One of the most common diseases in pediatrics is anemia.
In children under 3 years of age, anemia occurs in 40% of cases, during puberty in 30%.
Anemia is a pathological condition characterized by a decrease in hemoglobin content and, in almost all cases, the number of red blood cells in the blood.
Very often, the occurrence of anemia is associated with the intensive growth of the child’s body, the increased process of formation, development and maturation of blood cells in children.
The process of hematopoiesis in a newborn child differs significantly from the process of hematopoiesis in an adult. Only at the 4th - 5th month of life does the bone marrow period of hematopoiesis begin, which becomes decisive for the rest of life. During this period and until the 6th month, there is a physiological decrease in the amount of hemoglobin and red blood cells in the child’s blood. For the normal development of the hematopoietic system, a large amount of iron, vitamins, microelements and protein is required. That is why great importance is given to the child’s nutrition, as well as morbidity during this period. The toxic effects of seemingly the simplest and most easily treatable diseases very often cause the development of anemia in a child.
The most vulnerable are children between the 6th and 12th months of life, which is associated with the depletion of iron reserves accumulated during fetal development.
Long-term anemia in children is accompanied by hypoxia, and profound changes in organs and tissues can develop. Such children lag behind their peers in physical and mental development, they more often suffer from respiratory diseases with the risk of intercurrent diseases (accidentally acquired disease complicating the course of the underlying disease), they are more prone to the development of chronic diseases and various complications.
What is iron deficiency anemia in a child?
Pediatricians around the world deal with this disease every day.
This group of diseases includes those associated with a decrease in the content of hemoglobin and/or red blood cells per unit volume of blood, which negatively affects the oxygen supply to the body’s tissues. Iron deficiency anemia is the most common of all anemias, accounting for 80% of all cases. In our country and Europe, the prevalence of iron deficiency anemia in young children is approximately 50%, and in older children - 20% or more.
Iron deficiency anemia in a child is a syndrome characterized by a lack of iron in the body. It develops against the background of pathological processes and is manifested by signs of anemia and sideropenia.
Iron is one of the main microelements in the body of both children and adults. The body has hemoproteins, which contain about 70% of the total amount of iron, which is associated with porphyrin. Iron is contained in hemoglobin, myoglobin, peroxidases, cytochromes, catalases, etc.
This element is stored in the body in the form of ferritin (the majority) and hemosiderin. In babies, most of the iron is stored in erythroid cells and very little in the muscles.
Causes
According to the time of occurrence of anemia there are:
- Intrauterine.
During intrauterine development, the fetus creates an iron reserve, on average 300 mg. Peak iron accumulation occurs in the third trimester. If the period from 28 to 32 weeks is unfavorable (threat of miscarriage, placental abruption, fetoplacental insufficiency), the fetus does not have time to stock up on iron. The likelihood of anemia is high in premature babies and children born from multiple pregnancies. - Intranatal and early neonatal.
During childbirth, prerequisites for the development of anemia can also be created - early placental abruption, rupture of umbilical cord vessels, and fetal injuries. After birth, the main danger is fetal hemolytic disease (destruction of fetal red blood cells by maternal antibodies) and genetically determined bone marrow diseases. - Purchased.
Anemia is subsequently caused by poor nutrition. This happens if there is little iron in breast milk, inappropriate formulas or cow's milk are used. Premature babies and those children whose body weight is higher than normal require more iron than usual. Anemia occurs when there is insufficient supply of B vitamins, macro- and microelements, and when the baby lives in poor sanitary and hygienic conditions.
At risk are children with blood diseases, frequent nosebleeds, food allergies and atomic dermatitis (a childhood form of eczema), impaired absorption in the intestines. In children, anemia develops with any more or less severe infection (pyelonephritis, bronchiectasis), helminthic infestation, connective tissue diseases (rheumatoid arthritis).
Pathogenesis (what happens?) During iron deficiency anemia in a child:
Iron leaves the body through urine, feces, sweat, as well as through nails, hair and skin. Losses do not depend on gender. In children, about 0.1–0.3 mg is released into the external environment per 24 hours. In adolescents, the loss is a maximum of 0.5–1.0 mg. The child needs to receive 0.5–1.2 mg of iron per day. There is an increased need for infants and preschoolers. In order for a child to develop normally, the diet should contain 1.5 mg of iron per day in newborns, and at least 10 mg in children from 1 to 3 years old.
