© Author: A. Olesya Valerievna, candidate of medical sciences, practicing physician, teacher at a medical university, especially for SosudInfo.ru (about the authors)
Cerebrasthenic syndrome (CAS, cerebrasthenia) is a complex symptom complex that includes a variety of psycho-emotional abnormalities, behavioral disorders, reduced mental performance and learning ability. Patients with cerebrasthenic syndrome are usually seen by a neurologist.
Among patients diagnosed with CSA, children predominate. This is no coincidence, because the child’s brain is very susceptible to adverse effects not only in the first years of life, but also at the stage of formation of the nervous system during intrauterine development.
Cerebral asthenia is based on organic brain damage , and its manifestations can be so diverse that an accurate diagnosis is not always made on time. Adults attribute its manifestations to fatigue, age, past injuries or infections, without paying due attention to the progression of the pathology.
This condition deserves special caution in pediatrics. Children suffering from mild forms of cerebrasthenic syndrome experience learning difficulties, are disobedient, and capricious, but parents may not attach much importance to these symptoms in the hope that the child will “outgrow” everything.
With cerebrovascular disease, patients need not only appropriate treatment, but also a special lifestyle, the attitude of relatives and friends, and understanding from teachers. In this regard, timely diagnosis of CSA and informing relatives about the features of the pathology acquire great meaning.
Cerebrasthenic syndrome: causes, symptoms, diagnosis
Brain weakness in cerebrasthenic syndrome (CAS) develops due to a complex symptom complex of organic intracerebral disorders.
The pathology is typical for children. It manifests itself as a disturbance in the duration of sleep and wakefulness, and a complex of associated complications. Due to increased sleepiness, activity and performance decreases.
Timely detection by MRI of the brain in St. Petersburg, competent treatment, and the correct attitude towards a sick child on the part of loved ones can reduce the rate of progression.
It is necessary to take into account the likelihood of the occurrence of CSA not only in utero, after birth, but also during growth. Children's brain tissue at all stages is subject to the influence of unfavorable factors, as it is in a phase of constant formation.
Cerebrovascular disease in adults occurs due to environmental influences and brain diseases (hypoxia, microstroke, arteriovenous malformation).
The variety of symptoms does not allow timely diagnosis. Practice shows the possibility of correcting mild manifestations of CSA in children if detected in a timely manner. Parents believe that the child will “outgrow” the condition - this is a big mistake. Brain disorders progress, the size of the lesion increases.
If the cause of the nosology is an infection, you need to take antibacterial drugs. Destroying the pathogen will restore the physiological functioning of the brain.
Main causes of asthenia
In medicine, asthenic syndrome is one of the most common. It is observed in a variety of therapeutic, neurological, infectious diseases, some mental disorders, in the post-traumatic, postoperative and postpartum periods. Therefore, doctors of various specializations deal with asthenia. Asthenia can be the first symptom of the onset of the disease, accompany it during the period of activity and occur during recovery.
In addition, important factors leading or potentiating its development are:
- unbalanced or insufficient nutrition and nutritional deficiencies;
- metabolic disease;
- intoxication;
- high stress (both physical and mental);
- chronic stress condition;
- mental disorders;
- acute diseases and exacerbation of chronic diseases.
Therefore, it is very important to be attentive to the needs of your body, take care of your condition, provide yourself with the necessary help in time to improve your health, and restore strength when needed!
Classification of cerebrasthenic syndrome according to ICD 10
The group of brain diseases with primary lesions, secondary forms, according to the international classification of diseases, belongs to group “F”. The category also includes hormonal, inflammatory, and somatic nosologies. Cerebral damage is caused by alcohol abuse and the influence of psychoactive substances.
ICD 10 code:
- Hallucinosis of organic etiology – F06.0;
- Catatonic syndrome – F06.1;
- Schizophrenia-like disorder –F06.2;
- Affective pathology of mood – F06.3;
- Anxiety disorder (organic) – F06.4;
- Dissociative syndrome – F06.5;
- Asthenic emotionally labile pathology (cerebrovascular disease) – F06.6;
- Cognitive defect (mild) – F06.7;
- Other somatic dysfunctions of the brain – F06.8;
- Unspecified mental pathology with brain dysfunction – F06.9.
It is difficult to differentiate groups of nosologies at the beginning of development due to a variety of minor symptoms.
Diagnostics
Doesn't present much difficulty. The task falls on the shoulders of the neurologist. Child or adult. Among the measures to identify the problem:
- Oral questioning of the patient or his parents. In the latter case, it is important that the father or mother carefully observe the child’s condition in order to formulate complaints and describe behavior.
- Anamnesis collection. The moment of onset of the disorder, family history of diseases, especially the course of pregnancy and childbirth in the mother, these are the main factors that are clarified.
- Dopplerography of cerebral vessels. It is necessary to assess the quality and speed of blood flow in cerebral structures.
