Find out more about diseases starting with the letter “K”: Causalgia, Brain cyst, Cluster headache, Tick-borne encephalitis, Kozhevnikov epilepsy, Colloid cyst of the third ventricle, Coma, Compressive myelopathy, Balo concentric sclerosis, Radicular syndrome, Corticobasal degeneration, Craniovertebral anomalies, Craniospinal tumor, Craniopharyngioma, Myasthenia gravis crises, Hemorrhage into the ventricles of the brain.
Depending on the location of the formation, focal symptoms may be present. The diagnosis is made based on data from computed tomography and magnetic resonance imaging of the head or neurosonography (in children). Therapy consists of aspiration and surgical removal of the formation if complications develop or its growth progresses.
General information about pathology
A cyst is a fluid-filled cavity located in the substance of the brain or its membranes. When the pathology is small in size, it has a subclinical course and is diagnosed accidentally during a neuroimaging examination of the head. Since the intracranial space has limited dimensions, with a significant increase in the volume of the formation, intracranial hypertension develops.
The size of the cavity with liquid is largely determined by the compensatory capabilities of the formation and its localization. Due to the pliability of the skull bones in children at an early age, the cyst may not manifest itself for a long time.
The formation can be found in people of different ages, both in infants and in elderly patients. Even if the fluid cavity is congenital, it can make itself felt only by the age of 30-50.
According to generally accepted practice, treatment is prescribed only in the case of a pronounced clinical picture and when complications develop. If the cavity with fluid is frozen or slowly progressing and its volumes are insignificant, a wait-and-see approach is chosen, which involves regular monitoring of the patient.
Causes
There are several ways of developing inflammation of the arachnoid membranes and it has been established that arachnoiditis is polyetiological and can occur as a result of such factors as:
- past acute and chronic infectious processes (including influenza , rheumatism, measles , fever , sepsis , pneumonia , syphilis , tuberculosis , brucellosis , toxoplasmosis , osteomyelitis of the skull bones);
- inflammatory diseases of the nasal paranasal sinuses;
- acute or more often chronic suppurative otitis media , especially caused by low-virulent microorganisms or toxins;
- complication of suppurative otitis media, for example, labyrinthitis , petrositis , sinus thrombosis ;
- complication of cured purulent meningitis or brain abscesses;
- chronic intoxication with alcohol, lead, arsenic ;
- various injuries - craniocerebral and spinal cord (mainly as residual effects);
- reactive inflammation caused by slowly growing tumors or encephalitis, most often non-purulent otogenic.
Classification
Classification by location:
- Cerebral (intracerebral). It is formed in areas of dead brain tissue in the internal structures of the brain.
- Arachnoid. It is formed as a result of the accumulation of cerebrospinal fluid in places of adhesions formed as a result of inflammatory processes and in places of their congenital duplication. The advantage is localized in the meninges.
The following types of brain cysts are distinguished separately:
- dermoid;
- colloidal;
- choroid plexus;
- pineal gland.
According to its genesis, a cavity with fluid can be congenital or acquired. In turn, congenital is divided into colloid and dermoid, and due to its formation into post-infectious, post-traumatic, post-stroke and echinococcal.
Diet for arachnoiditis
Diet for the nervous system
- Efficacy: therapeutic effect after 2 months
- Timing: constantly
- Cost of food: 1700-1800 rubles per week
Treatment of arachnoiditis is best combined with a diet based on the principles of healthy eating:
- limited consumption of seasonings and salt;
- products containing refined sugar, butter, flour are excluded;
- meat should be of dietary grades - rabbit, turkey, chicken, etc.;
- no sausages or smoked meats;
- there should be fresh vegetables and fruits on the table;
- You need to enrich your diet with baked potatoes, cabbage and carrot salads, spicy and leafy greens;
- you need to add currants, sea buckthorn, persimmons, grapes, and raisins to dishes and teas.
Etiology and pathogenesis
The causes of a congenital cyst are unfavorable factors that occur during the development of the fetus. These are:
- fetal hypoxia during delivery;
- fetoplacental insufficiency;
- taking a specific group of medications by a pregnant woman;
- Rh conflict between mother and child;
- intrauterine infections.
Factors that provoke the development of a congenital cavity with fluid are drug, alcohol or nicotine addiction of the mother. In this case, the child’s development takes place under conditions of intrauterine intoxication, which negatively affects the brain structures. The causes of the cavity can also be chronic decompensated diseases of the expectant mother.
An acquired cavity with fluid in the head develops as a result of:
- inflammatory diseases (encephalitis, brain abscess, arachnoiditis, meningitis);
- traumatic brain injuries;
- injuries of newborns received during childbirth;
- cerebrovascular accidents (subarachnoid hemorrhage, ischemic stroke, hemorrhagic stroke).
Depending on the etiology, the following types of liquid cavities are distinguished:
- A cyst of iatrogenic origin forms as a complication after brain surgery.
- Parasitic - develops with paragonimiasis, cerebral form of taeniasis and echinococcosis.
A cavity with fluid can also replace cerebral tissue during degenerative and dystrophic processes in the head.
If a cyst is present, there are a number of factors that can trigger its growth. These include obstruction of venous outflow from the skull, strokes and other vascular disorders, as well as head injuries, hydrocephalus, and neuroinfections.
Examination and diagnosis
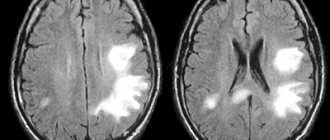
MRI or CT will provide unambiguous information about the presence, size and location of the cyst. A study with intravenous contrast helps to distinguish a cyst from a tumor You can perform such a study at the Clinic of the Academy of Sciences .
MRI scans of the brain. 1. Cyst after cerebral hemorrhage 2. Cerebellar cysts after ischemic stroke (blockage of cerebral arteries) 3. Cystic adhesive arachnoiditis
To avoid the enlargement and appearance of new cysts , we must clearly understand and treat the root cause of their occurrence. Therefore, we carefully examine you for circulatory disorders, infections, and autoimmune diseases.
Doppler ultrasound of the head and neck vessels (USDG) will help detect narrowing of the vessels that supply the brain with arterial blood. Lack of blood supply can lead to focal death of the brain matter and the appearance of cysts.