Iron deficiency provokes a tendency to infectious diseases of the baby's gastrointestinal tract and respiratory system. Without iron, brain structures cease to function normally. With a lack of iron, disruptions occur in the neuropsychic development of the baby. In children who were diagnosed with iron deficiency anemia in infancy, at the age of 3-4 years, disturbances in the transmission of nerve impulses from the centers of the brain to the organs of hearing and vision are found due to impaired myelination and, as a consequence, impaired nerve conduction.
Diagnosis of anemia
The diagnosis is established after a laboratory blood test, namely the number of red blood cells and hemoglobin.
They speak of anemia if the amount of hemoglobin is less than 110 g/l, red blood cells are less than 3.5 x 10¹²/l. These indicators correspond to a mild degree of anemia. Moderate anemia is established with the following indicators: hemoglobin less than 90 g/l, red blood cells up to 2.5x10¹²/l, severe anemia with hemoglobin less than 70 g/l, red blood cells less than 2.5x10¹²/l. When anemia is detected, the child is consulted by specialized specialists: gastroenterologist, nephrologist, allergist and others as appropriate.
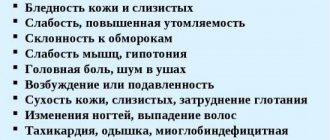
Less known clinical manifestations of iron deficiency include:
- neurotic reactions and neurasthenia;
- decreased muscle performance and general exercise tolerance;
- disturbances of metabolic processes in the myocardium;
- disorders of peripheral circulation and microcirculation.
The diagnosis of IDA is based on the characteristic clinical picture, changes in the blood and absolute iron deficiency.
Iron metabolism in a child's body
The fetus receives iron from the mother through the placenta throughout pregnancy, most intensively from the 28-32nd week. The body of a full-term baby contains about 300-400 mg of iron, while a premature baby contains only 100-200 mg. After birth, iron reserves received from the mother are replenished due to the utilization of hemoglobin during the breakdown of “extra” red blood cells containing HbF. Neonatal (maternal and erythrocyte) iron is spent on the synthesis of hemoglobin, myoglobin, iron-containing enzymes necessary to maintain normal metabolism and homeostasis, as well as to compensate for natural losses (with feces, urine, sweat), for the regeneration of skin cells, mucous membranes, etc. .d. In addition, the child needs to create iron reserves, i.e. The iron balance must be positive.
The needs of a full-term baby up to 3-4 months are satisfied by endogenous iron and mother’s milk, which contains iron in an average amount of 0.5 mg/l, and up to 50% of it (0.25 mg) is absorbed in the intestine with the help of a special protein, lactoferrin. However, by 5-6 months in a full-term baby and by 3-4 months in a premature baby, the need for iron, amounting to 1 mg/day, is satisfied by only 1/4 from these sources. Artificial feeding with cow's milk, consumption of cheese, eggs, tea, oxalates, and phosphates slows down the absorption of iron. Ascorbic, succinic and other organic acids, fructose, sorbitol, and animal protein promote the absorption of iron.
Iron absorbed in the small intestine is transported to the red bone marrow and tissue depots using the transport protein transferrin. There are heme (80% of the iron in the body) and non-heme iron.
Distribution and functions of iron in the body
| Connections | Function | Processes | |
| Heme iron | Hemoglobin, myoglobin, cytochromes (30 types), catalase, etc. | Transport 02, electrons, destruction of peroxide compounds | Porphyrin metabolism, collagen synthesis, normal functioning of lymphocytes and granulocytes, body and nerve growth |
| Non-heme iron | Flavoproteins, succinate dehydrogenase, xanthine oxidase, etc. | Redox processes in cells, oxidative phosphorylation |
In addition to what is indicated in the table, non-heme iron also includes transferrin (the main transport protein), ferritin and hemosiderin (proteins that serve as a reserve source of iron in the body). Iron is involved in many metabolic processes. Without it, normal growth and development of a child is impossible.
Iron deficiency in the body (sideropenia) goes through three stages.
- Prelatent - insufficient iron content in tissues, hemoglobin and serum iron concentrations are not changed.
- Latent - the hemoglobin concentration is normal, but serum iron is reduced.