- MRI. For high-precision imaging of nerve tissue. In detail. Using this method, it becomes possible to detect minimal structural changes in any area.
- Encephalography. It is prescribed to study the electrical activity of the brain.
In general, this is enough to make a diagnosis. There are no differences in the examination of adults and children. In some cases, it makes sense to undergo additional procedures. But this is rather an exception.
Causes of CAS
In adults, the etiological factor of the pathology is atherosclerotic and post-traumatic cerebrovascular disease. The accumulation of fatty deposits inside the lumen of the cerebral vessels provokes blood flow disturbances. Over time, wall plaques accumulate calcium and become dense. Only surgery can eliminate the blockade of cerebral microcirculation in atherocalcinosis. The operation of stenting or bypassing a vessel involves removing the damaged part and replacing the area with an artificial prosthesis.
Post-traumatic cerebrasthenic syndrome after traumatic brain injury (TBI) is caused by compression of the brain by hematoma, bone fragment, and foreign bodies. The absence of skull fractures does not mean the normal state of the cerebral parenchyma. At the moment of impact, the brain is displaced. Counter-impact from the opposite side causes rupture of blood vessels and hemorrhagic impregnation of tissues.
Causes of CSA in children:
- In newborns, the etiological nosology factor is intrauterine conditions - infection of the pregnant mother, taking pharmaceuticals, circulatory abnormalities, compression of the baby's head during childbirth;
- In preschoolers and schoolchildren, the cause of the nosology is acquired infection, skull injuries - meningitis, tick bites, poisoning;
- In adolescents - concussions, bacterial infections;
- Adults suffer from atherosclerosis, viral and bacterial diseases.
The most common causes of cerebrasthenic syndrome at different age intervals:
- Deposition of fatty plaques inside the artery;
- Traumatic brain injury (TBI);
- Infections of the membranes (encephalitis, meningitis);
- Poisoning, intoxication;
- Taking medications that affect brain tissue;
- Asphyxia of newborns;
- Birth injuries;
- Intrauterine hypoxia.
The child's fragile nervous tissue is sensitive to lack of oxygen. Prolonged hypoxia leads to ischemic changes, impaired blood supply, and death of parenchyma.
School maladjustment in pediatric practice
The beginning of schooling places new, more complex demands on the child’s personality and intellectual capabilities. This is due to the transition to a completely different set of mental, emotional and physical stress compared to the previous conditions of raising children in the family and preschool institutions.
Parents often come to consult a doctor whose children have a normal level of mental development and are quite capable of studying in a comprehensive school, but at the same time cannot successfully cope with the volume of educational loads or master school skills; in addition, they are often characterized by problems associated with inappropriate behavior. Often teachers in preschool institutions begin to pay attention to such difficulties in children when conducting various developmental activities, including in preparation for school.
In recent years, difficulties arising in the process of schooling have become the focus of attention not only of teachers and psychologists, but also of doctors. The causes of school maladjustment (SD) in children can be of a completely different nature. But at the same time, their external manifestations, which teachers and parents pay attention to, are similar. It is customary to consider the following main criteria and forms of manifestations of SD.
- Cognitive, or cognitive, component - poor academic performance in programs appropriate to the child’s age and abilities, with insufficient knowledge and development of learning skills, chronic academic failure.
- The personal, emotional and evaluative component of SD is constant violations of the emotional and personal attitude towards individual subjects and learning in general, teachers, as well as prospects related to studies.
- The behavioral component of SD is systematic violations of behavior during the learning process and at school.
In most children with SD, all three of the above components can be clearly seen. The predominance of one or another component among the manifestations of SD depends, on the one hand, on age and stages of personal development, and on the other, on the reasons underlying SD.
In their practical work, pediatricians, school doctors, pediatric neurologists and psychologists most often have to deal with conditions leading to the formation of SD, such as asthenic syndrome, cerebrasthenic syndrome, and minimal cerebral dysfunction. Less commonly, the cause of SD is various mental illnesses, if suspected, the child should be promptly referred for consultation with a psychiatrist.
If difficulties in learning are associated with low and unstable performance, high fatigue, insufficiently developed ability to control one’s activities, and a slow pace of assimilation of educational material, then after an appropriate examination, in many cases asthenic or cerebrasthenic syndrome is diagnosed. The development of asthenic syndrome is associated with somatic pathology. In cerebrasthenic syndrome, deviations in the processes of maturation and functioning of the central nervous system (CNS) are associated with its organic damage.