Heart studies (ECG, Echo-CG) . The brain may not have enough blood supply due to rhythm disturbances or heart failure.
Blood test for clotting and cholesterol. An increase in cholesterol concentration in the blood and increased clotting are the main causes of blockage of brain vessels with subsequent formation of cysts. This problem is easily solved with the help of modern medications.
Blood pressure monitoring. Episodic increases in pressure are a common cause of strokes and post-stroke cysts. A monitor is a small device that is constantly with you for 1 day and records your blood pressure on a memory card. The data is then read by a computer and gives the doctor a complete picture of the pressure for the day.
blood tests for infections and autoimmune diseases of the nervous system in cases of suspected neuroinfections, arachnoiditis, and multiple sclerosis.
Brain cyst
The growth of the formation at the initial stage is in most cases accompanied by symptoms of intracranial hypertension. Patients constantly complain of nausea, which has nothing to do with food, deterioration in general health and decreased performance, constant cephalalgia and pressure on the eyeballs.
In some cases, the main symptoms include a constant feeling of pulsation in the head, sleep disturbance, mild hearing loss, dizziness, motor dysfunction, fainting and tremors of the limbs. Possible visual impairment, namely double vision, visual hallucinations, deterioration of visual acuity. With high intracranial hypertension, the patient is worried about constant vomiting.
There are cases when the first signs indicating a cavity with fluid are the first occurrence of epileptic paroxysm. Subsequently, epileptic seizures recur. Paroxysms can take the form of focal Jacksonian epilepsy or absence seizures and be of a primary generalized nature.
Compared to general cerebral manifestations, focal symptoms are observed in fewer cases. These may be sensory disorders, monoparesis and hemiparesis, brainstem symptoms. The latter include dysarthria, eye movement disorders, and swallowing disorders.
One of the complications of formation is cyst rupture. In this case, hemorrhage due to rupture of the vessel, compression of the brain, the formation of an epileptogenic focus and occlusive hydrocephalus are possible.
In the congenital form of the cyst, episyndromes and intracranial hypertension are recorded at an early age. Education in the brain can cause the child to develop mental retardation and mental development disorders.
Schoolchildren
The causes of cysts in schoolchildren are most often associated with head injuries, inflammatory or infectious diseases such as meningitis, encephalitis.
If the cyst grows, the child may have headaches, nausea, numbness in body parts and other characteristic symptoms. Memory may deteriorate, behavior becomes more irritable.
Children of all ages need the supervision of a neurologist who will decide what measures to take and prescribe the appropriate treatment.
Types of brain cysts and their symptoms
Arachnoid - occurs in almost 4% of the population. A cavity with fluid can be congenital or acquired. In the latter case, it develops in response to traumatic brain injury. The formation is localized on the surface of the brain in its membranes. The cavity is filled with cerebrospinal fluid.
In most cases, an arachnoid cyst does not make itself felt for quite a long time and is discovered by chance. Severe symptoms appear only if a large amount of fluid accumulates in the cavity. In this case, cerebrospinal fluid is produced by the cells lining the cavity.
With a sharp increase in the volume of the cavity with liquid, it can rupture and, as a result, die.
Colloid cysts are recorded in 15-20% of all cases of formations inside the ventricles of the brain. Most often it is localized above the foramen of Monroe in the anterior region of the 3rd ventricle. Less common in the area of the transparent cerebral septum in the 4th ventricle.
The liquid filling the cavity of the colloid cyst has high viscosity. Patients experience symptoms of hydrocephalus and, with a certain position of the head, a paroxysmal increase in cephalgia is noted.
In rare cases, memory loss, behavioral disorders and weakness in the limbs occur.
Pineal cyst of the pineal gland - according to statistics, 10% of patients have formations of this type that are small in size and do not make themselves felt. Cystic formations are localized in the epiphysis of the brain, in most cases they are no more than 1 cm in size. Otherwise, symptoms appear. When it grows, it can block the entrance to the “plumbing” of the brain and block the circulation of cerebrospinal fluid, causing occlusive hydrocephalus.
Epidermoid or dermoid is a formation that is an anomaly of intrauterine development. In this case, the cells of the baby's future skin and its appendages remain inside the brain. Accordingly, in addition to liquid, elements of the ectoderm are present, namely sebaceous glands and hair follicles.
After the birth of a child, such a cyst quickly increases in size. The only possible treatment is surgical removal of the formation.
Choroid plexus cyst - forms regardless of the person’s age. In this case, the space between the plexus vessels is filled with cerebrospinal fluid. Symptoms are rarely present, sometimes accompanied by epileptic seizures and symptoms of intracranial hypertension.
With a congenital choroid plexus cyst, the formation is diagnosed at the 20th week of intrauterine development using ultrasound. By the 28th week, such formations resolve.
Materials
Authors:
| D.V. Ivanov, St. Petersburg State University, Faculty of Medicine, Institute of Osteopathy, Russia |
| S.V. Novoseltsev, St. Petersburg Medical Academy of Postgraduate Education, Institute of Osteopathic Medicine, Russia |
SUMMARY
Cranial biomechanical disorders play a significant role in the pathogenesis of secondary hypertensive-hydrocephalic syndrome in patients with arachnoid cysts . Taking into account the peculiarities of the pathogenesis and clinical picture in children with arachnoid cysts, the polymorphism of osteopathic findings, as well as data from neurophysiological studies, a basic scheme of osteopathic treatment of this pathology was proposed for the first time. There is a significant improvement in the clinical picture in patients with arachnoid cysts, which is confirmed by modern methods of neuroimaging and functional diagnostics. Osteopathic correction in the complex treatment of this pathology significantly expands therapeutic possibilities and reduces the treatment time for such patients.
Key words: hypertensive-hydrocephalic syndrome , arachnoid cyst , cranial biomechanical disorders , osteopathic correction .
Arachnoid cysts, accounting for about 1% of all intracranial space-occupying formations, are one of the forms of dysontogenetic cerebral anomalies. In most cases, they are formed in the prenatal period, are located extracerebrally, are formed by a duplicate of the arachnoid membrane and are benign. CSF-like fluid accumulates in the cyst over time, which can subsequently lead to a gradual increase in its volume. With an increase in the size of the cysts, an increase in the corresponding general cerebral and focal neurological symptoms is observed.
