Information about other types of diseases starting with the letter “V”: Vegetative state, Ventricularity, Vestibular ataxia, Vestibular neuronitis, Vibration disease, Viral meningitis, Viral encephalitis, Temporal lobe epilepsy, Intracerebral hematoma, Intracranial tumors of the cerebral hemispheres, Intracranial hypertension, Inflammatory myopathy, Inflammatory polyneuropathy , Congenital myopathy, Congenital paramyotonia, Secondary parkinsonism
In the medical community, the syndrome of increased intracranial pressure is called intracranial hypertension or hypertension. This disease develops against the background of damage to the brain tissue or appears autonomously, due to factors independent of the body.
Hypertension is a polysyndromic disease, and its manifestations are diverse: severe headaches with a feeling of pressure on the eyes, sometimes with temporary distortion of visual fields, a feeling of lightheadedness and vomiting. When blood pressure rises to high levels, loss of consciousness is possible.
The diagnosis is based on clinical manifestations, head tomography data, and echoEG results. An analysis of spinal fluid and ultrasound of brain vessels may also be necessary. Due to the large number of syndromes, treatment consists of eliminating or alleviating them. Neurosurgical operations are indicated in special circumstances.
Types of disease
Intracranial hypertension (ICP) is a disease that often occurs not only in adults, but also in children. The measure of intracranial pressure corresponds to the height of pressure in the spinal cord fluid, which is why this disease is also called cerebrospinal fluid hypertension syndrome. After head injuries or during brain diseases, hypertension is of a secondary nature. In a larger number of patients, hypertension is primary and manifests itself without visible motives - idiopathic hypertension, which is defined according to the ICD-10 classifier as benign. This diagnosis is established by a differential method of eliminating all possible causes of increased pressure inside the head.
ICP is divided into acute and chronic. The acute form occurs against the background of traumatic brain injury or infection, the chronic form occurs when vascular problems or intracerebral formations (tumors, cysts) occur. Chronic hypertension can be a side effect after brain surgery or after strokes, infections, or injuries.
Increased intracranial pressure: how to recognize and reduce?
Increased intracranial pressure - what does this concept really mean? How does intracranial pressure relate to arterial pressure?
We looked for answers to these and other questions with Yulia Vladimirovna Roshchupkina, a neurologist at the Expert Tula Clinic.
— Yulia Vladimirovna, what is intracranial pressure? What should it be normally and when it comes to increasing it?
This is a parameter that reflects the strength of the influence of cerebrospinal fluid (CSF) on brain tissue. The cerebrospinal fluid is under a certain pressure, which is called intracranial. Today it is measured in millimeters of mercury (mmHg) and is normally between 10 and 15 mmHg.
INTRACRANIAL PRESSURE IS MEASURED IN MILLIMETERS OF MERCURY (MM.Hg) AND IS NORMALLY FROM 10 TO 15 MM. RT. ST.
The danger is represented by pressure above 25 mmHg.
When it approaches 35 mmHg. it is designated as critical, loss of consciousness and death of brain cells are possible.
— Is increased intracranial pressure a diagnosis or a symptom?
This is a syndrome. Its synonym is intracranial hypertension. It occurs with a number of pathologies, as well as tilting the head, sneezing, physical activity, etc.
— By what signs can you understand that a person has increased intracranial pressure?
Symptoms of intracranial hypertension include a pressing, bursting headache, mainly in the morning. May be in different parts of the head.
Read the material on the topic: What to do if the head is “cast iron”?
Nausea and vomiting are also noted; drowsiness; disorders of memory, attention, thinking; autonomic disorders (fluctuations in blood pressure, decreased heart rate, increased sweating); blurred vision and blindness.
— What happens with increased intracranial pressure - do the vessels narrow or, on the contrary, expand?
Its increase is caused by dilation of the arteries leading to the brain, which is accompanied by an increase in blood flow to it, as well as a decrease in outflow through the veins. As a result, blood vessels overflow, and the surrounding tissue is saturated with blood plasma.
SYMPTOMS OF INTRACRANIAL HYPERTENSION INCLUDE PRESSING, BURNING PAIN, MAINLY IN THE MORNING. MAY BE IN DIFFERENT PARTS OF THE HEAD
In addition, this is also possible when a space-occupying formation or process develops in the cranial cavity.
