Subendocardial ischemia is considered one of the most common cardiac causes of sudden death among men and women over 45 years of age. A distinctive feature of the disease is the slow progression of irreversible changes in the myocardial tissue, the occurrence of systemic disturbances in the functioning of this area of the heart muscle. Subendocardial ischemia is determined using ECG, isotope diagnostics of the heart, echocardiography after stress loads on the patient’s cardiovascular system.
Definition of subendocardial ischemia
Subendocardial ischemia is a pathological condition of the myocardium that occurs due to disturbances in the circulatory supply of its tissues. The coronary vessels run along the entire area of the epicardial surface of the heart muscle, and then penetrate deep into the myocardium.
The main arteries sequentially connect the epicardial, middle, and subendocardial segments of the heart to the general blood flow system. The last section of the heart muscle is the most distant from the coronary vessels. The subendocardial layer experiences maximum tension during the contractile activity of the heart and needs more oxygen.
Development mechanism
The subendocardial region of the heart muscle is most susceptible to the development of coronary disease. This is due to the fact that the left wall of the ventricle is characterized by greater tissue thickness. Impaired blood supply to the myocardium leads to the occurrence of degenerative processes in its subendocardial layer. At the same time, the wall of the right ventricle is thinner and is much easier and faster irrigated with blood coming from the coronary arteries.
The subendocardial segment of the myocardium is considered a weak and vulnerable area of the human cardiovascular system, which is susceptible to the development of coronary artery disease due to circulatory disorders. The severity of the pathology depends on the severity of the deficiency of oxygen and other nutrients that enter the myocardium along with the blood.
Causes
The main cause of the development of subendocardial ischemia is atherosclerotic changes in the internal structure of the coronary vessels. One of the arteries that supplies blood to the myocardium narrows in the lumen or becomes clogged with plaques. A lack of blood supply negatively affects the functional state of the heart muscle, but the subendocardial region, which requires a larger volume of blood and oxygen, is primarily affected.
The following predisposing factors that cause subendocardial ischemia are identified:
- maintaining a sedentary lifestyle, when minimal physical stress is created on the heart muscle tissue;
- diabetes;
- hypertension, accompanied by stable maintenance of blood pressure, the levels of which are higher than 140 by 90 units;
- hereditary predisposition to coronary disease and myocardial infarction (for example, if one of the person’s parents previously died from this disease before the age of 55);
- overweight with progressive obesity;
- smoking;
- chronic alcoholism.
Subendocardial ischemia is a dangerous condition of the heart myocardium that can be diagnosed using a stress ECG. Prevention and effective therapy of this disease are impossible without eliminating the above risk factors.
ST segment elevation in ischemic heart disease
ST segment elevation is associated with transmural or subepicardial ischemia.
Look at Chart 4, which shows two typical types of ST elevation: concave and convex. IHD is characterized by convex elevation.
Diagram 4. Concave and convex ST elevation
Schema source.
In coronary artery disease, ST segment elevation can occur with a heart attack with ST elevation, with Prinzmetal's angina, as well as with post-infarction ventricular aneurysm.
ECG 4 shows an example of ST elevation in leads I, aVL, V2-V6, indicating myocardial infarction in the region of the anterior and lateral walls of the left ventricle. In addition to elevation, the cardiogram shows ST depression in the inferior leads (III, aVF). These are reciprocal (i.e., mirror) changes, reflecting the same process as ST elevation in I, aVL, V2-V6, but in leads located on the other side of the infarction area. In general, if the cardiogram shows ST depression, characteristic of ischemia, in a large number of leads, then this indicates subendocardial ischemia. And if such depression is recorded in a limited number of leads, as in ECG 4, then these are, as a rule, reciprocal changes associated with ST elevation infarction.
In addition, ECG 4 recorded pathological Q waves (in this case, QS complexes) in leads V2-V4. Pathological Q is a sign of necrosis.
ECG 4. Increased ST segment during myocardial infarction
ECG source.
Symptoms
The first signs of subendocardial ischemia are easily confused with most other cardiac disorders.
This myocardial pathology is manifested by the following symptoms:
- compressive pain in the chest, the intensity of which varies from minor discomfort to severe burning;
- a feeling of prolonged pressure on the surface of the chest;
- a feeling of lack of air, the appearance of which is paroxysmal in nature;
- girdling pain syndrome, which covers the area of the body from the left shoulder blade to the upper part of the abdominal cavity, where the solar plexus is concentrated.