Currently, no effective drug treatment has been developed for arachnoid cysts. Only symptomatic or surgical treatment is used. This type of pathology, despite its rarity, remains relevant, since only surgical treatment is most effective and provides a complete cure. However, the opinions of clinicians and researchers on the management of patients with arachnoid cysts of the brain remain controversial. Some authors believe that it is enough to limit themselves to symptomatic conservative therapy (Auer LM et al.. 1981; Galassi R. et al., 1985; Artico M. et al., 1995), while others consider surgical intervention necessary (Brandt M. et al.. 1986; Kang J.K. et al., 2000; Kandenwein JA et al., 2004). In addition, there is no clarity in determining the indications for surgical intervention.
Purpose of the study: to improve the effectiveness of treatment of arachnoid cysts (AC) accompanied by secondary hypertensive-hydrocephalic syndrome (HHS) in children.
TASKS
To study the features of the clinical picture in patients with arachnoid cysts.
To identify biomechanical disorders in this category of patients.
Identify risk factors for the development of AK and secondary HGS.
To develop an algorithm for the treatment of patients with AK accompanied by secondary HGS.
To evaluate the effectiveness of osteopathic treatment of AK in comparison with drug treatment in these patients.
An arachnoid cyst is a cerebrospinal fluid cyst, the walls of which are formed by the cells of the arachnoid membrane or scar collagen. Arachnoid cysts are localized between the surface of the brain and the arachnoid membrane. Arachnoid cysts, along with arachnoiditis and hydrocephalus, are diseases of the cerebrospinal fluid circulation system and are characterized by liquorodynamic disorders.
The origin of arachnoid cysts of the brain has not yet been fully studied. Each of the existing theories explains it only partially, leaving a number of questions about the pathogenesis of this pathology unresolved (Starkman SP et al., 1958; Robinson RG, 1964,1971; Fox JL, Al-Mefty 0., 1980; Brackett CE, Rengachary SS, 1982 ).
However, most researchers claim that the formation of arachnoid cysts is congenital. Pierre-Kahn et al. (2000), based on ultrasound studies of the fetus over time, provide data that arachnoid cysts in most cases form at the 20-30th week of gestation.
Primary arachnoid cysts are congenital formations; secondary cysts arise as a result of meningitis, surgery, or birth trauma. Arachnoid cysts are 4 times more common in men than in women; usually localized in areas rich in arachnoid membranes of the liquor cisterns, expanding them. Most often, arachnoid cysts form in the middle cranial fossa, outside the temporal lobes of the brain.
Clinical manifestations and their dynamics depend on the location, changes in the volume of the cyst and the age of the patient. In cases where they remain unchanged, the clinical symptoms remain unchanged throughout the patient’s life; in other cases, with an increase in the size of the cysts, an increase in the corresponding general cerebral and focal neurological symptoms is observed.
Microscopically it was established that the inner wall of the cyst adjacent to the brain passes directly into the outer wall. Thus, the arachnoid membrane of the underlying parts of the brain directly passes into the outer wall of the arachnoid cyst, thereby forming a duplication. The cyst cavity turns out to be limited on all sides by the arachnoid membrane. The differences between the inner and outer walls are determined only by the thickness, which depends on the number of collagen fibers and focal proliferation of the arachnoid endothelium of varying intensity. Signs of inflammation are usually not detected.
With congenital arachnoid cysts, an abnormal structure of the arachnoid membrane is observed with the formation of its duplication, between the walls of which cerebrospinal fluid accumulates, resulting in a disruption of its circulation and outflow.
In embryogenesis, in conditions of disruption of the formation of the membranes of the brain and the formation of the cerebrospinal fluid circulation system, which functions as a single circle, including three links - cerebrospinal fluid production, cerebrospinal fluid circulation and cerebrospinal fluid outflow - apparently, it becomes possible to form microcavities in the thickness of the arachnoid membrane, which subsequently increase in size and turn into arachnoid cysts. Due to a violation of the ratio of the inflow of cerebrospinal fluid and its outflow outside the cyst through the arachnoid membrane, the cyst increases in size. When equilibrium is established between these processes, the size of the cyst does not change.
Liquor enters the cyst cavity either from cisterns (communicating cysts) or from the subarachnoid space through its inner wall (arachnoid membrane). The outflow of cerebrospinal fluid occurs through the arachnoid membrane into the subdural space and further into the internal capillary network of the dura mater.
From the cyst, the outflow of cerebrospinal fluid occurs through its outer wall (arachnoid membrane). The more severe the fibrosis of the outer wall of the cyst, the more difficult the process of outflow of cerebrospinal fluid through it becomes.
About 80% of arachnoid cysts are localized in structures above the tentorium of the cerebellum and are divided into cysts of the cerebral hemispheres (lateral fissure, convexital surface of the cerebral hemispheres, parasagittal) and mid-basal localization (suprasellar, tentorial notch, posterior cranial fossa). The leading link in the pathogenesis of the disease is a violation of liquor circulation, the drainage function of the intrathecal space of the brain and the resorption of cerebrospinal fluid.
The appearance of its first symptoms is possible only several months or even years after the birth of the child. Typical for these cysts are the pseudotumorous nature of the process and the absence of signs of inflammation in the membranes of the brain. Neurological symptoms of the disease are manifested by a triad: hypertensive-hydrocephalic syndrome, focal symptoms, signs of damage to the brain stem.
In the clinical course of the disease, phases are distinguished: compensation, subcompensation and decompensation.
The compensation phase means an asymptomatic course; a sign of decompensation is progressive hydrocephalus. In young children, this is bulging and tension of the fontanelles, divergence of cranial sutures, and increasing delay in psychomotor development.
In older patients, headache and vomiting, congestive optic discs, and severe focal and dislocation symptoms appear. The subcompensation phase is characterized by severe symptoms of brain damage. With arachnoid cysts of the cerebral hemispheres, the characteristic triad of syndromes may be absent or slightly expressed due to a compensatory increase in the volume of the skull. The clinical course of the disease remains compensated or subcompensated. In medical practice, general cerebral symptoms associated with secondary hydrocephalus are more often observed, and focal symptoms are less common.
Arachnoid cysts are either asymptomatic or appear before the age of 20, while the nature and severity of symptoms, depending on the location and size of the cysts, make diagnosis difficult.