- Iron deficiency anemia - all red blood parameters are changed.
Clinical picture of iron deficiency conditions
The clinical picture of iron deficiency states (sideropenia) is nonspecific and includes several syndromes.
- Asthenovegetative syndrome is a consequence of impaired brain function. Young children with iron deficiency anemia are delayed in psychomotor development. They are whiny, irritable, capricious, and have poor contact with peers. In older children, intellectual development suffers: memory, attention, and interest in learning are reduced. Signs of autonomic dystonia syndrome appear. Possible muscle pain and hypotension (in particular of the bladder), enuresis.
- Epithelial syndrome includes dystrophy and atrophy of barrier tissues (mucous membranes, skin and its derivatives - nails, hair). Inflammatory changes are easily associated with trophic disorders. As a result, appetite decreases, perversion of taste and smell (pica chlorotica), dysphagia, dyspeptic disorders, disturbances in intestinal absorption processes, and hidden intestinal bleeding occur. Pale skin and conjunctiva are detected only with a significant decrease in hemoglobin concentration.
- Immunodeficiency syndrome is manifested by frequent ARVI and acute intestinal infections. About 70% of frequently ill children suffer from sideropenia. They have reduced both nonspecific (lysozyme, properdin, etc.) and specific immunity. It has been shown that in the absence of iron, IgA loses its bactericidal activity.
- Cardiovascular syndrome is observed in severe iron deficiency anemia. Children develop increased fatigue, low blood pressure, tachycardia, decreased cardiac muscle tone, muffled tones, a functional, rather rough systolic murmur, well audible on the vessels (“spinning top murmur”) and associated with hydremia. Dizziness is possible.
- Hepatolienal syndrome occurs rarely, usually with severe anemia and a combination of rickets and anemia.
Recently, attention has been paid to the fact that iron deficiency increases the absorption of lead in the gastrointestinal tract. This is especially important for children living in big cities, near highways. In this case, the manifestations of sideropenia may be accompanied (especially in young children) by lead intoxication, leading to severe mental and neurological disorders, impaired renal function and hematopoiesis. Anemia then becomes refractory to treatment with iron supplements.
Laboratory criteria for iron deficiency in children
| Index | Norm | Latent deficiency | Iron-deficiency anemia |
Hemoglobin, g/l
| >110 >120 | >110 >120 | |
| Color index, % | 0,86-1,05 | 0,86-1,05 | |
| Serum iron (SI), µmol/l | 10,6-33,6 | ||
| Average hemoglobin content in an erythrocyte, pg | 24-33 | 24-33 | |
| Average hemoglobin concentration in erythrocyte, % | 30-38 | 30-38 | |
| Total iron binding capacity serum (WSS), µmol/l | 40,6-62,5 | >63 | |
| Latent iron binding capacity of serum, µmol/l | >47 | >47 | >47 |
| Transferrin saturation coefficient iron (ZhS/OZhSS), % | >17 | ||
| Serum ferritin, µg/l | >12 | ||
| Desferal siderouria*, mg/day | 0,65+0,006 |
* The content of desferrioxamine (desferal) administered intramuscularly at a rate of 10 mg/kg is determined in daily urine.
Diagnosis of iron deficiency conditions
The diagnosis of iron deficiency anemia and latent iron deficiency is based on the laboratory criteria outlined above. The main indicator is the ferritin content in the blood serum. If it is impossible to obtain all the specified data, you can rely on the following indicators, available in any medical institution.
- Hemoglobin concentration.
- The color index is calculated as follows: color index = [(hemoglobin concentration, g/l)×3]÷(the first three digits of the number of red blood cells without a comma). Normally it is 0.85-1.05.
- Morphology of red blood cells in a peripheral blood smear.
- The Loitzky coefficient is calculated as follows: Loitzky coefficient = (hematocrit, %)÷(hemoglobin, %). Normally - less than 3.1.
- The result of treatment with iron preparations when taken orally: after 10-14 days, the hemoglobin concentration increases daily by 1-4 g/l, the content of reticulocytes increases to 3-4% (reticulocyte crisis).
