Find out more about other diseases starting with the letter “X”: Huntington’s chorea; Chronic inflammatory demyelinating polyneuropathy; Chronic cerebral ischemia.
Chronic cerebral ischemia is a failure of the cerebrovascular system that develops against the background of impaired blood circulation in the structures of the brain. Chronic cerebral ischemia is expressed by headaches, dizziness, emotional lability, disorders of cognitive and motor functions.
For diagnostic purposes, CT or MRI of the brain, ultrasound examination of cerebral vessels, and hemostasiogram examination are prescribed. Therapeutic efforts for chronic cerebral ischemia consist of the prescription of antihypertensive drugs, lipid-lowering, antiplatelet measures. In some cases, surgical treatment is provided.
Causes of chronic cerebral ischemia
- The main causes of chronic cerebral ischemia include arterial hypertension and atherosclerosis. Chronic cerebral ischemia caused by a combination of two conditions is common. In addition, among other reasons causing this disease, there will be symptoms of cardiovascular diseases, which are expressed in heart rhythm disturbances (for example, arrhythmia), which, in turn, leads to a decrease in systemic hemodynamics.
- Doctors attach great importance to the study of vascular anomalies, both in the brain and in the vessels of the cervical spine. Such anomalies, like those associated with the aorta or vessels of the shoulder girdle, often do not manifest themselves for a long time, until the development of atherosclerotic and hypertensive processes.
- In recent years, neurologists have identified a number of other reasons that contribute to the development of chronic cerebral ischemia, including venous pathology of an intracranial and extracranial nature. It is possible that the occurrence of chronic ischemia is influenced by compression of arterial and venous vessels. Doctors take into account both the spondylogenic effect and possible compression of blood vessels by muscles, an aneurysm or a tumor. Another possible cause of this pathology is developing cerebral amyloidosis.
Typically, identified encephalopathy manifests itself symptomatically mixed. If factors have been discovered that caused the development of chronic cerebral ischemia, then all other possible causes are considered additional causes. Of course, identifying and accurately identifying additional factors that aggravate the course of the disease will be very necessary, first of all, in order to make the right decision regarding symptomatic or etiopathogenetic treatment.
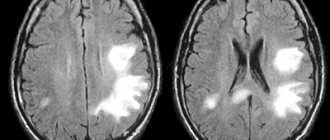
In medicine in recent years, the occurrence of chronic cerebral ischemia is usually considered in two ways: according to the nature and nature of the damage and according to the usual localization. In the case of bilateral diffuse damage to the brain, more precisely, its white matter, they speak of a leukoencephalopathic type of encephalopathy. The second option is the lacunar type, which has a large number of lacunar foci. If such two options are most often found in theory, then in practice they speak of their mixed type.
Most often, the lacunar variant is caused by a process such as occlusion of small vessels. A significant role in the pathogenesis of diffuse damage is assigned to a decrease in systemic hemodynamics or, as it is also called, arterial hypotension. The reason for the decrease in blood pressure will be improperly administered antihypertensive therapy, as well as a decrease in cardiac output. A significant role is played by severe cough and orthostatic hypotension, which often happens in the case of vegetative-vascular dystonia.
As is known, the main pathogenetic link of this disease is the depletion of the compensation mechanism, as well as a decrease in the energy work of the brain, which leads to the obvious development of functional disorders and such irreversible processes of a morphological nature as a slowdown in blood flow, a decrease in blood glucose levels, a decrease in oxygen levels, and the occurrence of capillary stasis, the appearance of slow cerebral blood flow, thrombus formation, the ability to depolarize cell membranes.
Classification of cerebrovascular pathology
CVD is a brain disease associated with progressive tissue damage due to impaired circulation in the organ. It can arise due to pathologies of cerebral vessels, which cause changes in the blood circulation of brain tissue and hypoxia. It is mainly diagnosed in older people, but in rare cases, the disease can also occur in a child.
Cerebrovascular disease develops gradually. At the very beginning, the brain begins to experience oxygen deficiency due to vascular dysfunction.
With chronic hypoxia, all brain functions begin to suffer. First, transient and then persistent changes in brain tissue occur.
Cerebrovascular disease contributes to the development of grade 2 DEP, which causes brain damage.
Based on the classification, CVD can be divided into transient, acute and chronic.
Acute cerebrovascular insufficiency includes:
- Encephalopathy of the hypertensive type.
- Ischemic attacks.