ACs of the mid-basal region, due to their close location to the cerebrospinal fluid tract, brainstem and diencephalic structures, manifest themselves with pronounced brainstem, diencephalic and cerebellar symptoms and tend to progress. These differences determine the choice of diagnostic methods and treatment tactics.
Arachnoid cysts are usually identified and differentiated from other types of cysts with MRI , CT , and ultrasound examinations, as well as with the help of anamnesis, neurological examination and topical diagnostics.
An important role in the diagnosis of the disease belongs to magnetic resonance imaging of the brain , which allows not only more accurate early diagnosis of cysts, but also to trace the course of the process over time.
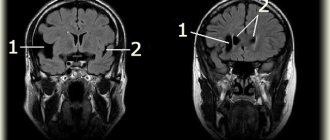
On MP tomograms, an arachnoid cyst looks like a uniformly intense zone of reduced density, close to the density of the cerebrospinal fluid, with clear, not always smooth edges (Fig. 1 and 3). In some cases, it is possible to trace the connection of cysts with the subarachnoid cisterns of the brain, as well as to detect thinning of the bones of the calvarium adjacent to the cyst or their erosion. When the cyst is localized in the middle cranial fossa, signs of hypoplasia of the temporal lobe may be detected.
Thus, macrocephaly developing in young children may be a symptom of not only congenital hydrocephalus. In the asymptomatic clinical course of macrocephaly, congenital hydrocephalus must be differentiated from other pathological processes accompanied by an increase in intracranial contents, primarily with an arachnoid cyst.
Detected arachnoid cysts in children can probably be a post-traumatic phenomenon, since the anamnesis of these patients often includes rapid labor, cesarean section, application of obstetric forceps and obstetric aid. Children diagnosed with an arachnoid cyst who do not have neurological symptoms and any clinical manifestations are not operated on.
MATERIALS AND METHODS OF RESEARCH
The work was carried out on the basis of children's clinic No. 5 in Nizhnevartovsk, Khanty-Mansi Autonomous Okrug-Yugra. We examined 30 patients. The selection of patients for examination was carried out on the basis of a complete clinical examination, taking into account complaints, anamnesis, and instrumental research methods.
Before and after treatment of patients, traditional clinical examination methods (history collection, objective examination data), neurosonography, Doppler ultrasound with duplex scanning of the great vessels of the head and neck were used.
The criteria for inclusion in the group were: confirmed diagnosis of arachnoid cyst of the brain (MRI, NSG), neurological examination, consultation with a neurosurgeon. The size of the AK was no more than 3x3 cm. Two groups of 15 people were formed. Group I (control group) received only drug treatment, group II (main group) received drug and osteopathic treatment.
Patients of group I (control group) received standard conservative treatment, which included dehydration, stimulating, vascular treatment, and resorption therapy. The selection of drugs and their doses was carried out individually, depending on the patient’s condition, but according to generally accepted methods. Treatment was prescribed and monitored by a neurologist once a month.
Patients from group II (main group), in addition to drug treatment, received osteopathic treatment, including restoration of the kinetics of the elements of the craniosacral system.
Patients were standardized by gender, age and neurological symptoms (p<0.01 according to Fisher's criteria and x2). The age of the patients was 6.5+5.3 in the main group and 6.7±6.1 in the control group. The distribution of patients by gender and age is presented in the table.
DISTRIBUTION OF PATIENTS BY GENDER AND AGE
| Floor | Main group | Comparison group | ||
| Abs. | % | Abs. | % | |
| Husband. | 9 | 60 | 7 | 46.6 |
| Women | 6 | 40 | 8 | 53.3 |
| Age, years | ||||
| 3-6 months | 6 | 40 | 5 | 33.3 |
| 6-12 months | 2 | 13.3 | 4 | 26.6 |
| 1-1.5 year | 7 | 46.6 | 6 | 40 |
We analyzed the obstetric history of pregnancy and childbirth, the features of the clinical picture of the arachnoid cyst; The main clinical, ultrasound and osteopathic changes before and after treatment were identified and assessed. To assess the effectiveness of osteopathic therapy, a comparison was made of the main clinical, ultrasound and osteopathic changes in the main group with similar indicators in the comparison group.
Osteopathic examination included assessment of the craniosacral mechanism, cervical spine, sacrum and was carried out using classical methods. The following techniques were used:
- correction of dysfunctions of sphenobasilar synchondrosis;
- correction of the craniovertebral junction;
- technique for draining venous sinuses;
- fourth ventricle compression technique;
- “temporal bone rolling” technique;
- Pan Dura technique;
- technique of balancing the dura mater of the frontal region;
- fronto-occipital balancing technique;
- L5-S1 decompression technique;
- core-link technique;
- sacroiliac joint decompression technique;
- correction of dysfunctions C0-C1 and L5-S1.
Osteopathic treatment of children in the main group was carried out no more than once a week. The number of treatment sessions performed was determined by the dynamics of neurological and osteopathic status and varied from 5 to 10 procedures. The rehabilitation period averaged from one and a half to three months.
The data obtained during the study were processed on a computer using the STATISTICA for Windows software system.
RESEARCH RESULTS AND DISCUSSION
A comparative analysis of pre- and perinatal risk factors (complications of pregnancy and childbirth) showed that the most common (48.33%) birth pathology (fetal traction, extrusion, breech presentation). In many cases, drug labor stimulation was used and a long period of labor was noted. A third of the children had a large weight (more than 4000 g) at birth. A detailed analysis of risk factors for the development of AK is presented in Diagram 1.
The results of a neurological examination of patients with AK are presented in Table. 2
table 2
DATA OF NEUROLOGICAL EXAMINATION BEFORE STARTING OSTEOPATHIC TREATMENT
| Main group, % | Control group, % | |
| Increase in head circumference compared to age norm | 33.1 | 34.0 |
| Increased vascular pattern on the scalp | 30.2 | 31.0 |
| Skull dehiscence | 26.1 | 29.4 |
| General brain symptoms | 67.5 | 66.3 |
| Focal neurological symptoms | 32.5 | 33.7 |
During a neurological examination of the main group and the comparison group, most children showed an increase in the rate of head growth compared to the age norm (33.1% in the main group and 34% in the control group) and an increase in the vascular pattern on the scalp (30.2 and 31% cases respectively). In this case, a mild divergence of the cranial sutures was detected (26.1% in the main group and 24.9% in the control group). General cerebral symptoms (67.5 and 66.3%, respectively) and focal cerebral symptoms (32.5 and 33.7%, respectively) were detected (p < 0.01 by Fisher’s criteria and x2).
