Causes of varicose veins
- Weakness of the venous wall - congenital or acquired.
- Venous valve insufficiency – acquired or congenital.
- Obesity.
- Prolonged stay in a sitting or standing position due to the nature of the profession.
- Repeated pregnancies, intoxication, excessive physical activity, injuries.
- Taking contraceptive hormonal drugs.
If varicose veins appear, you should consult a specialist.
Varicose veins can only be diagnosed by consulting a surgeon or phlebologist. Examination and duplex scanning of the veins are usually sufficient to make a diagnosis.
- The expansion of the veins leads to deformation of the labia.
- In areas affected by varicose veins, dry skin and discoloration are observed.
- Vascular nodules and asterisks appear.
- You may experience discomfort, itching, a feeling of heaviness and, sometimes, pain.
- The skin is irritated, dilated, protruding veins are visible.
- You may experience discomfort during sexual intercourse.
There are the following forms of varicose veins in pregnant women:
- Varicose veins of the lower extremities
- Varicose veins of the pelvis
- Varicose veins of the external genitalia
- Pelvic venous congestion syndrome
- Right ovarian vein syndrome
- Varicose veins of the ovarian veins (varicoovarium)
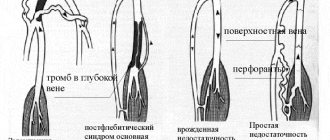
Currently, there are 2 variants of the course of varicose veins of the small pelvis: varicose veins of the perineum and vulva, as well as pelvic venous congestion syndrome. It should be emphasized that this division is quite arbitrary, since in more than 50% of cases, varicose veins of the perineum and vulva provoke a violation of the outflow from the pelvis, and vice versa.
Varicose veins of the perineum and vulva
Occurs in 30% of women during pregnancy. The mechanisms of this condition are basically similar to those of varicose veins of the lower extremities. At the same time, the progressive varicose transformation of the perineal veins is aggravated by compression of the main veins of the retroperitoneal space (iliac and inferior vena cava) by the pregnant uterus. Outside of pregnancy, it persists in 2-10% of cases.
Pelvic Congestion Syndrome
The variety of clinical manifestations and imperfect diagnostics disguise it as various forms of gynecological (inflammatory diseases of the uterus and its appendages, endometriosis), urological (cystitis), surgical (colitis, Crohn's disease, etc.) and even orthopedic (diseases of the hip joint) pathology.
This disease is associated with varicose veins of the venous plexuses of the ovaries and the broad ligament of the uterus. The main mechanism is valvular insufficiency of the ovarian veins, leading to the discharge of blood and increased pressure in the venous plexuses of the pelvis. Predisposing factors may be uterine retroflexion, leading to bending of the broad ligament of the uterus, which impedes the outflow of venous blood, as well as various gynecological diseases (endometriosis, tumors of the uterus and ovaries). In recent years, the adverse effects of hormonal therapy and contraception have been discussed. The influence of hormonal levels is evidenced by the fact that the manifestations of pelvic venous congestion syndrome in the postmenopausal period become less pronounced.
The clinical picture of the disease is quite characteristic and manifests itself as varicose veins of the perineum, vulva, vagina, and lower extremities progressing as the pregnancy period increases (cosmetic defect). Signs of such violations will be:
- Itching in the area of dilated veins.
- A feeling of heaviness and bursting pain in the perineum, pelvis, swelling of the external genitalia, lower extremities.
- Dyspareunia (pain during sexual intercourse)
- Dysmenorrhea
- Severe premenstrual syndrome
- Pain when walking and exercising
- Pain along the veins
- General pain and aches in the legs
- Dysuric disorders.
- Fatigue.
- The development of acute varicothrombophlebitis and rupture of altered veins, which is accompanied by massive bleeding.
Thrombosis during pregnancy is the most important clinical problem. This is due to the high frequency of this condition as a cause of maternal mortality (20% of all causes). As is known, during pregnancy there is a tenfold increase in the risk of thrombosis. The incidence of thrombosis is 0.7 - 4.2/1000 in pregnant women versus 1/10,000 in non-pregnant women of childbearing age.
The critical stage of the thrombotic process is pulmonary embolism - a severe and very often fatal complication of thrombosis. PE is the leading cause of maternal mortality in Western obstetric practice - 0.7 cases per 1000 births (from 11% to 27%). The likelihood of venous thromboembolic complications (VTE) during cesarean section is 3-6 times higher. The risk of developing VTE returns to the level typical for non-pregnant women 6 weeks after birth.
