About the operation
A pacemaker is a small device (artificial pacemaker) that creates electrical impulses and sends them to the chambers of the heart, forcing them to contract in a certain order, synchronizing the work of the atria and ventricles. A pacemaker eliminates the slow rhythm of the heart and prevents it from stopping.
The device consists of a generator and electrodes. The generator generates electrical impulses. The electrodes conduct impulses from the generator to the chambers of the heart that need to be influenced. Depending on the pacemaker, there can be from one to three electrodes. The device weighs 30-50 grams, is equipped with a battery and a microcircuit. It is installed by an arrhythmologist surgeon through a small incision in the upper chest. The case is made of titanium coating, so the risk of rejection is minimal. All information from the ECS is sent to the desktop computer of the medical institution where the device was installed. With its help, the doctor monitors the patient’s well-being, the work of the pacemaker, and, if necessary, makes changes in the device settings.
There are several types of pacemakers:
- Single-chamber – controls and stimulates only one chamber of the heart (atrium or ventricle). Not able to imitate the physiological contraction of the heart muscle;
- Dual-chamber – connects the generator through electrodes simultaneously to the atrium and ventricle. When the need for stimulation arises, the generator sequentially directs impulses from the atrium to the ventricles, restoring normal myocardial contraction;
- Three-chamber – designed to synchronize the ventricles of the heart. Electrodes are directed into the right atrium and both ventricles. Mainly used in the treatment of chronic heart failure.
According to the functionality of the EX, they are distinguished:
- Pacemakers – set the heart the correct rhythm;
- Defibrillators-cardioverters - in addition to imposing the correct rhythm, can stop attacks of arrhythmia and ventricular fibrillation.
Modern pacemakers operate on an on-demand basis. The device automatically monitors heart rate. If the heart rate is normal, the device does not send pulses. In case of a prolonged pause (above a threshold value), the device sends a signal to the myocardium.
There are also temporary pacemakers that are used for life-threatening conditions. In such a situation, the generator is not sewn under the skin, but is located outside the patient’s body. Also, a temporary pacemaker can be used until a permanent pacemaker is installed or to relieve an attack that may disappear (for example, with a drug overdose). The procedure is carried out only in a hospital under the constant supervision of specialists.
In some cases, installing an pacemaker is the only way to save the patient’s health and life.
Normally, the regular contractions of our heart are supported by special cells that form the sinus node. This structure is located at the top of the right atrium. (Fig. 1)
Figure 1 Normal formation and propagation of electrical impulses
In some cases, the normal functioning of the heart may be disrupted; patients may experience an irregular, fast or slow pulse, pauses between contractions. All this is called heart rhythm disturbance or arrhythmia.
There are several types of arrhythmia:
Supraventricular rhythm disturbances:
- Atrial fibrillation and flutter
- Supraventricular paroxysmal tachycardia
- Atrial extrasystole
Ventricular arrhythmias:
- Ventricular extrasystole
- Ventricular tachycardia
What is paroxysmal tachycardia?
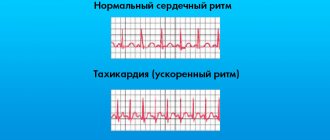
Under normal conditions, the normal heart rate is between 60 and 100 beats per minute. A heart rate greater than 100 beats per minute is called tachycardia.
With paroxysmal tachycardia, a sudden attack (paroxysm) of rapid heartbeat occurs, usually unrelated to physical activity.
Figure 2 Paroxysm of supraventricular tachycardia with a frequency of 180 bpm.
Paroxysm of tachycardia is a regular heartbeat with a frequency of usually 150 to 200 beats per minute, which is accompanied by weakness and shortness of breath. (Fig. 2) Sometimes patients may lose consciousness. In some patients, these episodes are short-lived and are not accompanied by significant symptoms.
How does extrasystole manifest?
An extrasystole is a premature contraction of the heart, which is felt by patients as a short-term interruption in the work of the heart, after which there may be a short pause followed by the restoration of a rhythmic heartbeat.
Treatment of arrhythmias
Both medicinal and surgical treatment methods are used to treat various types of arrhythmias. Among surgical treatment methods, the most common is catheter ablation.
What is ablation?
Catheter ablation is a minimally invasive operation that eliminates the “source” of arrhythmia using radiofrequency energy (RFA) or local cooling of heart tissue (cryoablation).