Asthenic syndrome
Symptoms of an asthenic nature are often one of the first nonspecific manifestations of a wide range of somatic disorders. Somatogenic asthenic conditions can be associated with unbalanced nutrition (protein-calorie deficiency, deficiency of vitamins, microelements), disorders of food absorption (malabsorption syndrome) in chronic diseases of the gastrointestinal tract, metabolic pathologies, with frequent colds and chronic infectious diseases (sinusitis, tonsillitis, etc.). Manifestations of asthenic syndrome are often observed in diseases of the respiratory system, bronchial asthma, diseases of the cardiovascular system, blood diseases, anemia, chronic diseases of the liver, pancreas, kidneys, endocrine pathology (thyroid diseases, diabetes mellitus).
Clinical manifestations of asthenic syndrome are increased fatigue, difficulty concentrating, and delayed perception. Children with asthenic syndrome stand out among their peers for their behavior: along with lethargy and exhaustion, many of them are overly shy, indecisive, and fearful. They are characterized by emotional lability, high vulnerability and touchiness. Children get upset over every trifle and start crying at the slightest failure. Hyperesthesia is often observed, expressed in intolerance to irritants such as loud sounds, bright light, and certain odors. Complaints of headaches may be due to other children making a lot of noise.
Asthenic symptoms in some cases are combined with anxiety, suspiciousness, and obsessive fears. Sleep disorders often occur. Sleep becomes superficial, restless, and is often accompanied by frightening dreams. Children have trouble falling asleep and have difficulty waking up, and there is no feeling of rest after sleep. Drowsiness may occur during the daytime.
Treatment is largely determined by timely diagnosis and treatment of primary somatic pathology, as well as the characteristics of the course of the underlying disease. Nootropic drugs are highly effective in treating manifestations of asthenic syndrome.
Cerebrasthenic syndrome
The discovery in a child during examination of mild residual manifestations of organic damage to the central nervous system usually serves as the basis for diagnosing cerebrasthenic syndrome. The causes of the development of cerebrasthenic syndrome include various forms of pathological course of pregnancy and childbirth associated with impaired oxygen supply to the brain of the fetus and newborn. Asphyxia in a full-term newborn almost always has an intrauterine origin; hypoxia and ischemia develop simultaneously; the result is hypoxic-ischemic encephalopathy. Other pathological conditions include intrauterine infections, taking medications by pregnant women, prematurity, and in newborns - intracranial hemorrhage, hemolytic disease, sepsis, and pneumonia.
Cerebrasthenic syndrome develops in most children who have suffered traumatic brain injury (TBI), neuroinfections (meningitis, encephalitis) or general infections with toxic brain damage. The uniqueness of the clinical course and outcomes of TBI in children is due to the fact that mechanical energy affects the brain, the growth and development of which is not yet complete. In the clinical course of TBI, three periods are distinguished: acute - the first 2-10 weeks, intermediate - 10 weeks-6 months, long-term - from 6 months to 2 or more years. Even mild TBIs do not go away without leaving a trace in childhood. Thus, approximately 1/3 of children who have suffered a concussion in the long term have complaints of headaches, increased fatigue, and difficulties in school learning (the so-called “post-concussion syndrome”). Moderate and severe TBIs lead to more serious consequences, but at the same time, in children, more often than in adults, a favorable outcome is possible even after severe TBI, due to the high compensatory capabilities and plasticity of the developing brain. To prevent persistent cognitive impairment in the long-term period of TBI, attention should be paid to the presence of manifestations of cerebrasthenic syndrome in the intermediate period of TBI, which are an indication for therapeutic courses with nootropics.
Cerebrasthenic syndrome develops in many children after various surgical operations. Its trigger is various types of hypoxia during surgery: anemic, circulatory, histotoxic. In the postoperative period, various extracerebral factors continue to operate: hypovolemia, surgical bleeding, dysfunction of the cardiovascular system and acid-base balance, hypoxemia.
A typical manifestation of cerebrasthenic syndrome is the so-called “irritable weakness.” On the one hand, children are characterized by general passivity, lethargy, slowness in thinking and movement; even with minor neuropsychic stress, exhaustion is observed, and the mood level is reduced. Fatigue is sometimes so severe that children are contraindicated from staying with their peers for a long time. On the other hand, there is increased irritability, readiness for affective outbursts, and insufficient criticality.
The occurrence of asthenic symptoms against the background of organic changes in the central nervous system gives the cerebrasthenic syndrome a number of features. Weakness of attention and thinking is accompanied by a fairly pronounced and long-term decrease in mental performance, especially with any intellectual load in school-age children. Memory loss is often noted.
It is believed that increased excitability, irritability, affective explosiveness, as well as hyperesthesia to sounds and bright light are more characteristic of post-traumatic cerebrospinal fluid. With post-infectious cerebrasthenia, mood swings are more often observed, accompanied by tearfulness, moodiness, and dissatisfaction. Children with consequences of intrauterine brain lesions may exhibit various dysembryogenetic stigmas. The structure of cerebrasthenic syndrome also includes more or less pronounced disorders of autonomic regulation.
