The splenic artery is a blood vessel that supplies blood to the spleen. The spleen is an organ involved in hematopoiesis and regulation of the immune system. Splenic artery aneurysm is the third most common type of aneurysm, occurring in 1% of all patients seen in vascular surgery departments. An aneurysm is defined as a local dilatation with an artery diameter of more than 10 mm.
Aneurysm of the splenic artery is a great danger, which lies in the possibility of its rupture with profuse bleeding and death of the patient. An established diagnosis of a splenic aneurysm is an indication for surgical intervention to eliminate it, since it is extremely rare to save a patient with a ruptured aneurysm.
What is an aneurysm
The splenic artery lies along or behind the upper edge of the pancreas and splits into small vessels at the hilum of the spleen. When an aneurysm occurs, its pathological expansion occurs under the influence of a number of internal and external factors:
- multiple pregnancy;
- pancreatic diseases;
- periarteritis nodosa (inflammation of the artery wall);
- lupus erythematosus;
- various injuries;
- vascular pathologies of the liver.
The risk of developing a pancreatic or splenic aneurysm increases after age 50. The disease is diagnosed more often in women than in men, especially in the presence of complications during pregnancy.
Symptoms of the disease
In most cases, the disease is asymptomatic. Patients learn about a saccular aneurysm of the splenic artery and what it is by chance as a result of examining nearby organs. Signs of pathology may include abdominal pain, nausea and vomiting. With large aneurysms, people of thin build experience negative sensations in the left hypochondrium.
The disease can remain latent for a long time. If a rupture occurs, heavy internal bleeding makes itself felt by pale skin, general weakness, decreased blood pressure and pulse rate, and the appearance of sticky cold sweat. Palpation reveals abdominal pain.
Causes
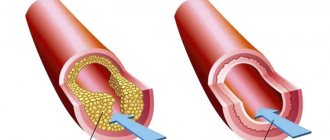
A pathology such as a vessel aneurysm occurs when the vascular wall is weakened and deformed under blood pressure. There are several reasons for the appearance of aneurysms. The disease can occur due to the following factors:
- Atherosclerosis of blood vessels, which weakens the vascular walls.
- High blood pressure.
- Various tumors and serious injuries.
- An aneurysm can also occur as a result of genetic changes: failures in the formation of connective tissue, congenital circulatory pathologies.
In what cases is surgery necessary?
More often, treatment is performed surgically. It is necessary when the diameter of the aneurysm reaches 5-6 cm. In this case, the risk of rupture increases significantly. The choice of technique is made by the doctor, taking into account a number of factors.
Methods for treating splenic artery aneurysm:
- Aneurysmorrhaphy. The method is used when the aneurysm is localized in the distal part of the artery and involves suturing the aneurysmal sac.
- Aneurysm resection with splenectomy. Elimination of the pathological section of the artery occurs with subsequent removal of the spleen. The surgical operation is performed openly or using laparoscopy (manipulations are performed through microincisions using a laparoscope equipped with a video camera and microinstruments).
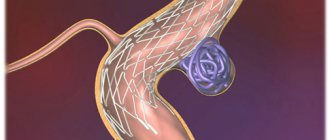
- Embolization with coils. This is a modern high-tech method of treating aneurysms. The goal of surgery is to stop blood flow in the aneurysm sac by inserting a coil. The latter is implanted through a microcatheter.
- Stenting. The task during the operation is similar to the previous method - exclusion of the pathological vessel from the bloodstream. A stent graft (tube-shaped prosthesis) is implanted into the artery through a microcatheter. After its installation, the direction of blood flow changes, and the aneurysm thromboses over time. The aneurysmal sac is isolated from the circulatory system after surgery, so the risk of rupture and bleeding is eliminated.
Stenting and embolization of splenic artery aneurysm are the most modern minimally invasive surgical methods. When the operation is planned, they guarantee a favorable prognosis.
Splenic artery aneurysm (SAA) was described by M. Beaussier in 1770. According to autopsies, during a special examination of the splenic artery, aneurysms were found in 10% of cases [1], which indicates their often asymptomatic existence. ASAs measuring 5 cm or more are considered gigantic [2–5], and by 2005, only 18 cases of such aneurysms were described [5]. By 2015, an analysis of electronic databases had already found 69 publications, which reported on 78 patients with ASA larger than 5 cm [2]. The source of literature [6] describes a giant ASA measuring 30×20×20 cm. Thanks to the widespread use of modern diagnostic methods, ASA is increasingly being detected intravitally. Nevertheless, aneurysms of this localization, including giant ones, as a rule, turn out to be accidental findings during instrumental examinations, as well as during surgical interventions performed for completely different indications. In addition to true ACA, the wall of which has 3 vascular layers, there are also false aneurysms, their structure lacks one or two vascular layers (usually adventitia). Damage to the wall of the splenic artery during pancreatitis can lead to the formation of pseudoaneurysms [7], which must be taken into account when managing such patients [8]. In addition to pancreatitis, factors contributing to the formation of ASA may be portal hypertension, atherosclerosis, connective tissue diseases, trauma, multiple pregnancies, septic conditions, and liver transplantation [5, 9–11].