The emergence of catheter ablation techniques was the result of intensive development of science and the emergence of new medical technologies over the past 20 years.
Today, the catheter ablation method is widespread throughout the world (more than 1 million operations annually) and is the only treatment method that can radically eliminate a significant portion of cardiac arrhythmias in humans.
Types of catheter ablations
Most often in clinical practice, ultrahigh frequency (radio) frequency current is used - 500 kHz. This type of ablation is called radiofrequency catheter ablation (RFA). The effects of radiofrequency energy are carried out using special controlled catheters installed in the heart under X-ray control. (Fig. 3)
Figure 3 Placement of catheters in the heart during RFA.
Another type of impact on the source of arrhythmia is based on rapid, deep and local cooling of the heart tissue. This type of catheter ablation is called catheter cryoablation. Most often, catheter cryoablation is used to treat atrial fibrillation; a special cryoballoon catheter is used for this purpose. This type of surgery is called catheter balloon cryoablation. (Fig. 4)
Figure 4 Balloon placement in the left atrium during cryoablation.
What types of arrhythmias can be treated with catheter ablation?
All rhythm disturbances in humans are usually divided depending on the location of the “source” of arrhythmia in the human heart into “supraventricular” and “ventricular”. The cause (etiology) of arrhythmias in humans can be various pathological effects on the heart (inflammation, ischemia, etc.), or they can be caused by congenital features (anomalies) of heart development, incl. conduction system of the heart. Often it is not possible to detect the cause of arrhythmia. Such rhythm disturbances (in the absence of other heart diseases) are called “idiopathic”. The catheter ablation method allows in most cases to effectively eliminate arrhythmias that differ in both etiology and development mechanisms.
Benefits of Catheter Ablation
Treatment of heart rhythm disorders can be medication or interventional (surgical). It should be borne in mind that drug treatment involves long-term, often lifelong, antiarrhythmic drugs. Stopping medication or reducing the dose creates conditions for relapse of the arrhythmia. In addition, the use of medications is often impossible due to side effects or contraindicated due to the presence of concomitant heart diseases.
Currently, international and domestic recommendations for the treatment of cardiac arrhythmias consider catheter ablation as the main method of treating a significant part of arrhythmias. Such recommendations are based on the fact that catheter ablation can eliminate arrhythmia without further resorting to the use of antiarrhythmic drugs.
According to the guidelines, ablation is recommended in the following cases:
— as the main method of treatment for arrhythmias, where the use of catheter ablation is accompanied by high efficiency and safety (supraventricular tachycardia, atrial flutter)
-as an alternative treatment, usually when drug therapy is ineffective or side effects of antiarrhythmic drugs develop (atrial fibrillation, ventricular arrhythmias)
About catheter ablation
Preparation
Before performing RFA, the department performs the necessary examination (blood tests, instrumental diagnostic methods) for, as a rule, 2-3 days. On the day of surgery, the patient does not have breakfast; immediately before the operation, he puts on compression stockings (antithromboembolic stockings or elastic bandages).
RFA is performed by interventional arrhythmologists in a cath lab equipped with modern equipment for diagnostics and interventional treatment.
Ablation procedure
As the first stage of the operation, the so-called intracardiac electrophysiological study (ICE), the purpose of which is to clarify the type of tachyarrhythmia and search for the source of the arrhythmia. (Fig.3 and Fig.4)
To do this, a puncture of the vessels (femoral vein and, if necessary, artery) is performed, and special diagnostic electrodes are carried out under X-ray control. When performing VEPI, electrical stimulation of the heart of various parts of the heart is performed in accordance with diagnostic algorithms. This allows you to establish an accurate diagnosis and determine the location of the source of the arrhythmia.
In some cases (with atrial fibrillation), inhalation anesthesia is used as an anesthetic aid; in other cases, local anesthesia is used.
The duration of the operation is determined by its volume and takes from 1.5 to 3 hours.
After ablation
After RFA, a pressure bandage is applied to the puncture site of the vessel and the patient is transferred to the postoperative ward, where he is under the supervision of an anesthesiologist-resuscitator for at least 12 hours. All this time the patient is on strict bed rest.
To exclude possible complications after RFA, all patients undergo a comprehensive postoperative examination.