Frequent manifestations of cerebrasthenia are headaches, worsening in the afternoon due to fatigue, and vestibular disorders (dizziness, a feeling of lightheadedness when driving, accompanied by nausea). In addition to driving, swings, heat and stuffiness, and weather changes with sharp fluctuations in atmospheric pressure are poorly tolerated.
Course of cerebrasthenic syndrome
As the central nervous system develops, various mechanisms of compensation for residual cerebral insufficiency are activated, therefore, the manifestations of cerebrasthenic syndrome are characterized by gradual regression. However, periods of decompensation may occur, especially during age-related crises. In addition to age-related physiological changes, the causes of decompensation can be fatigue associated with educational overload, psychotraumatic situations, various somatic diseases, and infections. Timely prescribed therapy with the inclusion of nootropic drugs contributes to the earliest and complete compensation of these disorders.
Minimal brain dysfunction (MCD) is the most common form of neuropsychiatric disorders in childhood. MMD are usually the consequences of early brain damage; their main characteristic is the age-related immaturity of individual higher mental functions and their disharmonious development. MMD is accompanied by a delay in the rate of development of functional brain systems that ensure the implementation of higher mental functions: speech - oral and written, attention, memory, perception, executive functions (programming, regulation and control) and a number of others. In terms of general intellectual development, children with MMD do not lag behind their peers, but at the same time experience significant difficulties in school learning and social adaptation.
The main clinical variants of MMD among school-age children are represented by attention deficit hyperactive disorder (ADHD), as well as specific difficulties in developing writing, reading and arithmetic skills - dysgraphia, dyslexia and dyscalculia. It is generally accepted that the pathogenesis of MMD is associated with the impact of various pathological factors on the developing brain during pregnancy and childbirth. The central nervous system is especially vulnerable when oxygen deficiency occurs, and biochemical and morphological changes caused by hypoxia can, to one degree or another, distort the normal course of complex processes of brain development. At the same time, studies in recent years have confirmed the significant role of hereditary mechanisms in the formation of MMD.
Attention deficit hyperactive disorder is manifested by motor hyperactivity unusual for normal age indicators, defects in concentration, distractibility, impulsive behavior, problems in relationships with others and learning difficulties. Children with ADHD are also distinguished by their awkwardness and clumsiness, which are associated with insufficient development of motor coordination. The prevalence of ADHD is quite high - 3-5% of school-age children. ADHD is 5–7 times more common among boys than among girls.
Hyperactivity is characterized by the fact that children are extremely active, constantly running, spinning, and trying to climb somewhere. Parents are oh, unable to sit still. Hyperactivity is also manifested by restlessness and extraneous movements during tasks that require perseverance (fidgeting in a chair, unable to keep arms and legs motionless). These children often experience a combination of excessive motor activity and destructive behavior. Thus, at school they constantly disturb teachers and provoke misbehavior among classmates.
Defects in concentration are the cause of poor performance in school lessons. According to teachers' descriptions, children with ADHD are able to maintain attention for no more than a few minutes. At the same time, indicators of concentration in children with ADHD are also subject to significant fluctuations. Parents often report that during activities and games that children are able to successfully complete, they can maintain attention for up to several hours. Such “selectivity” of attention is associated with interest, enthusiasm and pleasure from this activity. Hyperactive children perform worst on tasks that seem boring and difficult to them.
Impulsivity in such children is constantly observed both in a variety of everyday situations and when completing school assignments. During lessons, children have difficulty waiting their turn, interrupt others, answer questions inappropriately, without listening to them fully. Due to their impulsiveness, they are prone to traumatization, as they often commit dangerous actions, the consequences of which they do not think about. At the same time, impulsiveness provokes constantly emerging problems in relationships with others, including parents, brothers and sisters, and teachers. In a group, a child with ADHD is a source of constant anxiety: he makes noise without thinking, takes other people’s things, disturbs others, distracting them. All this leads to conflicts, as a result of which the child feels unwanted and rejected. Most children with ADHD are characterized by low self-esteem and weak psycho-emotional stability in the face of failures.
During school hours, children with ADHD find it difficult to cope with the assigned tasks, as they have difficulty organizing and completing work. Their reading and writing skills turn out to be much less developed than those of others. Written work is sloppy and prone to errors, which may be the result of inattention, failure to follow teacher instructions, or guessing without considering all possible options. At the same time, children are not inclined to listen to the advice and recommendations of adults. The difficulties in developing writing and reading skills in attention deficit hyperactivity disorder, along with attention disorders, are based on insufficient coordination of movements, visual perception and speech development.
In recent years, standardized diagnostic criteria for ADHD have been developed, representing a list of the most characteristic and clearly visible signs of this disorder. The diagnosis of ADHD is based on the criteria of the 10th revision of the International Classification of Diseases (WHO, 1994).
Attention-deficit hyperactive disorder: diagnostic criteria
I. Attention disorders
- Often unable to concentrate on details; due to negligence and frivolity, he makes mistakes in school assignments, work and other activities.