The main WTO risk factors include the following:
- Age (> 35 years)
- C-section
- Weight > 80 kg
- Personal and family history of thrombosis
- Repeated births
- Ovarian hyperstimulation
- Prolonged immobilization
- Varicose veins
- Thrombophilia
The difficulty of treating HTO during pregnancy is as follows:
- Direct dependence on the duration of pregnancy (safe periods of pregnancy for active treatment tactics 7-8 weeks, 13-17 weeks, 23-27 weeks)
- Difficulty in selecting the type and dosage of an anticoagulant
- High probability of miscarriage and/or complications
- The need to resolve the complex issue of choosing treatment tactics
- The ethical problem of choosing to preserve life
- The problem of achieving compliance with the patient and her relatives
As for varicose veins of the lower extremities during pregnancy, this problem is very extensive and controversial. Patients with varicose veins who are planning a pregnancy should be clearly aware of the risks, adequately assess the danger that the disease poses not only to the mother, but also to the unborn child, so as not to then place all responsibility on doctors, who in this case will have very limited possibilities. Such responsibility, first of all, should lie with the parents of the unborn child. Experts always insist that varicose veins be cured before pregnancy, then there will be no corresponding risk.
On the one hand, the presence of varicose veins is the main risk factor for the occurrence of VTO, i.e. there is a strict need to prevent such complications - surgical treatment. On the other hand, during pregnancy, the possibilities of surgical treatment are sharply limited by the safe periods of pregnancy. And if before pregnancy the patient has a fairly large choice in treatment methods, then if complications of varicose veins occur during pregnancy, for example thrombophlebitis, the only possible method of removing the veins will be a standard operation, and this means general anesthesia and the need to prescribe medications, which is a direct threat to the fetus, and in addition, severe surgical trauma, causing certain changes in the body that are clearly not beneficial to the pregnant woman and the fetus. In this case, modern low-traumatic methods of surgical treatment - EVLO and RFO - will have a clear advantage, because they do not require the use of general anesthesia and the prescription of a significant amount of medication, and also do not cause significant surgical trauma and are safe. However, in this case, given the constant growth of the pregnant uterus and progressive changes in venous circulation with a sharp increase in pressure in the veins, the likelihood of a relapse of the disease is very high. An important factor will be certain conditions and technical capabilities for performing such an intervention.
Therefore, if a patient with varicose veins seeks help during pregnancy, in most cases conservative methods of prevention are still prescribed, as a rule - compression therapy, taking phlebotropic drugs during safe periods of pregnancy, dynamic observation with an objective assessment of the condition. In the absence of complications during pregnancy, surgical treatment is prescribed after the period of breastfeeding. However, the high risk of VTO with varicose veins in pregnant women remains, even with compression therapy, especially in the presence of several risk factors, which we mentioned above.
For example, the standard for preventing VTO in Europe in the presence of several risk factors for thrombosis, in the presence of varicose veins, is to prescribe daily injections of drugs that “thin” the blood for the ENTIRE period of pregnancy! Is it really worth not having your varicose veins operated on before pregnancy, using modern methods, quickly, painlessly, and then being absolutely calm both for yourself and for your unborn child?!
So, the main measure to prevent the development of VTO in the presence of varicose veins is timely and adequate treatment (timely surgical treatment, compliance with compression therapy, correction of the rheological properties of blood and blood coagulation processes, active lifestyle).
How to treat varicose veins of the labia and perineum?
Unfortunately, if varicose veins have already appeared during pregnancy, they are unlikely to disappear before childbirth. However, it is within our power to alleviate the symptoms associated with it.
The doctor will prescribe appropriate treatment that will not harm the mother and baby and can reduce pain and improve the condition of blood vessels.
The doctor will also teach you how to carry out preventive measures to prevent worsening of the condition and the occurrence of complications:
- exercises that reduce pressure in dilated veins,
- wearing special bandages.
- special bondage for the prevention of varicose veins of the perineum special bondage for the prevention of varicose veins of the perineum special bondage for the prevention of varicose veins of the perineum
- For vascular decompression, a supine position with legs raised and pelvis up (placing a pillow under the pelvic area) is recommended. It is enough to repeat this exercise several times a day, for several minutes.