- Stroke (multilacunar form, ischemic, hemorrhagic, unspecified).
Chronic cerebrovascular insufficiency (CVI) is divided into:
- Embolism, which results in blockage of blood vessels by blood clots. Which arise in the large arteries of the body and can enter small ones with the blood.
- Bleeding resulting from rupture of the vascular walls. This condition provokes the development of hemorrhagic stroke.
- Thrombosis is a pathology when the lumen of blood vessels narrows and becomes clogged with plaques.
Neurologist Mikhail Moiseevich Shperling will tell you more about the ischemic form of stroke:
The transient form of cerebrovascular disease includes:
- Cerebral hypertensive crisis.
- Transient ischemic attacks.
Symptoms of chronic cerebral ischemia
The main symptomatic manifestations of chronic cerebral ischemia include:
- movement disorders of polymorphic type;
- decreased memory and mental abilities;
- changes in the patient's emotional background.
A feature of chronic cerebral ischemia is its progressive course. In addition, the disease is characterized by the presence of stages and syndromes. Doctors note the so-called inverse relationship between present complaints (especially those related to concentration and the ability to remember) and the degree of manifestation of this disease. The more the patient's cognitive functions are weakened, the fewer complaints he will have. As practice shows, the patient’s subjective complaints do not indicate the severity or nature of the disease process.
The main clinical manifestation of dyscirculatory encephalopathy today is considered to be cognitive impairment, which can be detected even at the first stage. Their nature, as a rule, is progressive, which is noticeable already at the third stage of the disease. In parallel with emotional disorders (such as emotional lability, inertia and all kinds of loss of interest), a variety of motor disorders can occur, including the inability to control and perform both simple reflex and complex automated movements).
Cerebrovascular disease - consequences
Severe cerebral damage is accompanied by an increase in irreversible processes in the brain, which is manifested by mental, neurological and cognitive disorders (the emergence of phobias, impaired coordination of movements, inability to concentrate, etc.). Sometimes involuntary movement of the eyeballs is possible.
The severe consequences of cerebrovascular disease include:
- ACVA is an acute cerebrovascular accident that is reversible. Neurological symptoms usually disappear within the first few days.
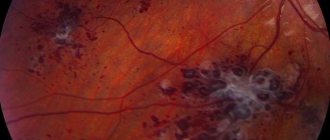
- Ischemic stroke – as a result of insufficient blood supply to certain areas of the brain, their tissues die. In this case, the patient experiences general cerebral and focal symptoms associated with the site of cell death. This may be paralysis, paresis, speech or vision impairment, memory loss, etc. Moreover, such changes can be both reversible and irreversible.
- Binswanger's disease. The pathology is associated with atrophic changes in the white matter. The disease has a progressive development. Gradually, the patient may experience dementia, memory impairment, and the person loses the ability to care for himself.
For symptoms, causes and first aid for stroke, watch the video below:
Other complications that have an unfavorable prognosis, including the death of the patient, are also possible.
First stage
At the first stage, there is a combination of classical complaints with a diffuse type of neurological symptoms, which manifests itself as anisoreflexia and a mild type of reflexes. It is also possible that the gait may change (walking may become slow, the patient often moves in small steps). The first stage is characterized by decreased coordination stability and uncertainty when performing movements.
Very often, doctors note emotional disturbances in patients in the form of irritability and anxiety, and depression is often observed. At this stage, minor cognitive deviations of the neurodynamic type occur, which implies exhaustion of the nervous system, decreased attention, and inertia of the intellect. However, in general, patients perform well on memory tests and on routine tasks, but only on tasks that do not require timed performance. Life activity and working abilities at the first stage are not limited for the patient.
Second stage
It is characterized by worsening neurological symptoms, which are characterized by the formation of an invisible syndrome, however, one that subsequently dominates. In addition, various kinds of extrapyramidal disorders can be detected, as well as ataxia, pseudobulbar syndrome, and even CN dysfunction. It is interesting that over time the complaints become less and less pronounced; they are no longer so acutely perceived by the patient himself. However, at this time the emotional background worsens and intensifies. There is an increase in cognitive function, up to the onset of neurodynamic disorders, which can later be supplemented by dysregulatory syndrome.
In addition, at the second stage, the patient’s ability to control his own actions deteriorates, and there are also difficulties in planning what the person wants to do at the next point in time. Although there is a violation in the performance of actions, the ability to compensate remains for a long time. In addition, signs of reduced social adaptation appear.