- Usually has difficulty maintaining attention when completing tasks or playing games.
- Often it seems that the child does not listen to those who address him.
- Often it is not possible to adhere to the proposed instructions and fully cope with lessons, homework or duties at the workplace (which has nothing to do with negative or protest behavior, or an inability to understand the task).
- Often has difficulty organizing independent completion of tasks and other activities.
- Typically expresses dissatisfaction and resists involvement in tasks that require prolonged attention (eg, school assignments, homework).
- Often loses things needed at school and at home (for example, toys, school supplies, pencils, books, work tools).
- Easily distracted by extraneous matters, objects, etc.
- Often shows forgetfulness in everyday situations.
II. Hyperactivity
- Restless movements of the hands and feet are often observed; sitting on a chair, spinning, spinning.
- Frequently gets up from his seat in the classroom during lessons or in other situations.
- Often exhibits aimless motor activity: runs, spins, tries to climb somewhere, and in situations where this is unacceptable.
- Usually cannot play quietly or quietly or do leisure activities.
- He is often in constant motion and behaves “as if he had a motor attached to him.”
Impulsiveness - Often talkative.
- Often answers questions without thinking, without listening to them completely.
- Usually has difficulty waiting his turn in various situations.
- Often interferes with others, pesters others (for example, interferes in conversations or games).
To make a diagnosis, six or more of the nine listed symptoms of attention disorders and/or six or more of the nine listed symptoms of hyperactivity and impulsivity must be present. The child's symptoms must persist for at least 6 months. In cases where the observed clinical picture fully corresponds to all of the listed diagnostic criteria simultaneously, a diagnosis of a combined form of ADHD is made. If there are six or more symptoms of attention impairment and less than six symptoms of hyperactivity, the diagnostic formulation “ADHD with predominant attention impairment” is used. If there is full compliance of symptoms with the criteria for hyperactivity and partial compliance with the criteria for attention impairment, then the diagnosis is designated as “ADD with a predominance of hyperactivity and impulsivity.”
In clinical practice, we most often encounter children's hyperactivity and attention disorders caused by ADHD. However, in addition to ADHD, these disorders can serve as external signs of a number of other conditions.
Differential diagnosis of hyperactivity and attention deficit in children
- Individual characteristics of temperament: characteristics of behavior and cognitive functions of active, active children do not go beyond the boundaries of the age norm.
- Anxiety disorders: the child’s behavioral characteristics are associated with the action of psychotraumatic factors.
- Asthenic syndrome in somatic diseases.
- Cerebrasthenic syndrome: residual effects of traumatic brain injury, neuroinfection, intoxication.
- Endocrine diseases (thyroid pathology, diabetes mellitus).
- Sensorineural hearing loss.
- Epilepsy (absence forms; symptomatic, locally caused forms; side effects of antiepileptic therapy).
- Mental disorders: behavioral disorders; affective disorders (moods); mental retardation; autism; schizophrenia.
- Hereditary syndromes: Tourette, Williams, Smith-Magenis, Beckwith-Wiedemann, fragmental X chromosome and some others.
It is necessary to carefully distinguish between ADHD and a wide range of conditions that are similar to it only in their external manifestations, but differ significantly from ADHD both in the causes of occurrence and methods of correction. It is all the more important to take this into account because in recent years there has been a tendency towards an unreasonably frequent diagnosis of ADHD and the misconception that diagnosing ADHD does not present significant difficulties has become widespread.
By adolescence, hyperactivity in children with ADHD significantly decreases or disappears, but attention disorders continue to varying degrees until adulthood. A number of adolescents are experiencing increasing behavioral disturbances, aggressiveness, difficulties in relationships in the family and school, and academic performance is deteriorating. Irresponsible behavior, violation of family and social rules, significant difficulties in choosing and mastering a profession are often observed, and there is often a craving for alcohol and drug use. In this regard, the efforts of parents and specialists should be aimed at timely identification and correction of ADHD. Nootropic drugs are highly effective in the treatment of ADHD. It is advisable to conduct nootropic courses several times a year during periods of the most intense training loads.
At preschool age, the child masters oral speech. Upon entering school, he begins to master visual (written) images of letters. The perception and recognition of graphic images necessary for written language (reading and writing) occur in the visual area of the cerebral cortex (occipital lobe). This means that the visual analyzer is included in the work of the speech system of the brain, and its functions must be coordinated with the activities of the speech-auditory and speech-motor analyzers. The child needs to learn to translate a heard and spoken word into a visual image (writing) and vice versa, be able to translate a visual image into an articulatory and auditory one (reading).