On average, the hospitalization period for RFA does not exceed 5 days.
Safety and effectiveness
The effectiveness of catheter ablation, depending on the type of arrhythmia, ranges from 70 to 99%. The risk of potential complications after surgery usually does not exceed 1%, but can reach 4-5% for the most complex heart rhythm disorders. The decision to carry out interventional treatment in each case is made by our specialists, taking into account the patient’s opinion, based on full information about the benefits and potential risks of surgical treatment.
Catheter ablation of atrial fibrillation
What is Atrial Fibrillation?
With atrial fibrillation (atrial fibrillation), instead of a regular heart rhythm, multiple electrical waves occur in the atria, leading to chaotic contractions of both atria at a very high frequency. [Rice. 5]
Figure 5. Atrial fibrillation
Atrial fibrillation (atrial fibrillation), as a rule, is manifested by a rapid, irregular heart rhythm, shortness of breath, and poor exercise tolerance. Often, atrial fibrillation is asymptomatic and is discovered accidentally during ECG recording.
Often, patients with atrial fibrillation (atrial fibrillation) are found to have another type of heart rhythm disorder - atrial flutter. [Fig.6]
Figure 6. Typical atrial flutter.
The symptoms of atrial flutter are not much different from atrial fibrillation. The exact diagnosis of these rhythm disturbances and treatment tactics should be determined by a cardiologist-arrhythmologist.
Why and how to treat atrial fibrillation?
Treatment of atrial fibrillation aims to: 1) eliminate the symptoms of arrhythmia, i.e. improving the quality of life of patients; 2) eliminating the threat of developing heart failure; 3) prevention of thromboembolic complications.
According to world medical statistics, atrial fibrillation (atrial fibrillation) is the most common (1-2% in the population) heart rhythm disorder. In a significant proportion of patients (up to 40%), AF is asymptomatic. In this category of patients, drug antiarrhythmic or non-drug treatment (catheter ablation) for AF is usually not carried out. Treatment of these patients consists of monitoring heart rate and administering anticoagulants to prevent thromboembolic complications.
Patients in whom atrial fibrillation is accompanied by the symptoms described above are prescribed continuous antiarrhythmic therapy aimed at preventing relapses of AF. In approximately one third of all patients with AF, it is possible to select an effective antiarrhythmic drug or their combination.
In 30% of patients with symptomatic, poorly tolerated atrial fibrillation, it is not possible to select effective antiarrhythmic therapy, or the use of antiarrhythmic drugs is contraindicated, is accompanied by the development of side effects, or patients do not want to adhere to long-term conservative drug treatment. In this category of patients, in accordance with modern international and Russian recommendations, catheter ablation is indicated.
It should be emphasized that the choice of treatment options in each specific case is the task of a cardiologist-arrhythmologist, taking into account the patient’s opinion and objective medical data.
Catheter and surgical ablation
Depending on the form of atrial fibrillation (paroxysmal, persistent or permanent), the presence of other pathologies of the cardiovascular system and concomitant diseases, 3 types of catheter (or surgical) ablation are used:
Intracardiac catheter ablation is the most widely used non-drug treatment for AF. Catheter ablation is performed in a cath lab using guided catheters moved into the chambers of the heart through vascular access (femoral and subclavian veins). The purpose of the operation is to radically eliminate the “sources” of arrhythmia in the left and (with atrial flutter) right atrium. Currently, two types of catheter ablation have found widespread clinical use: radiofrequency catheter ablation and balloon cryoablation.
· catheter ablation (destruction) of the AV node is a type of intracardiac catheter ablation, which is used in cases where AF is accompanied by a persistently high heart rate when drug control or radical elimination of AF is impossible. Ablation of the AV node is performed only after implantation of an artificial pacemaker (pacemaker).
· Operation “Labyrinth” – surgical ablation of AF. The “maze” operation (MAZE) is used in cases where a patient with AF is indicated for open-heart surgery due to the presence of an “underlying” heart disease: coronary artery bypass surgery, valve replacement, etc. As an independent intervention for AF, the “labyrinth” operation is used in the form of modified minimally invasive operations with thoracoscopic access (through a small incision in the chest) and only if previously performed attempts at catheter ablation are ineffective.
RFA or cryoablation?