— Increased intracranial pressure occurs only with high blood pressure or can it also occur with hypotension?
It is also possible with hypotension (one example is brain injury with concomitant significant blood loss).
Read the material on the topic: When there is nowhere lower. What are the reasons for hypotension?
On the question of the relationship between increased arterial and intracranial pressure: if the regulatory mechanisms work normally, then arterial hypertension does not necessarily lead to intracranial hypertension.
— What is the danger of high intracranial pressure?
As it increases, daily morning vomiting is possible against the background of intense headache. Mental functions are depressed. Lethargy appears, there may be disturbances of consciousness, even coma.
Blood pressure rises, breathing becomes depressed and becomes less frequent, and the pulse slows down. Generalized seizures may occur. In advanced cases, displacement and infringement of brain structures is possible, disrupting the functioning of vital centers of respiration and circulation, which leads to death.
— Tell us what leads to the occurrence of intracranial hypertension.
These are infections of the brain and its membranes; traumatic brain injury; neoplasms of various nature in the cranial cavity; hematomas, brain abscesses; prolonged lack of oxygen; difficulty in outflow through the jugular veins; dropsy of the brain; overweight, obesity, metabolic pathology; chemical poisoning.
Read the material on the topic: Will an MRI show meningitis?
— Are the reasons why intracranial pressure increases in children and adults the same or different?
In some ways they are similar. At the same time, in children, in particular, prolonged intrauterine oxygen deficiency, neuroinfections, and other pathologies of pregnancy and childbirth can lead to its increase.
— How is the cause of increased intracranial pressure diagnosed?
Mostly MRI and CT, ultrasound of the brain, echoencephaloscopy, and fundus examination are performed.
Read the material on the topic: What will the fundus tell you?
Intracranial pressure is measured using a pressure gauge. In this case, a special catheter is inserted into the spinal canal or into the ventricles of the brain.
You can sign up for a brain MRI in your city here
— Yulia Vladimirovna, does the condition of intracranial hypertension require mandatory treatment or can increased intracranial pressure go away on its own?
It depends on its cause. The solution to this issue is within the competence of the attending physician; self-medication is unacceptable. If any of the above complaints occur, contact your doctor for timely treatment.
— Are traditional methods used to reduce increased intracranial pressure? How effective are they?
And here everything depends on the cause and mechanism of development of this pathology. Folk remedies are not able to eliminate the cause; they are never used as primary means. However, theoretically, in some cases they can slightly alleviate the patient’s condition. In any case, the decision about the possibility of taking this or that drug is made by the doctor.
— What specialty should you consult with a doctor if you suspect intracranial hypertension?
To a neurologist. After clarifying the cause, consultation and, if necessary, treatment by a neurosurgeon may be necessary.
You can make an appointment with a neurologist in your city here
Attention: the service is not available in all cities
You may also find useful:
It's off scale! Looking for reasons for high blood pressure
What is hidden behind the diagnosis of migraine?
Vegetative-vascular dystonia: diagnosis or fiction?
For reference:
Roshchupkina Yulia Vladimirovna
In 2001 she graduated from the Faculty of Medicine of Kursk State Medical University.
From 2001 to 2002 she completed an internship in the specialty “Neurology”.
She specializes in acupuncture.
Currently he holds the position of neurologist at Clinic Expert Tula. Receives at the address: st. Boldina, 74.
Etiology and pathogenesis of intracranial hypertension
The sources of the disease are divided into groups:
The first is brain formations - primary or metastatic tumors, cysts, cerebral aneurysms, hematomas.- The second progresses against the background of a head injury, oxygen deficiency, ischemic stroke, toxic effects, encephalitis, edema of the brain or its membranes.
A separate group includes vascular causes that cause increased filling of the brain vessels with blood. This is possible when the temperature rises, when there is an excess of carbon dioxide in the blood, or when venous circulation is impaired.
Liquorodynamic disorders were identified as a separate category of causes of cerebral hypertension. It is caused by an increase in the production of cerebrospinal fluid. In this case, the volume of cerebrospinal fluid becomes excessive and leads to hydrocephalus.
Benign ICP occurs for unclear reasons. It develops more often in women than in men due to weight gain. This pattern gave rise to the hypothesis of an endocrine cause of the disease. Hypertension is caused by excessive intake of vitamin A, taking certain medications, and withdrawal of corticosteroid hormones after long-term use.