The most atypical symptom of subendocardial ischemia is pain, which is localized in the lower jaw. In this case, a person may experience severe discomfort in the muscles of the left arm, general physical fatigue, and decreased performance. The most dangerous manifestation of subendocardial ischemia is the sudden onset of myocardial infarction. For example, if the patient previously ignored the symptoms of this pathology, did not undergo diagnostics, and did not treat it.
Clinical case
A 74-year-old obese woman was admitted to our department with repeated episodes of chest pain over the past few days.
The photo below shows the ECG result recorded after the exercise. While recording the tape, the patient began to complain of chest discomfort. After the administration of Nitroglycerin, the patient felt better, and an ECG was re-recorded.
Coronary angiography performed on the patient showed severe stenosis of the right coronary artery.
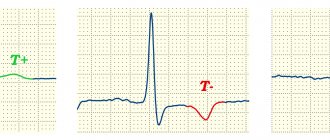
Manifestations on the cardiogram
Subepicardial ischemia on the ECG will be visible as negative, symmetrical and peak T-waves in leads that correspond to the location of the affected area of the myocardium. T-waves can be dynamic, appearing only during pain, and also regress on their own or after the administration of Nitroglycerin.
Diagnostics
Subendocardial ischemia on the ECG is manifested by ST segment depression. Signs of a painful state of the myocardium are determined after decoding the results of the electrocardiogram.
Preparing for the examination
An ECG is an informative method of hardware diagnostics that displays the functional state of the heart muscle.
To obtain the most objective data before the examination, the following preparation rules must be observed:
- during the day before the diagnosis, exclude any physical activity and psycho-emotional stress;
- you need to get enough sleep before going to the hospital;
- on the day of the ECG it is not recommended to overeat or consume too much fatty food;
- Do not apply oil-based cosmetics to the surface of the skin of the chest or use a variety of lotions and creams;
- The last cigarette should be smoked no later than 30-40 minutes. before the examination (otherwise the nicotine contained in tobacco products may provoke spasm of blood vessels, which will be reflected in the ECG results).
Before a heart diagnosis, you should not do any physical exercise. You should arrive at the hospital 10-15 minutes in advance. before the scheduled examination time. The cardiovascular system should not experience any critical stress.
Carrying out an ECG
Subendocardial ischemia on an ECG is diagnosed by a cardiologist, who records any changes in the rhythmic activity of the patient’s heart. Performing an electrocardiogram when the patient is at physical rest does not determine the severity of coronary artery disease.
In this case, the ECG method is used in combination with the following types of stress loads:
- quick work on an exercise bike, after which the patient immediately lies down on the couch to take an electrocardiogram;
- administration of drugs that stimulate the functional activity of the heart muscle (for example, Dobutamine);
- isotope study of the heart muscle with simultaneous creation of physical activity.
As additional stress on the cardiovascular system, the patient may be asked to perform squats, push-ups, and quickly walk around the perimeter of the room.
The electrocardiogram itself is performed as follows:
- After creating physical stress on the cardiovascular system, the patient lies with his back on the surface of the couch.
- The patient's torso and legs are freed from clothing.
- The cardiologist attaches special electrical sensors to the patient's chest, wrists and ankle area that record the rhythmic activity of the heart and blood vessels.
- The electrocardiograph is launched, which collects information about the performance of the patient’s cardiovascular system.
The average duration of the diagnostic procedure is from 10 to 15 minutes. Depending on the general condition of the patient, during one examination, a cardiologist may conduct an ECG before and after physical activity. The received data is recorded in electronic and paper versions. Based on the results of deciphering the ECG, the cardiologist decides to refer the patient to undergo an additional diagnostic method in the form of coronary angiography.
Interpretation of the results, signs of subendocardial ischemia on the ECG
Subendocardial ischemia on the ECG is manifested by changes in the functioning of the heart and arterial vessels. When interpreting the examination results, special attention is paid to the ST segment and T wave, the indicators of which are displayed in the form of wavy lines. Using the electrocardiogram method with physical activity, it is possible to determine the initial stages of subendocardial-type coronary artery disease, as well as more advanced forms of the disease.
