, pregnancy becomes impossible, and the body “turns off” the functions responsible for conceiving and carrying a child. In addition, the ovaries stop producing estrogen, which is responsible for egg implantation and prepares the uterine vessels for feeding the fetus. Due to hormonal changes that occur during menopause, the thickness of the endometrium (the inner mucous layer of the uterus) becomes smaller, as a result of which a woman loses the ability to bear a pregnancy.
This physiological process may speed up. Risk factors for early menopause include an unhealthy lifestyle, intense physical activity, chronic stress, chronic endocrine diseases (diabetes mellitus, hypothyroidism), unfavorable environment, hereditary predisposition, rare sex life, excess weight, poor nutrition and diets.
Menopause in men (andropause) is characterized by a decrease in the production of the male sex hormone - testosterone. The age of its onset also occurs at 45-50 years, and the duration ranges from 2 to 5 years. Childbearing function, like that of women, fades away.