After a course of drug and osteopathic treatment, positive dynamics in the neurological status were noted; according to ultrasound data, a decrease in the volume of the brain cyst and a decrease in intracranial pressure were observed. During a neurological examination, a decrease in hypertonicity was noted after the first procedure, normalization occurred after the third. The rate of increase in head circumference decreased after two procedures and normalized after four. Regurgitation and pulsation of the fontanel decreased after the first procedure and disappeared after the third. After rehabilitation, the majority of children (70.0%) showed no neurological manifestations of AK. In 30.0% of patients there was a decrease in the severity of neurological signs.
Data on the neurological status after osteopathic treatment are presented in Table. 3.
Table 3
DATA OF NEUROLOGICAL EXAMINATION AFTER OSTEOPATHIC TREATMENT
| Main group, % | Control group, % | |
| Increase in head circumference compared to age norm | 8.1 | 29.0 |
| Increased vascular pattern on the scalp | 5.9 | 27.6 |
| Skull dehiscence | 6.1 | 17.9 |
| General brain symptoms | 67.5 | 66.3 |
| Focal neurological symptoms | 12.8 | 44.3 |
An osteopathic examination of children in the main group and the comparison group revealed a dysfunction of the craniosacral system, manifested in a slowdown in the rhythm and amplitude of mobility of the SBS and sacrum. These disorders manifested themselves in the form of compression of the SBS of 20% in the main and 26.6% in the control group (p <0.01 according to Fisher’s criteria and x2). Compression of C0-C1 was detected in all children (p <0.01 according to Fisher’s criteria and x2). The majority of children (93 and 86.6%, respectively) had SBS strains. Compression of L5-S1 was also detected (66.6 and 73.3%, respectively), which was manifested by impaired sacral kinetics. Side-bading with rotation was detected in more than half of the cases: 73.3 and 80%, respectively. In all subjects, torsion of the SBS was detected.
Table 4
RESULTS OF OSTEOPATHIC EXAMINATION BEFORE TREATMENT
| Osteopathic dysfunctions | Main group | Comparison group | ||
| Abs. | % | Abs. | % | Abs. |
| SBS compression | 3 | 20,0 | 4 | 26,6 |
| Compression C0-C1 | 15 | 100 | 15 | •oo |
| Compression L5-S1 | 10 | 66,6 | 11 | 73,3 |
| Lateral strain | 14 | 93,0 | 13 | 86,6 |
| Torsion SBS | 100 | 15 | 100 | 15 |
| Side-bading with SBS rotation | 11 | 73,3 | 12 | 80,0 |
Osteopathic status before treatment
Two thirds of the children had displacements at the level of parts of the occipital bone. Moreover, more often (p<0.01 according to Fisher's criteria and x2) anteroposterior displacement of the scales relative to the condylar parts along the transverse axis was noted during compression of the skull in the birth canal. A significant number of children (93 and 86.6%, respectively) had lateral SBS strains. More than half of the children (66.6 and 73.3%, respectively) in both groups had compression at the level of the lumbosacral spine (L5-S1), which was manifested by impaired sacral kinetics. Apparently, impaired mobility of the SBS and mutual tension membranes, functional blocks of the cervical-occipital and lumbosacral junctions lead to venous stasis, impaired liquor outflow, which, in turn, leads to the accumulation of cerebrospinal fluid in the AC cavity. An arachnoid cyst, depending on its location, gives specific symptoms. Having increased in size, the AC interferes with the outflow of cerebrospinal fluid and causes secondary hydrocephalic hypertension. This is confirmed by instrumental data and neurological examination.
Table 5
RESULTS OF OSTEOPATHIC EXAMINATION AFTER TREATMENT
| Damage | Main group | Comparison group | ||
| Abs | % | Abs. | % | |
| SBS compression | 0 | 0 | 4 | 26,6 |
| Compression C0-C1 | 1 | 6,6 | 15 | 100 |
| Compression L5-S1 | 0 | 0 | 11 | 73,3 |
| Lateral strain | 2 | 13,2 | 13 | 86,6 |
| Torsion SBS | 2 | 13,2 | 15 | 100 |
| Side-bading with rotation | 1 | 6.6 | 12 | 80,0 |
Osteopathic status after treatment
A neurosonographic examination of children in the main group and the comparison group revealed an increase in the width of the lateral ventricles and an increase in the body index of the lateral ventricle in all patients. Enlargement of the third ventricle was observed in 51.67 and 53.33% of children, respectively. The majority of children showed widening of the interhemispheric fissure (66.67 and 68.33%).
Data on the dynamics of NSG before and after treatment are presented in Table. 6 and 7.
Table 6
NEURSONOGRAPHY DATA BEFORE OSTEOPATHIC TREATMENT
| NSG signs | Main group, % | Control group, % |
| Increased width of the lateral ventricles | 23,40 | 25,00 |
| Increased body index of the lateral ventricles | 21,00 | 24,56 |
| Enlargement of the third ventricle | 51,67 | 53,33 |
| Expansion of the interhemispheric fissure | 66,67 | 68,33 |
NEURSONOGRAPHY DATA BEFORE OSTEOPATHIC TREATMENT
Table 7
NEURSONOGRAPHY DATA AFTER OSTEOPATHIC TREATMENT
| NSG signs | Main group, % | Control group, % |
| Increased width of the lateral ventricles | 7,5 | 19,7 |
| Increased body index of the lateral ventricles | 6,3 | 20,04 |
| Enlargement of the third ventricle | 11,7 | 48,2 |
| Expansion of the interhemispheric fissure | 12,6 | 57,1 |
NEURSONOGRAPHY DATA AFTER OSTEOPATHIC TREATMENT
Table 8
SUMMARY TABLE OF ULTRASOUND RESULTS AFTER TREATMENT OF PATIENTS WITH AK
| Main group | Comparison group | |||
| Number of people | % | Number of people | % | |
| Stabilization | 2 | 14 | 9 | 60 |
| The decrease is insignificant | 4 | 38.85 | 4 | 27 |
| Reduction by 50% or more | 8 | 47 | 0 | 0 |
| Deterioration | 0 | 0 | 2 | 13 |
| Complete regression | 1 | 0,15 | 0 | 0 |
ULTRASOUND RESULTS AFTER TREATMENT OF PATIENTS WITH ARACHNOIDAL CYST DIAGNOSIS
Data from duplex scanning of the main arteries and veins of the head and neck showed that the greatest changes in children in the two groups concerned venous outflow. In 69.57% of children in the main group and 72.22% in the comparison group, venous dysgemia in the jugular vein was very pronounced. 47.83% of patients in the main group and 44.44% of the comparison group also had severe dysgemia in the vertebral veins. At the level of the cavernous sinus, pronounced changes were observed in 56.52 and 61.11% of children, respectively. Arterial blood flow disorders were mainly associated with the vertebrobasilar region. Hemodynamic disorders were manifested in the majority of subjects by asymmetry of linear blood flow velocity (LBV) in the vertebral arteries (79.91 and 72.22%, respectively) and asymmetry of their diameter (60.87 and 61.11%, respectively). In the carotid basin, disturbances were insignificant. Vascular hypoplasia was excluded in all children.