The table below details the procedure for interpreting ECG results to confirm or refute subendocardial ischemia.
| Diagnostic indicators | Decoding electrocardiogram data |
| ST segment | Subendocardial ischemia is determined by the characteristic presence of ST segment depression. This indicator indicates a severe disturbance of blood flow in the myocardial tissue. In this case, it is the subendocardial portion of the heart muscle that is in the affected area. If, during interpretation of the ECG results, it was determined that the ST segment is in a state of elevation, then this patient has pathological signs of subepicardial or transmural myocardial ischemia. |
| T wave | On the results of the electrocardiogram, the T wave shows physiological changes in the tissues of the myocardium of the heart. These fluctuations are especially clearly visible in the presence of coronary circulatory disorders. The severity of coronary artery disease is determined by the nature of changes in the shape of the T wave. For example, if the shape of the T wave quickly takes on its previous appearance, this indicates that there are no necrotic changes in the myocardial tissue. In patients with signs of necrosis of the subendocardial area, the T wave retains an atypical shape for several months, and sometimes pathological changes in this indicator are diagnosed for years. |
If the presence of ST segment depression always indicates acquired subendocardial ischemia of myocardial tissue, then the T wave is an indicator of pathological changes in this part of the heart. A high-quality interpretation of the results of an ECG with physical activity can only be done by a practicing cardiologist with sufficient experience. Additional signs of subendocardial ischemia are blockades and arrhythmic disturbances in the heart.
ST segment changes
Normally, the ST segment is located on or near the isoline.
Estimates of ST tolerances vary slightly across studies. There may also be different approaches to measuring ST deviation.
The following ST segment displacements are considered pathological.
- Decrease (depression) in ST by 0.5 mm or more in V2-V3 and by 1 mm or more in other leads.
- Increase (elevation) of ST by 2 mm or more in V2-V3 and by 1 mm or more in other leads in men (in men under 40 years old, an increase in ST in V2-V3 to 2.5 mm is acceptable).
- by 1.5 mm or more in V2-V3 and by 1 mm or more in other leads in women
If in two or more than two adjacent leads the ST segment deviates from the isoline by more than the specified values, then this is a pathology.
ST deviation is usually measured at the J point (where the QRS complex enters the ST segment), as well as at ST60 (0.06 s from the J point) and ST80 (0.08 s from the J point).
When measuring the ST deviation at the J point, comparison is made with the level of the PR interval at the point of transition of the PR to the QRS complex. This is shown in diagram 1.
Diagram 1. J point and PR transition point
Schema source.
ECG 1 shows how ST segment displacement can be measured. In the example shown, an ST depression of 2 mm was recorded.
ECG 1. Fragment of a cardiogram with ST segment shift
Measuring the ST segment displacement not at point J, but at a distance of 0.08 s, i.e. 2 mm from the J point may be an alternative approach. This is especially true when there is an initial shift in the PR interval and ST segment due to the atrial repolarization wave.
The wave of atrial repolarization (indicated by Ta) is superimposed on the QRS complex and, as a rule, is not visible on the ECG. However, in some cases, the Ta wave becomes noticeable and displaces the PR interval, QRS and initial ST region.
Illustration of the phenomenon of atrial repolarization, which shifts the PR interval, QRS and initial ST segment in diagram 2. Here the Ta wave is shown in red dotted line.
Scheme 2. Atrial repolarization wave Ta
Schema source.
It is believed that the duration of the atrial repolarization wave does not exceed 0.08 s after the end of the QRS complex. In this regard, the ST displacement measurement is in some cases carried out at a distance of 0.08 s from the J point. The point at a distance of 0.08 s (2 mm) from the J point is called the I point or ST80. When displacement is assessed at ST80, comparison is made with the TP interval (between the T wave and the P wave) rather than with the PR interval.
ECG 2 shows an example when the atrial repolarization wave simulates ST segment depression. A cardiogram was taken from a 25-year-old patient with complaints of chest discomfort. The patient abuses caffeine. The recording showed tachycardia and ST depression in leads II, III, aVF and V2-V6. However, if you look closely, you can also see that the PR segment has an oblique, downward shape. This is due to the atrial repolarization Ta wave, which also shifts ST downward. If you measure the ST level at point ST80 (2 mm after the J point) and compare it with the level of the TP segment, then there will be no significant depression.