Clinical forms of predominantly iron deficiency anemia
Early anemia of prematurity
Early anemia of prematurity has a complex pathogenesis and develops in the 1st-2nd month of life in more than half of premature infants and occasionally in full-term infants (“physiological” benign anemia), especially with an unfavorable premorbid background. During an objective examination, only pallor is noted (with a decrease in hemoglobin concentration to 80 g/l). When examining peripheral blood, normo- or hyperchromic normoregenerative anemia is detected, often reaching a severe degree.
The main reasons for the development of early anemia are considered to be increased “physiological” hemolysis of red blood cells containing HbF, insufficient functional and morphological maturity of the red bone marrow, and a decrease in the production of tissue erythropostins due to hyperoxia that occurred at the birth of the child. Of great importance is also the deficiency of many substances necessary for hematopoiesis, deposited in the depot only in the last 2 months of pregnancy (protein, vitamins C, E, group B, copper, cobalt) and ensuring the absorption, transport, exchange and fixation of iron in the heme molecule, and also the stability of the membranes and membranes of red blood cells. There is also a deficiency of iron in the depot, temporarily compensated by ongoing hemolysis, but clearly detected by detecting microcytosis and hypochromia of some red blood cells, a decrease in the concentration of serum iron and the number of siderocytes in the red bone marrow punctate. Once neonatal iron stores are depleted, early anemia progresses to late anemia of prematurity.
Treatment of early anemia is difficult. Previously, red blood cells were transfused for health reasons; now epoetin beta (for example, recombinant human erythropoietin) is successfully used.
Prescribe 10 injections of erythropoietin at a dose of 200 units/kg subcutaneously 3 times a week. At the same time, iron supplements (2 mg of elemental iron per day), folic acid (0.001 g/day) and vitamin E (25 mg/day for 2-3 months) are prescribed.
Late anemia of prematurity
Late anemia of prematurity (constitutional) develops at the 3-4th month of life as a result of depletion of neonatal iron stores in the depot. Clinical manifestations are usually minor; laboratory data indicate predominant iron deficiency.
Nutritional and infectious anemia
Nutritional and infectious anemia develop in the second half of life in full-term infants. In the origin of nutritional anemia, feeding disorders play a role, simultaneously causing dystrophy. Infectious diseases, most often acute respiratory viral infections and otitis media, usually contribute to a more severe course of nutritional anemia. Clinical and laboratory manifestations are characteristic of the predominance of iron deficiency.
Chlorosis
Chlorosis is a rare disease in girls during puberty. Develops against the background of regime disruption and endocrine dysfunction. Manifested by weakness, increased fatigue, anorexia, perversion of taste, dizziness, sometimes fainting, palpitations, pain in the epigastric region, nausea, vomiting, constipation. Characteristics: “alabaster”, in some cases with a greenish tint, pale skin, menstrual irregularities (oligo- or amenorrhea). Recovery is usually spontaneous, but relapses are possible. Laboratory studies indicate a predominant iron deficiency.
Differential diagnosis of deficiency anemias
Differential diagnosis of iron deficiency anemia is carried out with other deficiency anemias, thalassemia and sideroblastic anemia - lead and pyridoxine-dependent, in which erythropoiesis is impaired as a result of impaired incorporation of iron into heme. Hypochromia of erythrocytes in the latter case is combined with an increase in serum iron concentration.
- Clinical manifestations of acquired sideroblastic anemia caused by lead intoxication are more manifest than with iron deficiency anemia: cramping abdominal pain, severe dyspeptic symptoms, pallor with an earthy tint, mental and neurological disorders. Blood tests revealed basophilic granularity, hypochromia of erythrocytes, increased serum iron concentration. Urine tests measure aminolevulinic acid.
- In hereditary pyridoxine-dependent sideroblastic anemia, heme synthesis is disrupted at the last stage. Free protoporphyrin accumulates in hypochromic erythrocytes, serum iron concentration is increased, and there are many sideroblasts in the red bone marrow.
- Protein deficiency anemia is accompanied by more pronounced pallor and dyschromia of the skin and hair, blepharitis, tissue pastiness or edema, anorexia, vomiting, and diarrhea. The hemoglobin concentration is reduced to 40-90 g/l, the color index is within normal values, aniso- and poikilocytosis are pronounced.