Forecast
Depends on the root cause. At the initial two stages - favorable. It is possible to completely reverse the process, restore cognitive functions and higher nervous activity in general.
When adding deviations of consciousness, gross deficits (behavioral disorders, mental disability), the likelihood of cure is already low. But there is still a chance to take control of the process.
However, it is recommended to consult a doctor at the very first stages when suspicious symptoms arise.
Third stage
It is distinguished by a clear manifestation of neurological syndromes. In this case, there is a disturbance in walking and the ability to maintain balance (the patient may often fall). Urinary incontinence is observed, and parkinsonian syndrome is also characteristic. Due to the absence or decrease in a sober understanding of what is happening to the patient, the volume of his complaints decreases.
Personality disorders can manifest themselves as inhibited reactions, explosive states, apathetic-abulic symptoms and psychological abnormalities. In addition to neurodynamic (or dysregulatory) disruptions in the cognitive sphere, the manifestation of such operational disorders as speech and memory impairment, decreased thinking ability, etc. is possible. All these symptoms can later develop into dementia. The latter leads to an inability to quickly adapt to a new situation and to a drop in performance in personal, social and professional areas of life. Very often, doctors indicate a person’s inability to work. At a certain point, the patient stops caring for himself.
Causes
Were already partially affected. The factors for the development of the pathological process are as follows.
- Atherosclerosis. Narrowing or blockage of the arteries of the brain and neck with cholesterol plaques.
- Angiospasm. Similar in nature to the first factor described. With the difference that it goes away on its own after a few hours or days. May be persistent.
- Arteritis, vasculitis. Inflammation of the inner lining of blood vessels. Has an infectious or autoimmune origin.
- Anatomical defects. Malformations, aneurysms. They pose a colossal danger in themselves and can provoke an emergency at any moment.
Instrumental studies
In order to determine the degree of damage to the blood vessels of the brain, as well as its substance, and to detect any other underlying diseases, doctors recommend undergoing such instrumental studies as:
- ECG;
- echocardiography;
- ophthalmoscopy;
- Doppler ultrasound (primarily, this study is performed for the main arteries of the head);
- cervical spondylography;
- triplex (or duplex) scanning of vessels of intracranial and extracranial types;
- vascular angiography (to detect vascular anomalies).
All patient complaints usually characteristic of the chronic type of cerebral ischemia can also be detected in various somatic pathologies and in some cases in oncology. The symptoms inherent in chronic cerebral ischemia can also be signs of various mental disorders and endogenous disorders. Therefore, differential diagnosis is necessary. But it will be problematic because chronic cerebral ischemia is often confused with neurodegenerative diseases, which share the same cognitive impairments and neurological manifestations.
Diseases with which chronic cerebral ischemia should be differentiated are:
- progressive supranuclear palsy;
- Parkinson's disease;
- corticobasal degeneration;
- Alzheimer's disease;
- multiple system atrophy.
Very often it is necessary to carry out a differential diagnosis of this disease with malignant and benign brain tumors, idiopathic dysplasia, normal pressure hydrocephalus and ataxia.
Diagnosis of cerebrovascular disease
Cerebrovascular disease is detected by neurologists and vascular surgeons.
To do this, a number of examinations are carried out:
- Blood test (general, biochemical).
- Analysis of urine.
- Electrocardiogram.
- Determination of prothrombin index.
- X-ray examination of the chest.
- Test for syphilis.
The photo shows the diagnostic procedure for CVD
- Angiography – makes it possible to assess the condition of blood vessels, identify aneurysm, thrombosis, cancer, atherosclerosis, etc.
- Angioscanning.
- Transcranial Doppler sonography makes it possible to detect changes in blood flow.
- Brain scintigraphy is a method that can be performed on absolutely all patients due to the absence of contraindications or restrictions. In this case, a special drug containing radioisotopes is injected into the vein and after 15 minutes a scan is performed. During this time, the substances of the drug manage to spread throughout the body, accumulating in those places where pathological changes began.
- CT scan.
- Magnetic resonance imaging.
Treatment of chronic cerebral ischemia
The main goal in the treatment of chronic cerebral ischemia is to stabilize the destructive process of cerebral ischemia in order to restore blood circulation in the vessels. Proper treatment will help slow down the rate of disease progression by activating the sanogenetic mechanism of function compensation. Therapy also involves the prevention of this disease and its attendants.