ECG 2. ST shift caused by a pronounced wave of atrial repolarization
ECG source.
However, in the case of ECG 2, even without this adjustment, there was no evidence of ischemia, because the shape of the ST segment is obliquely ascending. Ischemia is characterized by downward or horizontal ST depression. Morphological assessment of ST segment changes is more important than assessment of displacement using one or another technique.
A displacement of the ST segment above or below its normal position can occur in different types of coronary artery disease, as well as in other heart pathologies (for example, with blockade of the ventricular pathways, with ventricular hypertrophy, with tachycardia and in other cases).
Different authors and different guidelines suggest different ways to measure ST levels, but everyone agrees that assessing the morphological pattern allows a more accurate conclusion to be made. Therefore, in order to understand what causes ST deviation in each specific case, you need to know the morphological variants of ST displacement.
Treatment
The treatment regimen for subendocardial ischemia is selected individually depending on the diagnostic results and the general well-being of the patient. Taking medications should be accompanied by the prevention of pathological changes in the myocardium, as well as the elimination of the main causes that caused atherosclerosis of the coronary vessels.
Antiplatelet drugs
The action of antiplatelet medications is aimed at preventing blockage of the coronary arteries and restoring full blood supply to all areas of the myocardium.
Clopidex
Clopidex is a medicine in tablet form, which is produced by a Turkish pharmaceutical company. This medication has antithrombotic properties, prevents myocardial infarction and sudden death. Clopidex is taken in a dosage of 0.5 - 1 tablet once a day. The dosage regimen for this medication can be changed by the attending physician depending on changes in the functional state of the myocardium. The average cost of the drug Klopidex is from 345 to 476 rubles. for 30 tablets.
Sylt
Zilt is an antiplatelet agent that is produced by the domestic pharmaceutical company KRKA-RUS LLC. The release form of the drug is pink tablets. The drug Zilt is prescribed for the treatment and prevention of coronary disease, myocardial infarction, and circulatory pathologies in the coronary vessels.
The dosage regimen for this medication is determined individually by the doctor. To enhance the antiplatelet effect, drugs based on acetylsalicylic acid are used in combination with the drug Zilt. The average cost of this medication ranges from 501 to 526 rubles. for 28 tablets.
Cholesterol-lowering drugs (statins)
Low molecular density cholesterol-lowering drugs must be taken continuously for the rest of your life. Lipid-lowering medications prevent the formation of cholesterol plaques in the lumen of arterial vessels.
Atorvastatin
The drug Atorvastatin is available in the form of tablets with the active ingredient atorvastatin with a dosage of 10 mg. The manufacturer of this medicine is ZAO Biokom, Russian Federation. The initial dose of this drug is 1 tablet once a day. If necessary, the therapeutic dosage can be increased 8 times. Every 2 to 4 weeks, all patients taking this medication should have their blood tested for lipid levels. The average cost of the lipid-lowering drug Atorvastatin is from 135 to 184 rubles. for 30 tablets.
Rosuvastatin
The drug Rosuvastatin is a safe medication for lowering blood cholesterol levels. Lipid-lowering tablets are produced by Russian pharmaceutical companies. The active substance of this medication is rosuvastatin calcium in a dosage of 5 mg. The dosage regimen for this drug involves taking it in the amount of 1-2 tablets 1 time per day.
The average cost of the drug Rosuvastatin is from 156 to 294 rubles. for 30 tablets.
Calcium antagonists
Calcium antagonists are a separate group of drugs that slow down the flow of calcium ions into muscle cells. In the treatment of subendocardial ischemia, they are used as agents that normalize the rhythmic activity of the heart and improve blood circulation in the coronary vessels.
Diltiazem
Diltiazem is an effective drug based on the active substance diltiazem hydrochloride with a dosage of 90 mg per tablet. This medicine is produced by a Macedonian pharmaceutical company. This drug is taken in a dosage of 1 tablet 2-3 times a day. In case of therapeutic need, the indicated dose can be increased by 2 times. The average cost of the drug Diltiazem is from 91 to 122 rubles. for 30 tablets.
Nifedipine
Nifedipine is a potent drug for blocking calcium channels, which is produced by Valenta Pharmaceuticals PJSC. The active substance of this medication is the chemical compound nifedipine in a dosage of 10 mg. This drug is prescribed 1 tablet 3-4 times a day. The average cost of Nifedipine is 28 rubles. for 50 tablets.