Duplex scanning data of the main arteries and veins of the head and neck
Duplex scanning data of the main arteries and veins of the head and neck at the extra and intracranial level after treatment
Results of duplex scanning of the great vessels of the head after treatment
According to the results of the duplex study, normalization of hemodynamic parameters was noted in 73.9% of children, and in the rest - an improvement in these parameters (26.1%). There was no stabilization or deterioration. When comparing the results of duplex scanning of the great vessels of the head after treatment, we obtained the following data: normalization of hemodynamics concerned both venous and arterial components and amounted to 73.9% in the main group and 22.2% in the comparison group. The improvement in hemodynamic parameters in the main group (26.1%) occurred primarily due to the normalization of venous outflow through the jugular and vertebral veins. Arterial blood flow in the vertebrobasilar region was well restored. A longer time was required to normalize venous blood flow along the sinus cavernosus and arterial blood flow in the carotid system. In the comparison group, the improvement (55.6%) concerned more arterial blood flow in the carotid and vertebrobasilar regions. Venous dyshemia regressed more slowly in the jugular and vertebral veins. In the comparison group, in 22.2% of children, hemodynamic disorders remained the same. When statistically processing the results of duplex scanning of the great vessels of the head after treatment in two groups, we obtained statistically significant differences (p < 0.001 according to Fisher’s criteria and x2).
In the main group, according to the NSG data, 47% showed a decrease in the size of the AC by two times or more. The decrease in AC size was also confirmed on MP tomograms (Fig. 1-4).
Rice. 1. Patient N., 1.5 years old. MRI of the brain before osteopathic treatment :
MRI of the brain before osteopathic treatment
1 - normal slit-like fluid space between the temporal and parietal lobes of the brain;
2 - arachnoid cyst, accumulation of fluid is visible
Rice. 2. Patient N., 1 year 7 months. MRI of the brain after osteopathic treatment :
MRI of the brain after osteopathic treatment
1 - normal slit-like fluid space between the temporal and parietal lobes of the brain;
2 - the same arachnoid cyst after a course of osteopathic treatment
Fig.3. Patient K., 10 months. MRI of the brain before osteopathic treatment :
MRI of the brain before osteopathic treatment
1 - ventricles of the brain;
2 - arachnoid cyst
Rice. 4. Patient K., 1 year. MRI of the brain after osteopathic treatment :
MRI of the brain after osteopathic treatment
1 - ventricles of the brain;
2 - the same arachnoid cyst, a decrease in the volume of the cyst is visible
When assessing the dynamics of AK manifestations against the background of osteopathic correction, we used the following concepts:
- normalization (absence of complaints; absence of clinical symptoms of AK; normalization of the sizes of liquor-containing spaces, confirmed by NSG data; normalization of hemodynamic parameters, confirmed by duplex scanning data, absence of displacements at the level of the cervical and sacral vertebrae; absence of osteopathic disorders);
- improvement (reduction of complaints; reduction in the size of liquor-containing spaces; improvement of hemodynamic parameters; reduction of displacements at the level of the cervical and sacral vertebrae; reduction of the severity of osteopathic disorders);
- stabilization (lack of dynamics in clinical manifestations, complaints and objective research methods);
- deterioration (increased clinical manifestations with negative dynamics from instrumental research methods).
The effectiveness of treatment in the main group is presented in Diagram 13.
The effectiveness of treatment in the main group according to the dynamics of neurological status, ultrasound, osteopathic status
During the treatment of children from the main group, all children noted a decrease in complaints after the first procedure; after the third, a stable improvement in their condition .
The effectiveness of treatment according to the dynamics of ultrasound signs of an arachnoid cyst after 3 months
The effectiveness of treatment according to the dynamics of neurological and osteopathic status of an arachnoid cyst after 3 months
Assessing the dynamics of AK manifestations against the background of osteopathic rehabilitation, data processing revealed a statistically significant dependence of the rehabilitation results on the age of the patients (with p <0.001 according to Fisher’s criteria and x2). Our study showed that the earlier rehabilitation began, the better the results.
The first comparative analysis of the dynamics of AC and HGS in children of the two groups was carried out three months after treatment. The assessment concerned the presence or absence of complaints, NSG data, Doppler sonography, neurological and osteopathic status. During the follow-up examination of children according to the NSG data, the results presented in diagram 14 were obtained. During the neurological and osteopathic examination of children, the dynamics presented in diagram 15 were revealed. When statistically processing the results of the follow-up examination of children after three months, we obtained differences that were statistically significant (p< 0.001 according to Fisher criteria and x2) for complaints, NSG data, Doppler sonography, neurological and osteopathic status.
The second stage of dynamic control of the AC and HGS in children of the two groups was carried out six months later. The assessment covered the same parameters as in the first assessment, as well as the dynamics of duplex scanning data after treatment. Based on NSG and Doppler ultrasound data, we obtained the results presented in Diagram 16.
The effectiveness of treatment according to the dynamics of ultrasound signs of AK after 6 months
Neurological and osteopathic examination of children also revealed statistically significant positive dynamics (p<0.001 according to Fisher and hg criteria).