According to modern concepts, the key role in the development of AF belongs to the so-called “arrhythmogenic” pulmonary veins (so-called AF triggers) - large vessels flowing into the left atrium. [Fig.7]
Figure 7. Left atrium and pulmonary veins. Multislice computed tomography
That is why most patients with paroxysmal and persistent forms of atrial fibrillation are indicated for catheter ablation (isolation) of the pulmonary veins.
How it works?
With radiofrequency catheter ablation, isolation of the pulmonary veins is achieved by applying a large number of targeted effects using high-frequency current. These effects should form a continuous chain of many sequential coagulative necrosis around each of the veins [Fig. 8A]. When using another technology - balloon cryoablation [video 1], a zone of necrosis around the veins is created due to the effect of low temperature (up to - 60ºC) in a cryoballoon located sequentially in each of the mouths of the pulmonary veins [Fig. 8B].
Rice. 8A - Radiofrequency catheter ablation (RFA); 1-circular diagnostic electrode of the “Lasso” type, 2-catheter for RFA
Rice. 8B — Catheter balloon cryoablation: 3- cryoballoon
Video 1. Balloon cryoablation.
In most cases, complete isolation is achieved with a single cryo-exposure for several minutes, which is an absolute advantage over radiofrequency ablation. Both types of catheter ablations are performed in a cath lab under general anesthesia or deep sedation. These interventions are high-tech types of medical care and should be performed by qualified specialists with sufficient experience in interventional interventions.
Efficiency and safety
The generally accepted definition of the effectiveness of catheter ablation for AF is the absence of any atrial arrhythmias after surgery without the use of antiarrhythmic drugs. Monitoring of effectiveness is carried out clinically (patient self-monitoring) or using long-term ECG recording systems (HM ECG or special implantable heart rate recorders).
One of the main factors determining the effectiveness of catheter ablation for AF is the duration of episodes of fibrillation. In cases where attacks of arrhythmia do not exceed several hours or days (the so-called paroxysmal form) and, as a rule, go away on their own, the operation is most effective. In comparative studies (the international Fire and Ice study), there were no relapses of AF during the first year in 65% of patients both after RFA and after balloon cryoablation. At the same time, there are observations that in individuals without concomitant cardiac pathology, the effectiveness of balloon cryoablation can reach 80-90%.
In patients with persistent AF, i.e. with arrhythmia lasting more than 7 days, and also requiring drug or electrical cardioversion to restore sinus rhythm, the expected effectiveness of catheter ablation is about 50-60%.
If, after catheter ablation, AF recurs with the same frequency and duration, re-intervention is justified.
Complications during catheter ablation of AF can manifest themselves in the form of vascular damage at the puncture site, perforation of the heart wall with the development of tamponade, the formation of blood clots in the heart cavity and thromboembolic complications, thermal damage to the esophagus, the development of phrenic nerve paresis and a number of others. The use of modern high-tech control methods during intracardiac interventions, sufficient experience and qualifications of the doctor allows these interventions to be performed effectively and without a significant risk of complications.
At the same time, it is necessary to clearly understand that the decision to carry out interventional treatment for AF should be made by a doctor with sufficient experience in treating this category of patients, objectively taking into account the pros and cons.
Catheter ablation of AF in the Department of Clinical Electrophysiology and X-ray Surgery of Rhythm Disorders
Interventional arrhythmology has been one of the main directions in the scientific and clinical work of the Department of Clinical Electrophysiology since its founding in 1990. It has almost 20 years of experience in treating various heart rhythm disorders using catheter ablation technology.
Since 2012, the department has introduced a catheter ablation method for AF. Today, the priority method used in the clinical practice of the Department of Clinical Electrophysiology for non-drug treatment of AF is the method of balloon cryoablation. This choice is based on the fact that cryoablation for AF is not inferior in effectiveness to radiofrequency, while being the safest method of interventional treatment of AF, which was proven by analyzing the many years of experience of the world's leading centers in the treatment of AF.
Specialists from the Department of Clinical Electrophysiology conduct a full preoperative examination of patients, perform interventional interventions and provide outpatient monitoring of all patients for at least 1 year after catheter cryoablation of AF. In cases where patients have complex concomitant heart rhythm disorders, complex (one-stage) interventional treatment, or the so-called. “hybrid therapy”, combining catheter intervention and subsequent drug treatment. If AF recurs, repeat balloon cryoablation or radiofrequency catheter ablation may be performed.