Antianginal drugs from the nitrate group
Drugs from the group of nitrate-based antiangial agents are taken to quickly expand the lumen in the coronary vessels and provide the myocardium with additional oxygen.
Nitroglycerine
Nitroglycerin is a cardiac medicine that is produced by the Russian pharmaceutical company. 1 tablet of this drug contains 400 mcg of nitroglycerin.
This drug is used to prevent and relieve acute attacks of angina caused by coronary artery disease. Nitroglycerin is taken in a dosage of 1-2 tablets at the time of the appearance of shortness of breath, heart rhythm disturbances, and dizziness. The average cost of this medication is about 110 rubles. for 40 tablets.
Isacardine
Isacardin is a concentrate for self-preparing an injection solution. 1 ampoule of this medication contains 10 mg of the active substance isosorbide dinitrate. Isacardin is produced by the Russian company Ozon LLC. An infusion solution prepared from a concentrate is administered intravenously or injected into the oral cavity. The dosage regimen and duration of therapy are determined individually by the attending physician. The average cost of the drug Izacardin is from 697 to 749 rubles. for 10 ampoules with concentrate.
Lifestyle correction
Subendocardial ischemia on the ECG is manifested by focal changes in the densest myocardial tissue. As the disease progresses, large areas of the heart muscle die. Lifestyle correction is the main rule for effective prevention of coronary artery disease.
In this case, the following recommendations must be followed:
- stop drinking alcohol and smoking;
- to live an active lifestyle;
- do not travel by transport, but walk more, training all segments of the cardiovascular system;
- control cholesterol and blood sugar levels;
- regularly undergo scheduled examinations with a cardiologist;
- do not eat too fatty, fried, smoked foods, since the substances contained in their composition negatively affect the condition of the heart muscle and blood circulation in the coronary vessels;
- promptly treat concomitant diseases that contribute to the occurrence of coronary artery disease;
- avoid stress and psycho-emotional stress;
- provide the body with moderate physical activity.
Corrective changes in the lifestyle of a person with subendocardial ischemia should be agreed upon with a cardiologist. The doctor of this specialization independently determines what level of physical activity of the patient is optimal for the prevention of coronary artery disease.
Expert advice
It is known that subendocardial ischemia is difficult to diagnose and is not often recorded on the ECG, since it occurs in the early stages of a disturbance in the blood supply to the heart muscle and the patient does not yet present any complaints. Moreover, it is necessary to conduct additional examinations, since there are some pathologies with the same signs on the cardiogram:
- subepicardial ischemia of the posterior wall of the myocardium (right leads);
- hyperkalemia (blood potassium above 6 mEq/L) - T waves are sharp, the QT interval is shortened;
- alcoholism (signs of alcoholic cardiomyopathy may not yet appear);
- when the left ventricle is overloaded in diastole, for example with aortic regurgitation, tall T waves in the left leads often appear on the film;
- The normal variant for vagotonia is asymmetrical, high T.
Possible complications, prognosis
In the absence of effective prevention and treatment of subendocardial ischemia, the patient will die from myocardial infarction. The risk of a heart attack increases sharply during physical activity. Lifestyle correction and regular use of medications can help curb degenerative changes in myocardial tissue.
Subendocardial ischemia is a dangerous type of coronary artery disease that occurs due to atherosclerotic changes in large coronary vessels. The disease occurs in a chronic form with slow progression. The mechanism of development of the pathology is a disruption of the blood supply in the tissues of the subendocardial region of the myocardium.
This segment of the heart muscle requires the greatest amount of oxygen. A lack of blood supply leads to local tissue necrosis. Diagnosis of cardiac disease is carried out using an ECG with physical activity. Based on the results of the study, an adequate treatment regimen is selected.
What is important to remember
Treatment of ischemia should be carried out according to a standard regimen, regardless of in which part of the myocardium it occurred. Its goals are to eliminate causes, relieve symptoms, and prevent necrosis. In our practice, we use both medicinal and surgical methods of therapy.
We always focus on modifying the patient’s lifestyle: giving up bad habits, adjusting the diet, and aerobic exercise. It is the reduction of these risk factors that will help keep the artery walls elastic, strong, smooth and ensure adequate blood flow.