- Lying on your left side, with your knees bent and pulled towards your stomach, also helps.
- During the day, avoid prolonged standing, sitting, and tight, tight clothing and underwear.
- Hot baths should be avoided.
Varicose veins of the labia, as a rule, are not dangerous and disappear in most cases spontaneously after childbirth. If varicose veins do not disappear after childbirth, they can be treated with foam sclerotherapy.
- Treatment is carried out on an outpatient basis, without anesthesia and rehabilitation
- A sclerosing substance in the form of foam is injected into the dilated vein, after which a bodysuit (or a special bandage) is put on.
- The patient leads a normal lifestyle, without any restrictions.
- The process of sclerosis occurs within 2-4 weeks, after which the dilated vein and all the symptoms that previously bothered the patient disappear.
Childbirth with varicose veins
Women with a predisposition to varicose veins also need medical supervision. Although the natural course of delivery is often accompanied by premature breaking of waters, short duration of contractions, postpartum hemorrhage, placental abruption, doctors strive to ensure the birth of the child naturally.
The uncomplicated course of varicose veins allows women to count on a natural course of childbirth. To prevent the backflow of blood into the veins during pushing, it is necessary to bandage both legs of the woman in labor with elastic bandages, or use compression stockings.
Expectant mothers must undergo laboratory tests to determine blood clotting. If a tendency towards increased coagulation is detected, the doctor prescribes medications to correct it and means to reduce platelet aggregation.
In the postpartum period, women need to get out of bed early, visit the physical therapy room, and continue elastic leg bandaging. If surgical delivery has taken place and there are significant disturbances in the blood coagulation system, drug treatment continues. In case of complex course of varicose veins, if the situation does not change after childbirth, they resort to surgical intervention.
To prepare for the birth of a child, it is useful for a woman to take walks lasting up to two hours, this helps improve blood circulation.
You need to give up heels and wear comfortable, stable shoes. Every day you need to give your legs a rest by placing your feet in an elevated position. For a good night's rest, it is advisable to place a small pillow under your stomach and legs. It is useful for a pregnant woman to visit the pool and use a contrast shower.
Pregnancy is characterized by changes in the hormonal background of the female body. A decrease in the amount of estrogen and an increase in the amount of hormones, relaxing the walls of blood vessels, leads to their varicose veins.
Regular visits to the doctor for examination help to promptly identify disorders that can lead to varicose veins. This may be an increase in venous pressure levels, slowing
blood circulation in the legs, which leads to the occurrence of disease. Varicose veins contribute to placenta previa or low position. This doubles the risk of complications during pregnancy and childbirth. Regular examinations, maintaining a healthy lifestyle and following all medical recommendations contribute to the birth of a healthy baby during natural delivery.
How is foam sclerotherapy performed?
In one session, 2-4 ml of sclerosing solution is injected into the vein, after which the vein is pressed with a gauze ball. A compression bandage is then applied to the patient, and after a short time the vein completely disappears. In addition, the pain and feeling of heaviness go away. The indisputable advantage of foam sclerotherapy is the absence of postoperative wounds, scars and associated complications. In one session, 2 to 4 injections are given, depending on the nature of the lesion. After a few days, the procedure is repeated.
The main recommendation for the patient after completing the session is to walk for several hours. It helps to avoid thrombosis of veins - deep and muscular. In addition, compression of the thigh and lower leg is important throughout the course of treatment and several weeks after its completion. For this purpose, special compression hosiery or elastic bandaging is used.
Phlebologist Khairbeik Aksam Ali Phlebologist of the highest category. Successfully performed more than 1000 sclerotherapy procedures. Work experience – more than 25 years.
Effective treatment at the Professor Gorbakov Clinic
At the Professor Gorbakov Clinic, treatment of veins of the perineum, buttocks and labia is carried out by high-level specialists using foam sclerotherapy. This method is a worthy alternative to surgical interventions, which require hospitalization and rehabilitation.
With the help of foam sclerotherapy, both large and small dilated veins are eliminated. The essence of the method is the introduction of a special drug – sclerosant. As a result, the affected vein narrows and ceases to function, and the outflow of blood occurs through healthy veins.
The procedure is almost completely painless due to the fact that microcatheters and special thin needles are used to perform it. The treatment is carried out on an outpatient basis and gives positive results - both therapeutic and cosmetic.