Reading and writing are among the newest higher mental functions in phylo-ontogenesis, which are mastered in the process of special training. In their implementation, the most late-forming parts of the cerebral cortex, mainly the parietotemporal-occipital region of the left hemisphere, are of primary importance. In addition, the implementation of these functions becomes possible with close interaction between the visual, auditory and motor analyzers, as well as with a sufficient level of development of complex voluntary actions (eye movements along lines of text, coordinated movements of the hand and eyes when writing).
Dyslexia is a partial specific disorder of the reading process and one of the forms of underdevelopment of written speech, manifested in repeated persistent errors. Children with dyslexia experience significant difficulties in mastering the skill of reading and, as a rule, writing, despite the normal level of intellectual development, the absence of impairments in the visual and auditory analyzers and pedagogical neglect. Dyslexia in children is the inability to achieve a level of development in reading, writing and spelling skills that is proportional to their mental abilities. In other words, dyslexia is often accompanied by dysgraphia and dysorthography. The incidence of dyslexia has not been definitively established. Based on studies of school-aged children, estimates of the prevalence of dyslexia range from 5–10 to 15–20%.
After 1–1.5 years of schooling, almost 50% of children with dyslexia do not have reading skills. Some of them do not know the letters, and the rest, having learned part of the alphabet, read only short, familiar words, the images of which they have memorized globally, like a picture. 25% of children master slow syllabic reading, making a large number of errors, the rest read letter by letter. As a result, children with dyslexia are unable to understand the meaning of what they read.
Dysgraphia is a violation of the development of writing processes and one of the forms of underdevelopment of written speech, manifested in repeated errors of a persistent nature. There are optical, phonemic and grammatical (dysorthography) types of errors in writing. In case of optical errors, graphically similar letters are not distinguished: p-n, p-i, p-t, u-i, sh-i, m-sh, m-l, l-i, b-d, etc. With phonemic ( errors in the perception of speech sounds) - phonemes that have acoustic-articulatory similarities are not distinguished, most often voiced and voiceless: d-t, z-s, b-p, zh-sh, g-k, v-f, etc.
Difficulties in mastering reading and writing skills can have a negative impact on the development of a child's personality. Constant failures in school can cause and reinforce such traits as uncertainty, anxiety, isolation, and low self-esteem. In some cases, especially when there is an incorrect attitude towards the child’s difficulties on the part of adults, both parents and school teachers, accusing him of reluctance to learn, slowness, laziness and disobedience, children with dyslexia and dysgraphia develop neurotic, depressive states or oppositional and aggressive behavior. Timely use of nootropics in the treatment of dyslexia and dysgraphia in children contributes to the most complete correction of these conditions. It is necessary to take into account that the manifestations of dyslexia and dysgraphia are usually characterized by persistence and cannot be completely overcome in a short time.
Providing assistance to children with SD should be timely, comprehensive and combine various approaches, including methods of psychological and pedagogical correction, psychotherapy, and drug treatment. All children with SD should be examined by a psychologist. In order for assistance to a child to be effective, coordinated efforts of various specialists are necessary - doctors, psychologists, speech therapists, teachers. It is important that the joint efforts of specialists are aimed at early detection and correction of cognitive, emotional and behavioral disorders in children. Planning and implementation of corrective measures, including drug therapy, should be carried out according to individual plans for each child.
Nootropic drugs are a relatively new group of drugs that entered widespread pediatric practice in the 1980s. According to WHO experts, nootropic drugs are drugs that have a direct activating effect on learning, improve memory and mental activity, and also increase the brain’s resistance to adverse effects. Based on their chemical structure, nootropics represent a heterogeneous group of drugs. The main nootropics include the following classes of drugs: 1 - pyrrolidone derivatives (piracetam), 2 - γ-aminobutyric acid (GABA) derivatives (phenibut, pantogam), 3 - neuropeptides and their analogues (Cerebrolysin, Semax), 4 - pyridoxine derivatives ( encephabol), 5 - cerebrovascular drugs (nicergoline, vinpocetine), 6 - multicomponent drugs (instenon, actovegin) and a number of others. The high effectiveness of nootropic drugs in combination with good tolerability has been confirmed in many studies that assessed their effect in the treatment of various conditions accompanied by difficulties in development, learning and behavior in children.
Most nootropic drugs are prescribed in the first half of the day due to their psychostimulating effect. It is advisable to use nootropic drugs in the form of monotherapy, while paying attention to the individual selection of optimal dosages and duration of treatment. In the first days of use, a gradual increase in dose is recommended. The duration of nootropic treatment courses ranges from 1 to 2–3 months. If during the school year there is a need for several courses of treatment, then intervals of 2–4 weeks are left between them, which are best planned during the holidays. If the first course of treatment turns out to be insufficiently effective, then the issue of increasing the duration of treatment, prescribing a second course of nootropics after a break, or combining pharmacotherapy with methods of psychological and pedagogical correction should be decided individually.