ACAs, especially those of small size, can remain asymptomatic for many years [2], but when they suddenly rupture, life-threatening bleeding occurs in the abdominal cavity, retroperitoneal space, stomach [12, 13], intestinal loops [14, 15], and pancreas and Wirsung duct [2, 16, 17]. Spontaneous ruptures occur in 2-10% of patients, more often with giant (up to 28%) and pseudoaneurysms (up to 37%), with a mortality rate reaching 40% [2].
Treatment of ASA is surgical. Open interventions include aneurysmectomy, including with concomitant splenectomy, and ligation of the splenic artery. Often the scope of surgical intervention has to be expanded to include organs adjacent to the ASA, such as the pancreas, large intestine, and stomach, which significantly complicates the operation [2, 4, 13, 16, 18]. In some cases, for these reasons, as well as due to the serious condition of the patient or the presence of serious concomitant diseases, open intervention may be impossible or very dangerous.
Recently, percutaneous endovascular interventions are increasingly used to treat ASA: embolization of the aneurysm cavity and/or proximal segment of the splenic artery using special coils or embolic agents (ethylene-vinyl-alcohol-copolymer, N-butyl-2-cyanoacrylate), blocking the mouth aneurysm using a stent graft, injection of thrombin into the aneurysm cavity. The choice of endovascular technique depends on the size of the aneurysm, the state of its mouth (narrow or wide), its location along the splenic artery, the presence of certain embolic agents, and previous experience with subfrontal interventions [3, 19—23].
We present two clinical observations of patients with large ASA, in whose treatment transcatheter proximal embolization of the splenic artery was successfully used.
Sick Yu
., 62 years old, in 2011, when performing a spiral computed tomography (SCT) of the coronary arteries, the upper parts of the abdominal cavity and retroperitoneal space were captured in the field of view of the tomograph. In the adrenal glands, formations measuring 2x3 and 4x2.5 cm were found, which upon further examination turned out to be benign tumors without hormonal activity, and in the area of the body of the pancreas, a formation measuring 4.5x4 cm was also accidentally discovered (Fig. 1),
Rice.
1. Spiral computed tomogram of the splenic artery of patient Yu., 2011. Aneurysm 4.5×4.0 cm (indicated by an arrow). which was interpreted as a pancreatic cyst. After 1 year, an ultrasound of the hepatobiliary zone in the projection of the pancreas also revealed a liquid formation measuring 4.4×4.1×4.8 cm with a heterogeneous structure, without signs of blood flow on color Doppler mapping (CDC), also regarded as a cyst. At the end of 2015, the patient was hospitalized due to a hypertensive crisis in the cardiology department and underwent a CT scan to evaluate adrenal tumors identified in 2011, the size and structure of which remained unchanged. The presence of a mass in the area of the body of the pancreas was also confirmed. The use of a contrast technique clarified the nature of this formation - ASA, the size of which increased over 4 years to 5.1 × 6.3 × 6.2 cm. In the parietal region of the aneurysm, thrombotic masses with calcium inclusions were determined, the size of the non-thrombosed part of the cavity was 4.1 × 4.7×5.2 cm. Three-dimensional reconstruction clearly identified the proximal afferent and distal efferent segments of the splenic artery (Fig. 2 and 3).
Rice. 2. Spiral computed tomogram of the splenic artery of patient Yu., 2015, contrast enhancement. Aneurysm 6.3×6.2 cm (indicated by arrow).
Rice. 3. Spiral computed tomogram of the splenic artery of patient Yu., 2015, contrast enhancement, 3D reconstruction. 1 — aneurysm 5.1×6.3×6.2 cm, 2 — afferent segment of the splenic artery, 3 — efferent segment of the splenic artery. The body of the pancreas, compressed by the aneurysm, was thinned, and the Wirsung duct was expanded to 5 mm. The patient was consulted by a surgeon, who concluded that there is a high risk of complications if open surgery is used due to the location of the aneurysm and its close contact with the pancreatic tissue.
On 02/24/16, the patient was hospitalized at Regional Clinical Hospital No. 2 of Khabarovsk for routine angiography, which confirmed the presence of a large ASA measuring 6x6 cm, located closer to the aorta, without a clearly defined neck (Fig. 4).