- Vitamin deficiency anemia (deficiency of vitamins B12, C) is manifested by asthenia, paresthesia, pallor with a lemon-yellow tint, subicteric sclera, glossitis, aphthous stomatitis, and moderate hepatomegaly. The hemoglobin concentration is reduced, as is the content of erythrocytes, normo- and hyperchromic, the color index is increased (more than 1.0). Macro-, poikilo- and anisocytosis, Jolly bodies, Cabot rings, megaloblasts, and giant metamyelocytes appear. In red bone marrow punctate, a megaloblastic type of hematopoiesis is detected.
Treatment of iron deficiency anemia is carried out in three stages.
Stages of treatment for iron deficiency anemia
| Stages | Target | Duration _ | Average daily doses of elemental iron |
| Elimination of anemia | Restoring normal hemoglobin concentration | 1.5-2 months | Up to 3 years - 3-5 mg/kg/day; from 3 to 7 years - 100-120 mg/day; over 7 years - up to 200 mg/day |
| Saturation therapy | Restoring iron reserves in the body | 3-6 months | Up to 3 years - 1-2 mg/kg/day; from 3 to 7 years - 50-60 mg/day; over 7 years - 50-100 mg/day |
| Maintenance therapy | Maintaining normal levels of all iron funds | For bleeding from the gastrointestinal tract 7-10 days every month, and for teenage girls with hyperpolymenorrhea - 7-10 days after each menstruation | 40-60 mg/day |
A mandatory and most important component of each stage is taking iron supplements. In the vast majority of cases, iron supplements are taken orally. When treating iron deficiency anemia and latent iron deficiency, in addition to iron supplements, it is necessary to adhere to the regimen, follow a diet balanced in terms of the main ingredients; normalization of iron absorption if it is impaired (for example, combined treatment with enzyme preparations for malabsorption syndrome), dosed physical activity.
Treatment with oral iron supplements
The most commonly used iron compounds include iron (III) hydroxide polymaltosate (maltofer) and ferrous salts - sulfate, fumarate, chloride and gluconate. To improve absorption, ferrous salts are combined with organic acids, amino acids and other compounds. Liquid dosage forms are indicated for young children, allowing for more precise dosing of iron.
Iron supplements used in young children
| A drug | Compound | Dosage form | Elemental iron content |
| Maltofer | Iron hydroxide polymaltose complex | Drops | 1 ml (20 drops) – 50 mg |
| Aktiferrin | Ferrous sulfate, series | Drops Syrup | 1 ml (18 drops) - 9.5 mg; 1 drop - 0.54 mg 1 ml - 6.8 mg, 1 teaspoon - 34 mg |
| Hemofer | Ferric chloride | Drops | 1 ml (20 drops) 44 mg; 1 drop - 2.2 mg |
- Older children and adolescents are prescribed tablets and capsules containing iron. Recently, combination preparations containing vitamins and other microelements in addition to iron have been used mainly for preventive purposes. The drug of choice is maltofer, which contains iron in nonionic form, does not cause side effects, has a pleasant taste, and is taken immediately after or during meals. It can be added to any juices and dishes. The remaining medications are taken between meals, washed down with fruit juices (preferably citrus). At the same time, take an age-specific dose of ascorbic acid.
The most commonly used iron supplements
| A drug | Compound | Dosage form | content , mg |
| Maltofer-Fol | Iron hydroxide polymaltose complex + folic acid | Tablets (chewable) | 100 |
| Aktiferrin | Ferrous sulfate, series | Capsules | 34,2 |
| Aktiferrin-compositum | The same + folic acid + cyanocobalamin | Capsules | 35 |
| Hemophere prolongatum | Ferrous sulfate | Capsules | 105 |
| Conferon | Ferrous sulfate + sodium dioctyl sulfosuccinate | Capsules | 50 |
| Ferroplex | Iron sulfate + ascorbic acid | Dragee | 50 |
| Sorbifer | Iron sulfate + ascorbic acid | Pills | 100 |
| Ferrograd S | Iron sulfate + ascorbic acid | Pills | 100 |
| Tardiferon | Ferrous sulfate + mucoprotease | Pills | 80 |
| Ferrogradumet | Ferrous sulfate | Pills | 65 |
| Heferol | Iron fumarate | Capsules | 115 |
| Pregnavite | Iron fumarate + multivitamins | Pills | 30 |
| Materna | Iron sulfate + multivitamins | Pills | 60 |
| Fenyuls | Iron sulfate + multivitamins | Capsules | 45 |
The daily dose of all drugs is divided into three doses. At the beginning of treatment, the drugs are prescribed at half the dose for several days to clarify their individual tolerability. In the absence of dyspeptic symptoms and other side effects, proceed to the age-specific dose. Combination drugs prescribed for prophylactic purposes are taken once a day.