It is important to note that side effects during treatment with nootropics in children are rare and are not persistent or significantly pronounced. They often occur when parents do not accurately follow nootropic regimens with a gradual increase in dose, taking drugs in the morning and afternoon. Possible side effects of nootropics include: a feeling of heaviness in the head, the appearance of excitability and irritability, difficulty falling asleep and restless sleep, rarely - nausea, discomfort in the stomach. If such complaints appear, clarifications should be made to the nootropic prescription regimen, and in some cases, the dose should be slightly reduced. Certain caution is required in prescribing nootropic drugs to patients with manifestations of intracranial hypertension. In such cases, at the first stage of treatment, dehydration therapy is prescribed or nootropics are used in combination with it.
In conclusion, it is necessary to emphasize once again that identifying the causes of SD and correcting its manifestations must be timely. Patients with SD are recommended to undergo a comprehensive examination with the participation of a pediatrician, neurologist, psychologist, and, if indicated, a psychiatrist. All children with SD require dynamic monitoring not only by a doctor, but also by a psychologist.
Our experience in the use of nootropic drugs indicates the positive effect of encephabol and instenon in the treatment of these conditions in children.
Encephabol (pyritinol) is a nootropic drug whose chemical structure is a double molecule of pyridoxine (vitamin B6).
Features of prescribing encephabol
- Release forms: tablets of 100 mg and suspension containing 20 mg of encephabol in 1 ml.
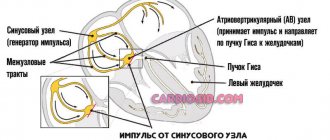
- Mechanisms of action: improves the transmission of impulses and their conduction to various parts of the brain, normalizes the energy metabolism of neurons, activates glucose metabolism in brain tissue, improves microcirculation in the brain.
- Minimum contraindications, approved for use from an early age.
- Recommended doses for children: up to 10–12 mg/kg body weight (daily dose up to 300–400 mg), in 2–3 doses, after meals, the last dose no later than 17:00.
- To avoid side effects at the beginning of the course, it is recommended to slowly increase the dose of encephabol over 7–10 days.
- Course duration is up to 6–12 weeks.
Encephabol is highly effective in the treatment of asthenic and cerebrasthenic syndromes, dyslexia and dysgraphia, ADHD.
If there are appropriate indications, long-term use is advisable, allowing to achieve a significant increase in performance, improvement in the state of higher mental functions and school learning skills.
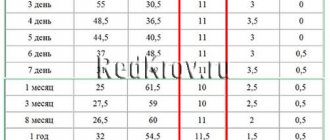
| Instenon dosage regimens for children of different age groups |
Instenon is a multicomponent nootropic drug; in pediatric practice, a tablet form is used containing 1 tablet 50 mg of etamivan, 20 mg of hexobendine, 60 mg of etophylline. Instenon is especially effective in the treatment of ADHD and can be recommended for the treatment of asthenic and cerebrasthenic syndromes. Depending on age, the daily dose is 1.5–2.5 tablets, prescribed in 2 doses (morning and afternoon) after meals. It is recommended to begin therapy with a gradual increase in dose over 7–10 days. The duration of treatment is from 4 to 6–8 weeks. Instenon dosage regimens for children of different age groups are given in the table.
N. N. Zavadenko , Doctor of Medical Sciences, Professor of Russian State Medical University, Moscow
The first signs of cerebrasthenic syndrome
Early manifestations allow one to suspect CAS in adults:
- Deterioration of condition after staying in stuffy rooms;
- Bad mood during the heat;
- Dizziness, weakness when changing atmospheric pressure;
- Constant feeling of fatigue;
- Desire to rest;
- Development of vegetative-vascular dystonia (VSD);
- Causeless nausea;
- Irritability;
- Emotional instability;
- Deterioration of intellectual activity;
- Memory impairment.
Vegetative-vascular dystonia is accompanied by a change in the balance between the sympathetic and parasympathetic components of the central nervous system (CNS). The nosology manifests itself as redness of the skin, an imbalance in the innervation of internal organs with an increase in heart rate and respiratory movements.
Let's understand the terms
When making a diagnosis, a doctor may use the term cerebrasthenia or cerebrasthenic syndrome. These conditions have almost the same causes and symptoms; both are not a disease as such, but its long-term consequence.
The term syndrome is more often used when the etiology and pathogenesis are unclear. After clarifying the etiology, the word syndrome is not always replaced by the word cerebrovascular disease; both terms can exist in the name of the pathology as equivalent.
A syndromic diagnosis is usually made with a smaller volume of diagnostic tests, but it is sufficient to prescribe treatment.
Symptoms of cerebrasthenic syndrome in adults
A constant feeling of fatigue with impaired performance and weakness appears after strokes, heart attacks, and cerebral infections.
Cognitive impairment in CSA:
- Memory loss;
- Concentration disorders;
- Reading difficulties.