The skull is a confined cavity, so growing parts of the brain causes increased pressure. The result of this is compression of the brain of varying degrees. This condition leads to dysmetabolic changes in brain neurons. The more pressure increases, the more significant the shifting of brain structures, which can lead to wedging of the cerebellar tonsils into the foramen magnum. The cardiovascular and respiratory nerve centers are located in the brain stem, and when compression of these areas occurs, the vital functions of the body are disrupted.
The occurrence and development of the disease in children is facilitated by malformations of the brain (hydrocephalus, microcephaly, defects in the development of arteries and veins of the brain), birth injuries to the head, intrauterine infections, asphyxia and hypoxia of newborns. Due to the mobility of cranial sutures and their elasticity in infancy, the manifestations of high ICP contribute to long-term compensation.
Three variants of cerebral herniation syndrome
- Under the falx GM with displacement of the cingulate gyrus under its lower edge. It occurs more often than other types, but symptoms in almost all cases cannot be identified;
- Transtentorially with displacement of the inner part of the temporal lobe (often the uncus of the parahippocampal gyrus) into the depression formed by the tentorium of the cerebellum, where the midbrain (MB) is located. In this case, the oculomotor nerve and the SC itself are compressed, less often the posterior cerebral artery (PCA) and the upper parts of the brain stem;
- In the area of the cerebellum, which leads to a displacement of its tonsils into the space of the foramen magnum.
Clinical signs of pathology
The main symptom of the disease is headache. A growing, intense headache is a sign of an acute attack of hypertension. Intermittent headaches are a sign of a chronic form of the disease. The pain is symmetrical, with a feeling of pressure on the eyes, localized in the frontal and parietal parts of the head.
Patients report nausea, vomiting, pain when moving their eyes, and a feeling of fullness in the head. An acute, growing headache leads to loss of consciousness, and in severe cases to coma. Long-term hypertension worsens the general nervous condition of the patient, causing physical fatigue, nervousness, sleep disturbances, and mental instability.
Chronic intracranial hypertension lasts with crises - periods of sudden surges in pressure with severe headaches, nausea, vomiting, and fainting. Most often, patients experience darkening of the eyes, deterioration of sharpness, or double vision. 30% of patients note a decrease in vision clarity.
Intracranial hypertension in children under one year of age is accompanied by refusal of mother's milk, crying and restlessness, frequent regurgitation, and tension of the fontanel. Chronic hypertension in an infant can cause mental retardation, even mental retardation.
Causes of the disease
The increase in pressure is caused by an increase in the production of intracerebral fluid, or a violation of its release into the bloodstream. The accumulating volume begins to affect the parts of the brain being washed.
If a tumor occurs, the new formation begins to put pressure on the brain tissue. On the other hand, they are affected by cerebrospinal fluid. As a result, the brain begins to resist - hypertension appears.
Indirect sources are considered:
- Congestive heart failure;
- Obstructive pulmonary diseases;
- Impaired blood flow through the internal jugular vein;
- Pericardial effusion.
Reasons for the development of pathology in children:
- Congenital defects;
- Problems during childbirth;
- Prolonged hypoxia;
- Prematurity;
- Infections affecting the nervous system.
Establishing diagnosis
Only a neurologist, after thorough examinations, can make a diagnosis of high intracranial pressure. The main difficulty is that there is no generally accepted standard for ICP indicators. The experience of many years of research allows us to conclude that pressure values from 70 to 220 mm of water can be considered normal. pillar
Papilledema detected by an ophthalmologist may be a sign of ICP. X-rays of his skull show areas of thinning of his bones. A successful diagnostic method was lumbar puncture. When a needle is inserted into the cerebrospinal fluid space, cerebrospinal fluid flows out in strong jerks.
The use of electronic sensors requires craniotomy and therefore becomes an extremely undesirable way to make a diagnosis. This method is useful in severe cases of ICP to monitor pressure dynamics in the brain. Among the instrumental methods, MRI and CT of the head, ultrasound of the vessels of the head, biopsy of intracranial tumors are most often used; in children, neurosonography is performed through the fontanel.
Symptoms of the disease
Symptoms depend on the individual characteristics of the body and the amount of cerebrospinal fluid.