Pathology is not an indication for urgent hospitalization of the patient. Treatment in a hospital is necessary when the course of the disease is complicated by the development of a stroke condition or severe pathology. If a cognitive type of disorder is detected, if the patient is deprived of his usual environment, the condition may worsen.
Treatment of chronic ischemia is usually carried out by a neurologist on an outpatient basis. If the disease develops to stage 3, doctors prescribe patronage.
Diagnosis of CVD - is it that simple?
Specialists in the field of vascular surgery and neuropathology diagnose CVD. Based on the characteristics of the disease, doctors determine the treatment trajectory, first of all paying attention to the presence of concomitant diseases.
The first stage of the examination includes a general analysis of the course of the disease: clinical blood tests, urine tests, electrocardiography, determination of the prothrombin index, reaction to syphilis, biochemical blood tests, chest x-ray.
CVD can also be diagnosed using angioscanning (duplex or triplex). This method includes primary diagnosis, is the least expensive in terms of time and money, and is most beneficial for a person’s well-being. Angioscanning allows you to find out the extent of vascular damage without causing harm to health.
Another clinical diagnostic method is angiography, through which blood vessels are scanned under the influence of “contrast x-rays”.
This technique allows you to determine the degree of damage to blood vessels and find out how long ago the damage processes began. Angiography also helps to determine the presence of blood clots, hematomas, areas of narrowing or excessive expansion of the walls of blood vessels, as well as oncological pathologies.
Most clinics also offer scintigraphic analysis of the brain, MRI, transcranial Doppler sonography and CT.
Antihypertensive therapy
Antihypertensive therapy is aimed at maintaining normal blood pressure and stabilizing the state of chronic ischemia. If doctors prescribe antihypertensive drugs, the patient should be careful and monitor for fluctuations in their blood pressure. As is known, in the case of developing chronic ischemia, the mechanism of autoregulation of cerebral blood flow begins to work intermittently.
If we talk directly about antihypertensive drugs prescribed by doctors, then first of all we are talking about medications of two groups:
- angiotensin-converting enzyme inhibitors;
- angiotensin II receptor antagonists.
Drugs of both the first and second groups are capable of simultaneously exerting two effects: in addition to angiohypertensive, they are also angioprotective, which means protecting the affected organs, which usually include the kidneys, heart and brain. The effect of antihypertensive drugs usually increases significantly when they are combined with antihypertensive drugs such as hydrochlorothiazide and indapamide.
Treatment
The point is to eliminate the root cause. For atherosclerosis, statins are prescribed. Atoris as the main one. They remove cholesterol and dissolve existing cholesterol plaques.
Antiaggregants allow you to restore blood fluidity and prevent the formation of blood clots and clots that can block blood vessels. Aspirin, Heparin.
Anti-inflammatory, glucocorticoid drugs (Prednisolone, Dexamatezone and others), if necessary, antibiotics to eliminate arteritis and vasculitis. Lesions of the internal lining of blood vessels.
In fact, cerebrovascular agents and protectors are used to correct cerebral blood flow. Piracetam, Actovegin, nootropics like Glycine and others.
Operations are required in extreme cases, for example, if there is malformation, aneurysms, advanced atherosclerosis with plaque hardening. The question of the appropriateness of therapy is decided at the discretion of the specialist.
Lifestyle changes do not play a big role. It is enough to give up smoking and alcohol, minimize the amount of fatty foods and everything will fall into place. Adequate physical activity will not be superfluous.
Treatment of cerebrovascular insufficiency of the brain is medicinal, less often surgical, according to indications.
Combination drugs
In addition to the main therapy described above, depending on the mechanism that caused the disease, individual treatment is prescribed, which is designed to normalize the rheological properties of the blood and improve venous blood flow, bringing microcirculation back to normal. Typically, such drugs have neurotrophic and angioprotective properties. For example, a doctor may prescribe one of the following combinations:
- cinnarizine (no more than 75 mg) together with piracetam (1-1.2 g per day);
- piracetam (no more than 1.2 g) with vinpocetine (15 mg per day);
- nicergoline (no more than 30 mg per day) and pentoxifylline (approximately 300 mg per day).
Typically, such combinations of drugs are prescribed no more than twice a year, each course lasting approximately 2 months.
Development mechanism and reasons
There are at least four known processes that could be called cerebrovascular insufficiency. The pathogenesis, accordingly, is somewhat different.