CONCLUSION
During the analysis of the pathophysiological causes of AK, the predominance of impaired outflow and resorption of cerebrospinal fluid was established. According to the duplex study, in all children, as a rule, a violation of the venous outflow was detected both in the jugular and vertebral veins, which led to difficulty in circulation and resorption of cerebrospinal fluid. Osteopathic examination revealed factors leading to the occurrence of these disorders. This is a violation of the kinetics of SBS, the functional block C0-C1, L5-S1, disharmonious tension of the reciprocal tension membranes.
The data obtained led to the conclusion that osteopathic treatment of young children with arachnoid cysts is effective. In 86.67% of cases, there was a complete recovery of children in the main group , and in 13.33% there was an improvement in condition. There was not a single child with negative dynamics of AC. The treatment period averaged from one and a half to three months. In children in the comparison group who received standard treatment regimens, recovery was noted in 30.0% of cases, deterioration in 55.0%, and 15.0% of children stabilized their condition by 1 year. The high effectiveness of osteopathic correction was directly related to the ability of osteopathic techniques to influence the pathophysiology of the process of arachnoid cyst formation. The reliability of the results of osteopathic rehabilitation is confirmed by instrumental neuroimaging methods and statistical research. When statistically processing the results after treatment in the two groups, we obtained statistically significant differences (p < 0.001 according to Fisher and hg criteria). When treating children in the comparison group, the low percentage of recovery and long treatment periods were due to the persistence of identified biomechanical disorders, which continued to create obstacles to normal blood flow, and, consequently, to the outflow and resorption of cerebrospinal fluid. This was confirmed by duplex scanning. The persistence of extravasal influences on hemodynamics in the vertebral arteries did not allow normalization of blood flow in such children. In half of the cases it was necessary to change medications due to various reactions to them (excitement, dyspepsia, skin rash).
CONCLUSIONS
- A significant link in the pathogenesis of arachnoid cysts are somatic dysfunctions of the SBS, craniovertebral junction, lumbosacral junction, imbalance of receptive tension membranes, which leads to disruption of cerebrospinal fluid dynamics and venous outflow.
- The risk factors we identified have a significant impact on the development of AK and secondary
- GGS.
- It is advisable to include neurosonography, MRI, and Doppler ultrasound in the algorithm for diagnosing and monitoring the progress of osteopathic treatment of patients with AK.
- In the treatment algorithm for patients with AK. accompanied by secondary HGS, it is advisable to include osteopathic correction of the craniosacral system.
- Osteopathic treatment in combination with drug treatment is more effective in the treatment of arachnoid cysts and secondary HGS compared with isolated drug treatment.
LITERATURE
1. Badalyan. L.O., Zhurba. P.T.. Vsevolozhskaya. N.M. Guide to early childhood neurology. - Kyiv. 1980.
2. Barashnev, Yu.I. Diseases of the nervous system in newborns. - M., 1971.
3. Baron, M.A., Mayorova, N.A. Functional stereomorphology of the meninges. - M., 1982.
4. Volodin, N.N., Medvedev, M.I.. Gorbunov, A.V. Computed tomography of the brain in newborns and young children. - M.: Geotar-Med, 2002. - 119 p.
5. Dobrovolsky, G.F. II Issues of neurosurgery. - 1974. - No. 2. - P. 32-39.
6. Konovalov, A.N., Kornienko, V.N., Pronin, I.N. Magnetic resonance imaging in neurosurgery. - M.: Vidar, 1997.
7. Konovalov, A.N.. Kornienko, V.N. Computed tomography in a neurosurgical clinic. - M.: Medicine, 1985.
8. Kornienko, V.N., Ozerova, V.I., Pronin, I.N. Neuroradiology of childhood. - CD-ROM, LLC "PO Vidar", 2002.
9. Kuzenkova, L.M., Vavilov, SB. Towards the diagnosis of arachnoid cysts in young children. - ZhNIP im. S.S. Korsakov. 1990; 90(8): 13-6.
10 Novoseltsev, SV. Introduction to osteopathy. Craniodiagnosis and correction techniques. - St. Petersburg: Foliant Publishing House LLC. 2007. - 344 p.
11. Novoseltsev, SV. Introduction to osteopathy. Private cranial osteopathy. - St. Petersburg. : Foliant Publishing House LLC, 2009.-352 p.
12. Rostovtsev. DM. Endoscopy in pediatric neurosurgery: a manual for doctors / Khachatryan V.A., Samochernykh K.A., Kim A.V., Kommunarov V.V., Beskrovny A.S., Gogoryan S.F., Rostovtsev D.M. - St. Petersburg, 2004.
13. Rostovtsev, DM. Rational tactics for the treatment of hydrocephalus / Kommunarov V.V., Samochernykh K.A., Rostovtsev D.M. // Damage and diseases of the nervous system. - Kirov. 2005. - pp. 65-66.
14. Rostovtsev, D.M. Intraoperative endoscopy in the treatment of neurosurgical diseases in children / Khachatryan V.A., Samochernykh K.A., Rostovtsev D.M. // Damage and diseases of the nervous system. - Kirov, 2005.-S. 117-119.
15. Rostovtsev, DM. Results of surgical treatment of arachnoid cysts of the posterior cranial fossa / Rostovtsev D.M., Samochernykh K.A. // Polenov readings. - 2006. - P. 264-265.
16. Rostovtsev, DM. Results of surgical treatment of convexital supratentorial intracerebral cysts of the brain in children.
17. Rostotskaya, V.I., Ivakina, N.I., Kornienko, VN. and others. II 4th All-Union Congress of Neurosurgeons: Abstracts of reports.-M., 1988.-P. 277-278.
18. Shcherbakova, E.Ya., Kulakova, S.V., Ozerova, V.I. and others. SPECT data for arachnoid cysts of the brain and hydrocephalus in children. Advanced treatment technologies at the turn of the century // Mat. international symposium. - M., 2000; 97.
19. Caporossi, R., Peyralade, F. Traite pratique d'Osteopatique cranienne. SI 0. Paris, Ed. De Verlaque, 1992.
20. Frymann, V.M. The trauma of birth // Osteopathic Annals, 1976. - P. 56-68.
21. Jacoby, R., Levy, R., Dawson, J. Computed tomography in the elderly: 1. The normal population // Br. J. Psychiatry. - 1980; 135:249-2550.