Radiofrequency ablation of paroxysmal supraventricular tachycardias
The most common types of paroxysmal supraventricular tachycardias are:
- Paroxysmal atrioventricular nodal reentrant tachycardia or AV nodal tachycardia. It is characterized by the presence of a congenital anomaly - an additional pathway in the AV node, which normally conducts impulses from the atria to the ventricles. This anomaly is the cause of tachycardia (Fig. 9);
Rice. 9. Paroxysm of AV nodal tachycardia on the ECG.
-Paroxysmal tachycardia in Wolff-Parkinson-White syndrome (WPW syndrome) also occurs due to a congenital anomaly - an additional pathway between the atria and ventricles (Kent's point). (Fig. 10);
Fig. 10 Kent bundle of left lateral localization
-Atrial tachycardia can have a source in both the left and right atria (Fig. 11), and can be a consequence of concomitant heart diseases (coronary heart disease, hypertension or valve defects), or have the so-called. idiopathic (without concomitant pathology) nature.
Fig. 11 Sources of atrial tachycardia in the left atrium (indicated by arrows)
An ECG recorded during a paroxysm of tachycardia often does not allow an accurate diagnosis to be made.
It can be clarified by such examination methods as transesophageal pacing (TEPS) or intracardiac electrophysiological study (ECES), which are standard methods for diagnosing arrhythmias.
Surgical treatment of the above types of tachycardias using radiofrequency ablation (RFA) allows you to completely get rid of arrhythmia; the effectiveness of the method is 97-99%. At the same time, the risk of potential complications of RFA, as a rule, does not exceed 1%.
Ventricular tachycardia
With ventricular tachycardia, a pathological impulse circulates in the myocardial tissues of the right or left ventricles.
This type of arrhythmia can occur in healthy individuals without any serious heart pathology. Often these heart rhythm disturbances have a benign course and do not always require treatment.
In other cases, ventricular tachycardia may be the result of serious illnesses such as myocardial infarction, which can cause sudden cardiac death. (Fig.12)
Figure 12 Ventricular tachycardia
Currently, non-drug treatment methods, such as radiofrequency ablation (RFA) or implantation of a cardioverter-defibrillator, are usually used to treat ventricular tachycardia.
To select the optimal treatment method, a comprehensive examination is necessary.
Indications for implantation
When drug treatment is not enough, the cardiologist recommends implantation of a pacemaker. The operation is intended to treat diseases:
- bradycardia, accompanied by constant fainting, loss of consciousness, dizziness, low pulse during physical exertion;
- atrial fibrillation;
- AV heart block with clinical manifestations;
- sick sinus syndrome;
- cardiomyopathy with impaired myocardial contractile function;
- chronic heart failure.
Relative indications include:
- AV heart block without clinical manifestations;
- fainting states are not associated with complete transverse block or ventricular tachycardia, but another cause of the condition cannot be established.
In this case, the decision on implantation is made by the doctor individually for each patient, taking into account physiological characteristics and the presence of concomitant pathologies.
In fact, there are no contraindications to installing an pacemaker. Surgery may be postponed due to viral or infectious diseases. After treatment of the concomitant pathology, the operation is carried out as planned after examinations.
Consequences and complications of the operation
Implantation of an artificial heart pacemaker is a surgical intervention in which there is a risk of complications:
- perforation of the myocardial wall;
- venous bleeding;
- pneumothorax;
- thrombosis of the subclavian vein.
During the recovery period, the following may develop:
- infectious inflammation of the area where the pacemaker is installed;
- endocarditis;
- conductor migration;
- pacing syndrome.
The latter develops in patients with a single-chamber pacemaker installed. The disorder is based on asynchronous contraction of the atria and ventricles, as a result of which the diastolic filling of the cavities of the heart decreases - the patient experiences increased symptoms of heart failure. Pacemaker syndrome requires additional studies (radiography, Holter rhythm monitoring) and reprogramming of the device.
In rare cases, after ICD placement, shocks may be generated when the rhythm is normal or cardioversion may not be performed when needed. The main causes of the problem are: migration of the electrode inside the cardiac cavity, an increase in the threshold of sensitivity to impulses, or complete discharge of the power supply.