Rice. 4. Angiogram of the splenic artery of patient Yu. dated 02.24.16. Aneurysm 6x6 cm (indicated by arrow). A decision was made on the need for endovascular embolization of the proximal segment of the splenic artery due to the large size of the aneurysm and its dynamic increase, which determined the high risk of rupture. On August 24, 2016, the patient underwent selective catheterization of the splenic artery with sequential embolization of its proximal segment with detachable mini-spirals of SOOK measuring 15×15, 10×8, 8×5 mm. Control angiography showed a significant slowdown in contrast enhancement of the aneurysm cavity (Fig. 5).
Rice. 5. Angiogram of the splenic artery of patient Yu. dated 08/24/16. 1 — the proximal segment is embolized with mini-coils of SOOK, 2 — mini-coils in the lumen of the aneurysm, blood flow in the aneurysm is reduced.
On the 3rd day after endovascular embolization, a control SCT was performed: the aneurysm is completely thrombosed, there is no accumulation of contrast agent, mini-coils are located in the lumen of the segments of the splenic artery (Fig. 6).
Rice. 6. Spiral computed tomogram of the splenic artery of patient Yu., 08/26/16, contrast enhancement. 1 — aneurysm is filled with thrombotic masses, there is no blood flow in it, 2 — embolizing mini-coils in the proximal segment of the splenic artery.
The postoperative period was uneventful, and the patient was discharged home on the 8th day. During control SCT after 5 months, the aneurysm cavity remains completely thrombosed, the proximal segment of the splenic artery is filled with embolic coils.
Patient R
., 34 years old, was admitted to the surgical department on March 11, 2018 with a complaint of severe weakness and bloody vomiting. History of chronic hepatitis of mixed etiology (HCV infection and alcohol abuse), associated with liver cirrhosis, class C according to the Child-Pugh classification, portal hypertension, ascites, splenomegaly. In 2006, she was operated on for a penetrating stab wound to the abdominal cavity. Upon admission, the condition was serious, the skin was pale, pulse 114 per minute, blood pressure 60/40 mm Hg. Esophagogastroscopy revealed an ulcer of the lower third of the esophagus without signs of ongoing bleeding. Hemostatic therapy was carried out (transfusion of red blood cells, fresh frozen plasma), during which the condition improved and hemodynamics stabilized. On March 13, 2018, an ultrasound scan revealed a liquid formation of 6.7×7.5 cm with thick walls in the projection of the head of the pancreas. After 3 days, repeated echography revealed an increase in its size to 8.2×7.1 cm. On March 21, 2018, the patient underwent surgery: laparotomy, gastrotomy, and gastric revision. Deformation of the posterior wall of the stomach was discovered due to a pulsating tumor-like formation in the omental bursa, during puncture of which arterial blood was obtained through the posterior wall of the stomach. The defect in the puncture area is sutured with interrupted sutures. Intraoperative Doppler ultrasound was performed and arterial (pulsating) blood flow into the lumen of the formation was detected. It was decided to complete the operation by suturing the body of the stomach and draining the abdominal cavity. On 03/23/18, a contrast-enhanced examination of the abdominal cavity was performed, revealing a partially thrombosed saccular aneurysm (probably a pseudoaneurysm) of the splenic artery measuring 7.8×5.7 cm (Fig. 7).
Rice. 7. Spiral computed tomogram of the splenic artery of patient R., contrast enhancement. Partially thrombosed aneurysm 7.8×5.7 cm (indicated by arrow). Due to the large size of the aneurysm, which increased dynamically over 3 days, which created a high risk of rupture, a decision was made on endovascular surgical intervention. On 03/28/18, the patient underwent catheterization of the right femoral artery and angiography of the celiac trunk, which confirmed the diagnosis of splenic artery aneurysm (Fig. 8).
Rice. 8. Angiogram of the splenic artery of patient R. Contrast in the cavity of the aneurysm (indicated by the arrow). A stent graft was installed in the area of the aneurysm neck. On the control angiogram, the filling of the aneurysm with blood flow remained. Embolization of the splenic artery was performed with 0.035" detachable peripheral coils. During installation of the coils, the stent graft dislocated into the distal part of the splenic artery. The control angiogram showed a decrease in blood flow in the area of the aneurysm (Fig. 9).
Rice. 9. Angiogram of the splenic artery of patient R. The proximal part is embolized with coils (indicated by an arrow), blood flow in the aneurysm is reduced. On the 5th day after endovascular intervention, a control SCT with contrast enhancement was performed: parietal thrombosis of the splenic artery from the mouth in the embolization zone, absence of contrast accumulation in the aneurysm, heterogeneity of its contents, and signs of aneurysm thrombosis were noted (Fig. 10).