The main option is atherosclerosis. This is a narrowing or, more often, blockage of the arteries with cholesterol plaques.
In the first case, the condition is transient, the stenosis recedes on its own. Not counting critical situations. Thus, in experienced smokers, spasm of the vascular muscles can last indefinitely.
The main danger here is the likelihood of spontaneous development of a stroke, acute neurosis of nerve clusters.
As for cholesterol plaques, they arise against the background of metabolic (metabolic) problems. Normally, lipids (fatty compounds) are eliminated from the body naturally. Only a small part of fats is absorbed due to enzymatic reactions.
If there is a metabolic disorder, the degree of absorption (absorption) will be higher, and accordingly more harmful compounds penetrate into the blood. In the short term, this leads to plaque growth. It blocks the blood flow.
The second option is thrombosis. Partial blockage of the lumen of a vessel with a blood clot. This formation of shaped cells is not always related to the brain. The original source can be anywhere. Most often these are the blood supply structures of the lower extremities.
The third possible situation concerns arteritis. Inflammation of the endothelial layer or lining of blood vessels. It develops as a complication of infections or an autoimmune process within systemic pathologies.
Finally, vascular malformations or aneurysms are also often found. The first are abnormal areas of communication between arteries and veins, the second are protrusions of the walls of a saccular or diffuse nature (along the entire diameter in a certain place).
What do the described pathologies have in common?
Despite the difference in the essence of the deviation, the disorders have one thing in common: the occurrence of a mechanical obstacle to the blood flow. Insufficient liquid tissue reaches the nerve clusters.
On the other hand, the body intensifies the work of the heart in order to compensate. And this is the path to increased blood pressure.
Thus, the risk of not only acute ischemia, when tissues lack trophism, increases, but also hemorrhage - rupture of a vessel from excessive stress, which is much more dangerous.
Attention:
All described conditions without treatment are fraught with acute cerebral insufficiency, which diagnostically corresponds to a stroke.
Prognosis and prevention
With timely diagnosis and correctly prescribed treatment, it is most often possible to stop the progressive course of chronic cerebral ischemia. If the disease is quite severe, being aggravated by parallel pathologies (for example, diabetes mellitus or hypertension), there may be a noticeable decrease in the usual ability to work, and sometimes even to the point of complete disability of the patient.
Among the preventive measures that can prevent this disease are the following:
- prevention of obesity in general, and in particular, obesity of cerebral vessels;
- active lifestyle;
- giving up alcohol and smoking;
- avoidance of stressful situations.
An important preventive measure will be the prevention of hypertension and diabetes. Not everyone knows that atherosclerosis can also contribute to the development of chronic cerebral ischemia, so it must be dealt with in the early stages.
As soon as a person discovers the first symptoms of chronic cerebral ischemia, one should immediately reduce the amount of alcohol consumed (or better yet, give it up altogether), reduce physical activity and avoid direct sunlight.
Signs of pathology
Cerebrovascular disease develops over a long period of time. At the initial stage of its development, the pathology manifests itself weakly and many attribute it to overwork. Therefore, almost no one seeks medical help at this time.
The first signs of CVD include:
- Fatigue quickly.
- Moderate headaches.
- Frequent irritability and mood swings.
- Dizziness.
Symptoms of progressive cerebrovascular disease
- General decrease in performance.
- Noise in the head.
- Memory impairment.
- Sleep problems.
All this can be a symptom of overwork, a stressful situation or physiological processes, even in healthy people. Therefore, no one expects to develop a serious illness.
Over time, symptoms of cerebrovascular disease occur more frequently and become more severe.
The patient is concerned about:
- Increased headache and noise in the head.
- Frequent dizziness, which may occur when moving or turning the head.
- Insomnia at night and feeling tired during the day.
- Visual impairment.
- Chronic depression and apathy. The patient begins to focus on his poor health.
One of the signs of pathology is insomnia
- Sometimes there may be a lack of sensation in the limbs.
- Speech disorder.
- Brief fainting.
- Decreased intellectual abilities, memory problems, which others begin to pay attention to.
If the patient does not immediately seek help from a doctor when such symptoms occur, then cerebrovascular disease is complicated by life-threatening conditions (stroke or ischemic attack).
It is important to remember that poor circulation in the brain has serious consequences. Due to the sharp restriction of blood supply to the cells of the organ, they begin to die. Depending on where this happened, a person may experience paresis, deterioration of vision or speech, paralysis or death.