Symptoms that require you to consult a doctor:
- fever, redness of the postoperative scar, pain, swelling, discharge of fluid, pus;
- uncharacteristic sensations in the area of the pacemaker;
- dyspnea;
- attacks of dizziness, loss of consciousness;
- decreased tolerance to physical activity;
- constant fatigue, drowsiness;
- chest pain;
- constant hiccups;
- increasing swelling of the legs;
- heartbeat;
- heart rate decreases below the programmed level.
Electrode dislocation
The situation represents a shift in the position of the electrode relative to the area of its installation. Most often it occurs in the first day or several weeks after surgery. The electrocardiographic picture will depend on the position of the torn conductor:
- disordered unresponsive stimuli with imposed complexes;
- failure of synchronization and stimulating function of the device;
- stimulation of the atrium or phrenic nerve.
Symptoms of dislocation of electrodes in a pacemaker manifest themselves in the form of an increase in the symptoms of heart failure and require immediate correction of the position of the conductors or their complete replacement.
Despite positive reviews of pacemakers from patients, an artificial driver or cardioverter-defibrillator is implanted to correct the heart rhythm, and this does not eliminate the root cause of the disorders.
Preparing for surgery
Before the operation, the patient must undergo a full examination and pass a list of tests. Our cardiology center of the Federal Scientific and Clinical Center FMBA offers its patients planned hospitalization. During your stay in the cardiovascular surgery department, you will undergo all the necessary tests. The list of examinations includes:
- clinical and biochemical blood test (total protein, creatinine, urea, total bilirubin, direct bilirubin, glucose, pancreatic amylase);
- determination of blood group and Rh factor;
- detailed coagulogram;
- platelet aggregation indicator ADP;
- markers of infections: HIV, hepatitis B, hepatitis C, syphilis;
- general urine analysis;
- chest x-ray;
- ECG;
- EchoCG;
- EGDS;
- Ultrasound scanning of brachiocephalic arteries;
- Ultrasound scanning of the arteries of the lower extremities and veins of the lower extremities;
- FVD;
- Ultrasound of internal organs;
- TEE;
- coronary angiography.
If during the examination the doctor discovers a concomitant pathology, you may be prescribed additional tests and consultation with related specialists (neurologist, ophthalmologist, endocrinologist, etc.).
Our center is equipped with high-precision modern equipment. Thanks to their extensive experience and many years of work experience, doctors guarantee the most accurate diagnosis and interpretation of indicators. Our own clinical diagnostic center is responsible for the accuracy of test results. By undergoing an examination with us before implantation of an pacemaker, you can be confident in the quality of the services provided and the speed of their provision. Collecting all the necessary research can take months, while we will prepare you for surgery in just 1 day.
Before the operation, the patient needs to prepare; to do this, just follow simple recommendations:
- A few days before surgery, the doctor may stop taking medications. Alcohol must be eliminated (preferably a week in advance);
- on the day before pacemaker implantation, the patient has breakfast and lunch as usual. In the evening, a light dinner is brought, the last meal should be no later than 6-8 hours before the operation. You can drink water in unlimited quantities;
- at night the patient is given a cleansing enema;
- In the morning, the patient takes a shower and prepares the surgical field. It is necessary to shave the hair in the chest area.
Before the patient is taken to the operating room, he is examined by a surgeon and an anesthesiologist. A mild sedative may be administered to calm and relieve anxiety.
Heart functions
Before talking about the classification of pacemakers or pacemakers, it should be said about the main functions of the heart:
- The heart has automatism , which means the ability of the pacemaker system to independently produce excitation impulses in a self-oscillatory mode. The higher-lying sections of the conduction system have a depressing effect on the underlying ones, since the pacemaker of the first order has greater automaticity than the pacemaker of the heart of the second, third or fourth order.
- The heart has excitability , which means the ability of cardiomyocytes to be excited under the influence of stimuli of various origins, chemical or physical.
- The heart has conductivity , which means the ability of cardiac structures to conduct excitation from one participant of the pacemaker system to another due to a change in the action potential.
- The heart has contractility , which means the ability of the heart muscle to contract under the influence of electrical impulses, and the greater the length of the muscle fiber, the greater the contraction.