Iron preparations for parenteral administration
Parenteral iron preparations are administered only if there are appropriate indications.
- Conditions after operations on the gastrointestinal tract.
- Syndrome of impaired absorption in the small intestine.
- Chronic enterocolitis and nonspecific ulcerative colitis.
- Iron intolerance when taken orally.
The main drug for parenteral administration is iron (III) hydroxide polyisomaltose (ferrum lek).
Average daily doses of iron preparations for parenteral administration (calculation based on elemental iron)
| Children's age | Daily dose of elemental iron, mg/day |
| 1-12 months 1-3 years Over 3 years old | up to 25 25-40 40-50 |
Calculation of the course dose of elemental iron for parenteral administration is carried out according to the formula:
Amount of elemental iron = M × (78 - 0.35 × Hb),
where: M is the patient’s body weight, kg; Hb—hemoglobin concentration, g/l.
The course dose of the drug for parenteral administration is calculated using the formula:
Amount of drug per course = KJ/SVP,
where: KI – course dose of iron, mg; SIP - iron content in mg in 1 ml of the drug.
With parenteral administration of iron supplements, side effects often occur: dyspeptic disorders, allergic reactions (up to the development of anaphylactic shock), hemosiderosis. Blood and red blood cell transfusions are carried out only when the hemoglobin concentration decreases to less than 60 g/l.
Prevention
Antenatal prevention. Throughout pregnancy, a woman should take long-acting or complex iron supplements with multivitamins (tardiferon, ferrogradumet, materna, etc.). These medications must be continued while the baby is breastfeeding. In addition, the prevention and treatment of miscarriage and gestosis, good nutrition, and dosed physical activity are important.
Postnatal prevention:
- natural feeding with timely introduction of juices and meat products;
- prevention of other early age diseases;
- adequate regime, good care, sufficient exposure to fresh air;
- monthly peripheral blood test;
- Conducting preventive courses in risk groups with the prescription of iron supplements in half the dose (1-2 mg/kg/day).
Forecast
The prognosis for iron deficiency anemia with timely and consistent treatment is favorable.
Original article www.eurolab.ua Illustrations from the site: © 2011 Thinkstock.
Source: Children's diseases. Baranov A.A. // 2002.
Note to mom
Iron deficiency anemia can be suspected based on the following signs:
- the child has pale skin, lips, and the inside of the eyelids;
- the baby has become more capricious, cries more, sleeps poorly;
- the child has no appetite or it is reduced;
- the child constantly puts inedible things into his mouth: clay, earth, chalk, and they seem tasty to him;
- the baby gets tired quickly, it is difficult for him to do physical activity that he could handle before;
- in children older than one year, the skin becomes dry and rough, the hair becomes dry and brittle, painful cracks may appear in the corners of the mouth, and stomatitis often occurs;
- the child is lagging behind in physical and psychomotor development.
Treatment of anemia
Methods for correcting anemia depend on age.
When breastfeeding, it is necessary to introduce vegetable, fruit and meat complementary foods on time, and spend a lot of time in the fresh air, including in the sun. The room must be well ventilated, kept clean, and sanitary rules for child care must be observed. For older children, it is enough to streamline their diet and daily routine to improve their blood tests. The diet includes beef liver, legumes, seafood, fresh vegetables and fruits, and herbs. If necessary, the timing of vaccination is postponed, massage and ultraviolet irradiation are used.
Medicines are prescribed by a doctor. Iron supplements and vitamins are indicated. The minimum duration of drug treatment is 1 month.
Prevention of anemia
Prevention begins with good nutrition for the pregnant woman, allocating sufficient time for walking and sleeping. Children of the first year of life need to add complementary foods to breast milk after 6 months of age; for older children, a varied, balanced diet should be organized. It is important that during the warm season the baby spends as much time outdoors as possible and takes sunbathing. The team of doctors at the SM-Doctor clinic will help your baby cope with anemia and develop individual preventive measures. Contact professionals to create ideal conditions for the growth and development of your child!