- The first sign is a feeling of heaviness, frequent headaches observed at night or in the morning. This is explained by an increase in the secretion of cerebrospinal fluid when a person is in a horizontal position, and a decrease in reabsorption.
- The maximum pressure observed in the morning provokes nausea on an empty stomach. After the release of vomit, the patient's condition does not improve.
- Long-term exposure to an irritating factor leads to nervousness, irritability and fatigue.
- There are complaints of vegetative-vascular disorders: increased heart rate, sharp jumps in blood pressure, frequent fainting states, sweating.
- Noticeable “bruises” under the eyes against the background of good sleep and a normal rhythm of life. The effect is provoked by the expansion of the venous network of the lower eyelid and infraorbital region.
- There is a clear dependence of exacerbations and remissions on weather conditions.
- Sometimes the clinical manifestation is considered to be a lack of libido.
Treatment methods
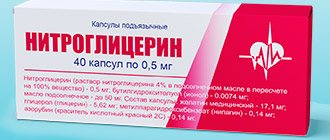
Regular use of medications is necessary for the chronic course of the disease or during crises in the absence of deep disorders of consciousness. Depending on the level of ICP, one or another diuretic pharmaceutical is prescribed. In mild cases - furosemide, hydrochlorothiazide, spironolactone, in acute form - mannitol. Taking diuretics should be combined with potassium preparations - potassium chloride, potassium aspartate.
In the presence of concomitant infectious diseases, antiviral and antibacterial drugs are prescribed. When the body is intoxicated, detoxification measures are carried out. For venous circulation - venotonics. In conditions of ICP, nerve cells need special nutrition; for this purpose, piracetam, gamma-aminobutyric acid, and glycine are prescribed. It is advisable to undergo courses of cranio-manual therapy, which improves the outflow of venous blood. During crises, excessive strain on the eyes and emotional overload should be avoided.
Neurosurgical surgical interventions can be performed urgently or plannedly in severe forms of the disease. In acute prolonged crises, external ventricular drainage or craniotomy is indicated to reduce intracranial pressure. Removal of brain tumors, elimination of hydrocephalus, and cerebral shunting are routinely performed.
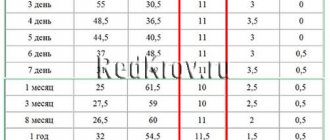
Stepped therapy to reduce ICP
Typically, treatment to reduce elevated ICP is gradual. It is assumed that the patient is already undergoing basic measures aimed at reducing ICP: artificial ventilation, sedative therapy, body temperature, electrolyte composition and blood gases are normalized.
Any disruption of the patient’s synchronization with the ventilator, coughing during sputum suction, is accompanied by an abrupt increase in ICP. To avoid these issues, muscle relaxants and/or deep sedation should be used. Rarely, the patient can remain spontaneously breathing. The next stage of action is started if the previous actions are ineffective.
Hyperosmolar therapy
Traditionally, mannitol or hypertonic solutions (3-20%) sodium chloride (HS) are used. In some cases, doctors may want to consider giving these drugs alternately. Mannitol, given its diuretic effect, is preferable in patients with normo- or hypervolemia. It is believed that a dose of mannitol less than 0.5 g/kg has little effect on intracranial pressure, and a dose of more than 2 g/kg increases the likelihood of kidney damage. In case of hypovolemia, hyponatremia, hypotension, a hypertonic sodium chloride solution is recommended for the patient.
In most cases, hypertonic sodium chloride solutions were more effective than mannitol in reducing ICP. Firstly, the effect of reducing ICP lasts for 4-8 hours after the administration of sodium chloride, versus 2-5 hours when using mannitol. Second, the blood-brain barrier is less permeable to sodium chloride (reflectance 1.0) compared to mannitol (reflectance 0.9). Therefore, when using sodium chloride, the rebound phenomenon does not appear; the “working range” is significantly expanded - up to an osmolarity of 350 mOsm/l.
Mannitol (Mannitol) is administered over 15-20 minutes at the rate of 1 g/kg body weight. After this - 3-4 times a day at the rate of 0.25-0.5 g per 1 kg of the patient’s body. Sodium chloride 7.5% is prescribed at the rate of 3-4 ml/kg (in 20-30 minutes), then 1-1.5 ml/kg 3 times a day. When blood osmolarity is more than 320 mOsm/L, mannitol is not recommended. When using hypertonic solutions (3-7.5%) sodium chloride, blood osmolarity should not be higher than 340 mOsm/L.