- The heart is refractory , which means the ability of cardiomyocytes to be temporarily unresponsive to any impulses after contraction. The function ensures the restoration of the action potential in the cells and the relaxation of the heart muscle.
Implantation of a pacemaker
The operation to implant a pacemaker is performed under local anesthesia. Depending on the type of pacemaker, the procedure can take from half an hour when installing a single-chamber pacemaker, to 2.5 when installing a three-chamber pacemaker. If the patient is right-handed, the pacemaker is installed in the left subclavian region, if left-handed - in the right. This allows you to reduce the impact of the pacemaker on the working arm.
The cardiac surgeon and assisting staff perform the following actions:
- the surgical field is treated with antiseptics and anesthetized;
- the surgeon makes a small incision about 5 cm under the collarbone and creates a pocket for implantation of the pacemaker. The pocket may be located under or above the pectoralis major muscle. The location is determined by the surgeon;
- From the incision, the subclavian vein is punctured (pierced) with a special needle;
- A conductor is inserted into the vein through a needle into the cavity of the heart. The doctor controls the movement of the conductor using an X-ray unit;
- the needle is removed and an introducer (plastic tube) is inserted into the vein along the guidewire. Depending on the type of pacemaker, if it is necessary to introduce 2 or three electrodes, an additional introducer is inserted along the same path or through a puncture of another vein;
- the conductor is removed;
- 1 or several electrodes are inserted into the heart cavity through the introducer. The electrodes are attached to the inner lining of the heart using hooks at the end of the electrode or using a special fastener that resembles a corkscrew (the electrode seems to be screwed into the inner lining);
- when the electrodes are installed in the desired location, the introducer is removed;
- the doctor connects the other end of the electrodes to the pacemaker;
- the pacemaker is implanted into a previously formed pocket under the collarbone;
- the wound is sutured;
- an aseptic dressing is applied;
What is a pacemaker and how does it work?
A pacemaker (pacemaker) is a medical device designed to encourage or impose a normal rhythm on patients whose heartbeat is not fast enough or there is a blockage in signal transmission between different parts of the organ.
It is a small-sized device measuring 3 by 5 centimeters, weighing 30-45 grams, the service life without replacing batteries varies from 5 to 15 years. The operating principle of the device is based on the application of external electrical stimuli produced by the pacemaker to the heart area to ensure normal myocardial contraction. Advanced (frequency-adaptive) pacemakers additionally have sensors that can respond to changes in respiratory rate, nervous system activity, and body temperature. There are also pacemakers equipped with a defibrillator. Modern models have the function of non-invasively changing operating parameters using special devices.
A chip embedded in the device analyzes the signals generated by the heart, transmitting them directly to the myocardium and ensuring their synchronization. Conductors implanted under the endocardium transmit information from the external part of the device to the heart and data about the work of the myocardium itself back. The end of each electrode is equipped with a metal tip that collects indicators of cardiac activity and generates impulses only when necessary. When a critical decrease in heart rate or asystole develops, the pacemaker begins to work in a constant mode, producing stimuli at the frequency specified when it was implanted. If there is a sudden resumption of cardiac automaticity, the device goes into a standby state.
In emergency cases, temporary cardiac pacing is used. With external (transthoracic) pacemaker, electrodes are placed on the chest. Since the procedure is very painful, it requires deep sedation and anesthesia. Transesophageal manipulation involves the installation of a temporary device in the esophagus, and therefore has limited use.
After operation
The patient is under the supervision of medical personnel for a week. During this time, the sutures heal and can be removed. The patient is preparing for discharge. Before sending the patient home, he is examined by a doctor. Makes appointments and issues instructions on how to behave during the rehabilitation period and move on with your life.
After discharge, the patient registers at his place of residence and promptly visits the doctor. In the first 3 months, it is important to follow the recommendations:
- temporarily stop physical activity;
- you cannot lift weights;
- You can’t drive;
- MRI cannot be done;
- avoid radar technology;
- refuse thermal procedures;
- Report any ailments to your doctor.
You should visit a cardiologist regularly for the next six months. It is allowed to use household appliances. You need to turn them on with the opposite hand to the installed pacemaker, including when talking on the phone, and place the phone on the opposite side of the installed pacemaker. Metal detectors should be avoided in stores, airports, and concert halls.