Lack of strength in adults can be seen around lunchtime. Even without physical activity, a person wants to rest, fatigue and weakness appear. The symptoms include excessive sweating, signs of VSD, insomnia, headaches, and fluctuations in blood pressure.
Most types of traumatic brain injuries do not go away without leaving a trace. In adults, vascular collaterals actively develop, so small intracerebral bleeding is partially compensated by the distribution of blood. In children, the arteries are poorly developed. Any external influence leads to the death of part of the parenchyma. The activity of recovery depends on the size of the hypoxic zone.
Common symptoms of cerebrastia in adults:
- Nausea;
- Poor tolerance to weather changes;
- Frequent dizziness and headaches;
- Emotional lability.
Individual symptoms are determined by secondary diseases. Diabetes mellitus and metabolic disorders (atherosclerosis, gout, antiphospholipid syndrome) disrupt cerebral microcirculation.
Treatment
Treatment of cerebrasthenic syndrome is carried out with medication. There is no fundamental difference in the restoration of functional brain activity in children and adults. Only the drugs, names and dosages are different.
What means are used:
- Nootropic. Accelerate metabolic processes in nerve tissues. Finibut, Phezam, Glycine and others. Used with caution; it may cause allergies in young patients.
- Cerebrovascular medications. Accelerates cerebral blood flow. Piracetam, Actovegin. They form the basis of therapy in most cases; treatment is required in courses.
- Mild sedatives. Based on herbal ingredients as an option. Valerian, motherwort in tablets (not in tinctures, because alcohol forms provoke stimulation of the nervous system). If ineffective, a short situational use of tranquilizers is possible. The question of which ones is addressed to the doctor.
- Sleeping pills as needed. Not prescribed for children.
- Vitamin and mineral complexes. To maintain cerebral structures in a normal state, inhibit or prevent destruction.
Proper nutrition with a sufficient amount of plant foods and protein, lean poultry (chicken, turkey) is especially important. The diet should be tailored to the load.
It is recommended to avoid stress and have enough walks in the fresh air per day. The rule is true for children and adults.
Patients with atherosclerosis are prescribed statins as medications to remove excess cholesterol and restore blood circulation in the brain. If the cause is narrowing of the arteries, it is necessary to stop smoking and drinking alcohol.
In situations that cannot be corrected conservatively, surgical treatment is possible, at the discretion of the doctor.
Prognosis and complications
In most cases, the prognosis for cerebrastia is favorable, especially in childhood; after adequate therapy and spa treatment, its symptoms practically disappear.
However, this neurological disorder in children predisposes to a decrease in school performance, the formation of negative character traits, and neuroses; such children are more easily susceptible to negative influence, and more often imitate antisocial behavior.
If a gentle regimen is not observed and there are unfavorable situational influences, the syndrome can develop into a more severe personality pathology.
Prevention – is it possible?
In order to minimize the risk of developing cerebrastia in young children, the expectant mother needs to promptly treat chronic diseases before and during pregnancy, correct endocrine, vascular and other pathologies of pregnancy, promptly seek qualified help if there are signs of toxicosis, Rh conflict, threat of miscarriage, hypoxia.
Careful diagnosis and correction of neurological disorders, prevention of childhood injuries, timely and competent treatment of infectious diseases and intoxications will help to avoid nervous exhaustion.
Symptoms of the disorder
With the asthenohyperdynamic variant of cerebrasthenia, fussiness, motor disinhibition and activity, restlessness, nervous excitability, aggression, and irritability predominate.
In the asthenoadynamic variant, lethargy, apathy, drowsiness, lethargy, and inactivity predominate.
General symptoms of cerebrospinal gravis:
- emotional instability, sudden mood swings, increased vulnerability and susceptibility to external influences, tearfulness, touchiness;
- increased fatigue and exhaustion of the nervous system;
- deterioration of memory and concentration;
- sleep disorders – insomnia or constant drowsiness;
- headaches, often accompanied by nausea, vomiting, increasing with fatigue and sudden movements;
- dizziness, fainting with darkening of the eyes and a feeling of severe physical weakness;
- poor tolerance to travel in transport, heat and stuffiness;
- sweating, lack of thermoregulation, fluctuations in body temperature, tachycardia;
- increased sensitivity to auditory, light and olfactory stimuli;
- long-term decrease in performance under intellectual load.
Symptoms of the syndrome in young children:
- motor restlessness;
- causeless crying, screaming;
- interrupted sleep;
- delayed formation of motor functions and speech development.
Symptoms in children of preschool and school age:
- in the motor sphere, two opposite options are possible: motor disinhibition or vice versa, lethargy and inertia;
- difficulties adapting to school;
- long-term persistence of speech defects;
- difficulties in developing reading, writing, and counting skills;
- poor memorization of educational material;
- intolerance to riding on carousels or swings;
- frequent causeless changes in mood, moodiness, dissatisfaction, melancholy.