Rice.
10. Spiral computed tomogram of the splenic artery of patient R., contrast enhancement, 5 days after endovascular intervention. Thrombosis in the area of embolization with coils (indicated by an arrow). There is no blood flow in the aneurysm, its cavity is thrombosed. On 04/09/18, the patient was discharged on the 12th day after endovascular intervention in satisfactory condition. Observed in the clinic at the place of residence. Our first observation confirms that even fairly large ASAs can be asymptomatic and turn out to be an incidental finding during examination or surgical operations for other indications. In the second case, the clinical picture of gastric bleeding with bloody vomiting and hemorrhagic shock did not exclude a possible breakthrough of a pseudoaneurysm through the posterior wall of the stomach. In both cases, upon initial examination, the aneurysms were regarded as pancreatic cysts. Therefore, it seems advisable, when identifying such formations that are large in size and especially signs of vascularization during echography with color Doppler mapping, to perform multislice CT with contrast enhancement, which makes it possible to accurately establish the diagnosis of ASA.
The need for surgical treatment in the above observations is dictated not only by the large size of the aneurysms, but also by the fact that their size increased over time (in the second case very quickly, within 3 days), which created a very high risk of rupture. There is evidence that blocking giant ASAs with a stent graft may be ineffective due to its prolapse and subsequent migration into the aneurysm cavity through a wide orifice, which also complicates the passage of the stent graft into the segment of the splenic artery distal to the aneurysm [20] . In our observations, embolization of the proximal part of the splenic artery turned out to be effective. It is also important that the use of this technique allows you to preserve the spleen, the blood supply of which continues to be carried out through short gastric, gastroepiploic and pancreatic collaterals. Another advantage of endovascular methods for treating ASA is the possibility of their use in situations where open surgical intervention is impossible or is associated with a high operational risk, due to both the anatomical features of the location of the aneurysm and the patient’s condition.
The authors declare no conflict of interest.
*e-mail
Treatment at home
Timely diagnosis provides a chance to slow down the progression of the disease with the help of medications. Radiation diagnostics provides the greatest information in case of splenic aneurysm. It includes:
- Angiography (x-ray examination of arteries and veins). The method allows you to identify the localization of pathological expansion and the presence of internal bleeding. Diagnosis is carried out by injecting a contrast agent into the vessel and simultaneously examining the artery with an X-ray machine.
- Radiography. Diagnosis is also carried out using x-rays, but using special paper to obtain a projected image of anatomical structures.
- CT and MRI. These methods play an important role in differential diagnosis and allow us to establish the exact location of the aneurysm.
- Ultrasound with Doppler. The diagnostic method makes it possible to examine the blood supply to organs and, based on the data obtained, determine the presence of pathology.
Instrumental diagnostics allows one to accurately determine the location of the pathology and the degree of risk of complications in the patient. If a small aneurysm is detected at an early stage, drug therapy is possible under constant medical supervision.
It includes taking beta blockers, drugs prescribed for hypertension, high cholesterol. Medicines slow the growth of an aneurysm, but cannot completely cure it. The patient can take the medications at home. If injection administration is required, outpatient treatment is possible.
Diagnosis of aneurysm
In our department of vascular surgery, experienced phlebologists perform high-quality diagnostics of all forms of aneurysms using modern instrumental techniques:
· ventriculography and angiography are invasive research methods that involve the introduction of contrast into the blood vessels in the affected area. Such studies can detect vascular aneurysms, their dissection, signs of rupture or thrombosis;
· ECHO of the heart, ultrasound of the arteries – used to diagnose aneurysms located outside the brain;
· Ultrasound examination of blood vessels, Dopplerography;
· CT with contrast - allows you to identify signs of aneurysm dissection.
Signs of bleeding or arterial thrombosis can also be detected by laboratory blood tests.
Prevention of splenic aortic aneurysm
Patients who are at risk are advised to follow a number of recommendations:
- eat less animal fats and enrich your diet with vegetables and fruits;
- keep cholesterol levels under control with blood tests;
- give up cigarettes and alcoholic drinks;
- lead a healthy lifestyle;
- keep blood pressure levels under control;
- If suspicious symptoms appear, consult a doctor;
- perform a preventive ultrasound of the abdominal organs.
Since the mortality rate for aneurysm is 40-50%, timely prevention will avoid serious complications and prevent vessel rupture.
Still have questions about splenic artery aneurysm?
Free consultation with AngioClinic specialists
Author
Salmina Daria Vladimirovna
Geneticist. Graduated from the Chelyabinsk State Medical Academy. She completed an internship at the Northwestern State Medical University named after I.I. Mechnikov.