Lifetime rules after pacemaker implantation:
- monthly visit to a cardiologist;
- daily measurement of blood pressure and pulse. It is advisable to keep a diary and mark the data;
- complete cessation of bad habits;
- carry your pacemaker passport with you.
Installation of a pacemaker: how is the operation performed?
Before the intervention, the patient must undergo a number of instrumental studies:
- ECG with description;
- 24-hour Holter monitoring;
- EchoCG;
- general radiography of the OGK;
- bicycle ergometry, treadmill test;
- transesophageal examination of the cardiac conduction system.
Implantation of an pacemaker or cardiac defibrillator is considered a minimally invasive and low-traumatic procedure that does not require deep anesthesia and is performed under local anesthesia. If necessary, the patient may be given additional sedatives, but the patient remains conscious at all times and can talk to the medical staff. The procedure is carried out in a special operating room with an X-ray machine to constantly monitor the position of the electrodes. Duration – from 30 minutes to 1.5 hours.
Under X-ray control, a puncture of the subclavian vein is performed on the side opposite the leading arm (on the left for right-handed people and vice versa). Through a central catheter fixed to the skin, thin electrical probes are inserted into the heart cavity, which will conduct impulses from the subcutaneous part of the device to the heart. After attaching the electrodes, the cardiologist performs a series of tests to determine the threshold of myocardial sensitivity to signals in response to which an effective contraction should follow.
Throughout the procedure, the electrocardiogram is continuously recorded and interpreted.
During the operation, the doctor asks the patient to perform some tests to ensure that the electrodes are securely attached to the endocardial layer of the heart wall - take a deep breath, cough, slightly tense the abdominal muscles. After calibrating the optimal ECG indicators, the conductor is finally fixed and connected to the outdoor unit.
The pacemaker body is implanted in a pocket formed of fatty tissue or under the pectoral muscle in thin patients. After connecting all the wires, the “bed” is sutured tightly with self-absorbing sutures.
To prevent complications, a sterile bandage is applied to the vein puncture site and a prophylactic course of broad-spectrum antibiotics is prescribed.
Strict bed rest is required for the first 24 hours (there is a risk of displacement of the conductors inside the heart). The patient is under 24-hour supervision by a doctor on duty. On the second day, an X-ray inspection of the installed device is performed, the pacemaker system is adjusted (the operation of the device is optimized depending on the patient’s own rhythm), and daily electrocardiographic monitoring is carried out.
Immediately after the operation, sudden movements should be avoided: swinging the arm on the implantation side, quickly getting out of bed, bending the body, coughing. Also, do not sleep on your stomach, putting pressure on the place where the stimulator was installed.
Features of implantation in the elderly
A pacemaker can be installed in a patient of any age. The only nuance typical for older people is an increased risk of rejection due to an immune reaction to a foreign object. Due to combined pathology (the presence of atherosclerosis, type 2 diabetes mellitus), the level of complexity of installing the device increases, the procedure for implantation and healing of the postoperative scar is lengthened. The likelihood of developing purulent complications does not depend on the patient’s age. The doctor takes into account all the pros and cons of installing a pacemaker of each type for a particular patient and chooses the safest option.
Stimulator operating life
The exact length of time your pacemaker battery lasts depends on the type of pacemaker, your health, lifestyle, and other factors. Typically, the duration of work is from 5 to 10 years. You can get more information about the type of pacemaker you have from your doctor. How is a pacemaker replaced?
It is generally a safe and simple procedure to replace your old pacemaker with a new one. During the process of replacing a pacemaker, the doctor monitors the electrodes. If they function flawlessly, the doctor only connects them to a new pacemaker.
Period after implantation
Typically, the recovery period after surgery is quite short. You may have some pain around the pacemaker implantation site, in which case your doctor will prescribe a pain reliever. You may need some time to get used to your pacemaker. However, the feeling of discomfort will pass very soon. You should have your first examination with your doctor soon after surgery. He will check the electrical activity of your heart and the functioning of your pacemaker. If necessary, the doctor will adjust the parameters of the program according to which the pacemaker operates to suit your individual needs. On average, you should have regular checkups every six months. In general, you will be able to live a full life soon after implantation. You can continue to do your normal activities - work in the garden or around the house, drive a car. You can shower, bathe or swim. After consulting with your doctor, you can resume sports, favorite activities, and resume sexual activity.