If it is not possible to control ICP, the administration of osmotically active drugs should be limited, in most cases, to one to two days. The blood sodium level during this period of treatment should be maintained within the upper limit of normal - 144-155 mmol/l.
Hyperventilation
The use of mechanical ventilation in hyperventilation mode (PaCO2 <30-32 mm Hg) makes it possible for some patients to reduce the degree of ICH for 1-2 hours, and thereby gain time for other methods of combating ICH.
Sodium thiopental
Sodium thiopental is prescribed if there is no effect from the above treatment. In case of hypotension and hypovolemia in humans, this method is contraindicated. The first (loading dose) of sodium thiopental is 10-15 mg/kg (administered over 30 minutes). In the next 3 hours, if the patient's hemodynamics allow, continue administration of sodium thiopental at a rate of 3-6 mg/kg/hour. And then - throughout the day, 2-4 mg/kg/hour.
Use of cerebrospinal fluid drainage
Liqueur drainage through a ventricular catheter is prescribed for hydrocephalus, but it is not always feasible and increases the risk of purulent complications.
Moderate hypothermia
Moderate hypothermia (33-34°C), performed for 1-2 days, is quite effective in reducing ICH.
Decompressive craniotomy
This is an effective but difficult intervention to reduce treatment-resistant ICH.
Prevention and prognosis
The outcome of liquor-hypertensive syndrome depends on the underlying disease, pressure level and adequate surgical therapy. In severe cases, the patient's death is possible. ICP of unknown origin responds well to therapy. If a child remains in this state for a long time, the most severe complication may be mental retardation.
Preventive measures that prevent the development of intracranial hypertension include: current diagnosis and treatment of intracranial neoplasms, dyscirculatory disorders, regular use of blood pressure-normalizing drugs in the chronic course of the disease, adherence to a daily routine, proper management of pregnancy and obstetric care.
Benign form of pathology
Benign intracranial hypertension is a separate form of the disease that occurs with the mildest manifestations, without symptoms of damage to the nervous system. It is also called idiopathic or false brain tumor. Women who are young and obese most often suffer from the pathology. The main symptoms are the urge to vomit, unsteadiness of gait, pain in the head and eyes. Why such a syndrome is formed is still not completely clear to doctors.
Initially, headaches are mild, which is why people do not seek medical help, especially since attacks are quickly eliminated after taking analgesic tablets. Then the problem becomes constant, accompanied by nausea and vomiting. Vision problems appear, in women the regularity of the menstrual cycle is disrupted, in men - weakening libido.
As a rule, there are no signs of damage to the nervous system, and in the initial stages the disease goes away on its own without treatment. Doctors have identified a connection between the development of symptoms in women and the use of oral contraceptives, after which the pathology disappears without a trace. If the clinical picture is pronounced, the same drugs are used in conservative treatment as in the treatment of the usual form of intracranial hypertension.
Features of treatment of ICH in certain conditions
Corticosteroids are quite effective in reducing the degree of ICH if it is caused by a tumor process. The drug of choice is dexamethasone. It is prescribed intravenously at 4-12 mg three times a day. For ICH caused by other causes, the effectiveness of corticosteroids has not been proven.
If ICH is caused by hydrocephalus (occlusion of the cerebrospinal fluid ducts due to SAH, meningitis, brain tumors, etc.), in addition to the main therapy, furosemide 1 mg/kg or acetazolamide (Diacarb) 10-20 mg/kg per day is prescribed (the dose is divided into 3 doses ). Both drugs reduce the production of cerebrospinal fluid, which helps reduce ICP.
Dihydroergotamine, a selective venous vasoconstrictor, may be effective in people with severe cerebral congestion (brain swelling) and refractory ICH. 250-500 mcg of the drug is administered intravenously, if necessary, repeat after 1 hour, maximum dose 2 mg per day.
If symptoms of brainstem dislocation develop quickly (in minutes), you can try using hypertonic sodium chloride solution in higher doses. A quick infusion (about 10-20 minutes) of 7.5% sodium chloride solution is performed at a rate of 3-4 ml/kg. At the same time, of course, resuscitation measures continue - sedation, mechanical ventilation in hyperventilation mode, administration of vasopressors, etc.