22. Lee, SH, Rao, KC Cranial computed tomography and MRI. Mc. Crow-Hill Book Company. - NY, 1987; 858.
23. Magoun, HJ The cranial concept in general practice // Osteopathic Annals, 1964. - P. 32.
24. Still, AT Osteopathy. Research and practice. - Eastland Press, 1992. - P. 5-39; 145-147.
25. Upledger, J. E., Vredevoogd. JD Craniosacral therapy. - Seattle: Eastland Press, 1983. - P. 348.
26. Weisberg, L. Nace. With Cerebral computed tomography. A text atlas. W. B. Saunders Company. Philadelphia. 1989; 399-430.
S.V. Novoseltsev
St. Petersburg Medical Academy of Postgraduate Education, Institute of Osteopathic Medicine, Russia
D.V. Ivanov
St. Petersburg State University, Faculty of Medicine, Institute of Osteopathy, Russia
Diagnostic measures
A neurologist may suspect the presence of an intracranial formation of significant size based on the patient’s neurological status and clinical symptoms. In this case, the patient is sent for examination to an ophthalmologist and otolaryngologist to check vision and hearing. Specialists perform ophthalmoscopy, audiometry, perimetry and visometry. With severe hydrocephalus, ophthalmoscopy reveals congested optic discs.
By referring the patient for echo-encephalography, it is possible to diagnose increased intracranial pressure. If the patient experiences epileptic paroxysms, he is additionally sent for electroencephalography.
It is extremely important to differentiate a cavity with fluid from a tumor, abscess and hematoma. It is not possible to do this on the basis of collected clinical data alone. Therefore, to make a clear diagnosis, neurologists use neuroimaging diagnostic methods.
By performing an ultrasound examination, it is possible to diagnose certain types of congenital cysts even at the stage of intrauterine development of the fetus. After birth, until the baby's large fontanelle closes, neurosonography is performed to make the correct diagnosis. In adulthood, to visualize a brain cyst, the patient is sent to a magnetic resonance or computed tomography scan of the head.
MRI and CT are performed with contrast in order to differentiate a cyst from a tumor. A cavity with liquid is not able to accumulate a contrast agent, unlike a tumor.
After diagnosis, constant monitoring of the patient with a cystic formation is important. During regular examinations, the doctor monitors the volume of the cyst over time.
If the cyst is a consequence of a stroke, additional vascular examinations are carried out: ultrasound, MRI and CT of vessels, duplex scanning.
Second opinion for arachnoid cyst
Despite the fact that MRI diagnostics using a contrast agent provides the doctor with the necessary information, there is still a risk of error. It is associated primarily with the doctor’s lack of residual experience in interpreting MRI results and identifying cysts. Not a single patient is immune from such errors, and they happen both in large cities and in small towns. In this situation, the only way to eliminate an error or at least significantly reduce its likelihood is to obtain a second opinion from a highly qualified specialist
The National Teleradiological Network (NTRS) offers you the opportunity to receive consultations from the country's leading specialists in the field of MRI diagnostics, who have extensive experience in analyzing tomographic images of various diseases. To get a consultation, you just need to upload the scan results to our server and within a day you will receive an alternative opinion to the opinion of your doctor.
Perhaps it will be the same as the first medical opinion, perhaps it will differ from it, but the second opinion will definitely allow you to reduce the risk of misdiagnosis and incorrect treatment to almost zero.
General principles of therapy
Drug therapy for cystic formations has practically no results. The only possible treatment is surgical removal of the fluid cavity. But, most forms are small in size and remain in a “dormant” state for many years. In this case, no methods of therapy are used; a wait-and-see regimen is chosen and the patient is regularly examined.
Formations that are accompanied by symptoms of hydrocephalus, complicated by bleeding and rupture, compressing the brain and rapidly increasing in size must be removed. Only a neurosurgeon decides which method of surgical treatment to use.
If the patient has a disorder of consciousness (coma or stupor), he is urgently referred to external ventricular drainage. This method allows you to reduce compression of the brain by the cyst and intracranial pressure. If the cyst ruptures or hemorrhages, surgery is performed. The patient undergoes craniotomy and the formation is excised.
In the absence of complications and disturbances of consciousness, the operation is performed planned and endoscopically. The advantage is the patient’s quick recovery period and low trauma. With endoscopic access, a milling hole is made in the skull, through which fluid is sucked out from the cavity. In order to avoid subsequent accumulation of fluid, several holes are made in the cavity (connected to the cerebrospinal fluid space) or cystoperiotoneal shunting is performed (a special shunt is installed).
The postoperative period involves rehabilitation therapy, including exercise therapy, reflexology and massage. The patient is prescribed drugs to improve blood supply to the brain, absorbents and decongestants.
Forecasts
In most cases, a frozen cavity with liquid of insignificant size does not bother the patient and does not cause any symptoms. In other cases, with adequate and timely treatment, the outcome is favorable.
In rare cases, patients after surgical removal of a cyst experience a residual moderate-to-severe liquor-hypertensive symptom. If a focal neurological deficit develops, it persists after treatment.
With the removal of the cyst, epileptic paroxysms disappear, but often appear later. This is justified by changes in the operated area of the head, in particular the formed adhesions. Secondary epilepsy is practically uncontrollable by anticonvulsant therapy.
Prevention
An acquired cyst most often becomes a consequence of developing inflammatory, vascular, infectious and post-traumatic processes. Therefore, it is absolutely obvious that only correct and timely treatment of any pathologies, including resorption and neuroprotective therapy, can serve as a preventive measure for the development of formations in the brain.
The only measure to prevent congenital cysts is to protect the woman and fetus from exposure to provoking factors. Equally important are correct management of pregnancy and delivery.
Diagnostic methods
The difficulty in identifying the disease is that the symptoms are largely similar to those of other diseases. In the case of a cyst in a child, especially an infant, it is not possible to identify it based on a simple survey. Modern examination methods are designed to ensure diagnostic accuracy. MRI of the brain, ultrasound, computed tomography, electroencephalography, echo and rheoencephalography are performed. The most informative method in making an accurate diagnosis is MRI - magnetic resonance imaging. With its help, the doctor can not only determine the presence of a tumor, find and accurately determine its location, but also understand the nature of the tumor.