DlyaSerdca → Heart diseases → Other diseases → Inflammation of the lining of the heart: pericarditis
The pericardium (pericardial sac, cardiac sac) is a closed organ that surrounds the heart on all sides. It consists of two layers: the visceral (epicardium) is fused with the heart muscle and completely covers it, and the parietal (pericardium itself), consisting of two layers, is the outer layer. Between the sheets of the pericardium there is a slit-like space normally containing 15-30 ml of pericardial fluid.
Functions of the pericardium
The outer layer of the pericardium is attached in front to the sternopericardial ligament, from below to the diaphragm, on the sides to the parietal pleura, and behind to the vertebral-pericardial ligaments.
Its main function is to hold the heart in a certain position and protect it from injury when changing body position.
Negative pressure is maintained in the slit-like space, which helps straighten the chambers of the heart and fill them with blood. In addition, pericardial fluid is a lubricant that reduces friction of the heart. The pericardium also protects the heart from infections.
External structure of the heart
Types of disease
The clinical course and severity of pericarditis is determined by the amount and nature of the effusion and the speed of development of the disease.
There are acute pericarditis (less than 1.5 months), subacute (from 6 weeks to 6 months) and chronic (more than six months).
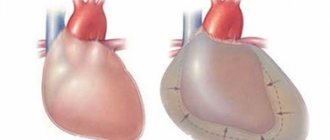
Based on the amount of effusion, dry (fibrinous) and exudative pericarditis are distinguished. With dry pericarditis, most of the inflammatory fluid is absorbed, leaving a protein - fibrin - in the cavity. It can accumulate focally, or be evenly distributed throughout the heart sac, creating a condition described as a “hairy heart.”
Fibrinous
Exudative
Dry
Effusion with exudative pericarditis can be:
- Serous - the liquid contains little protein and formed blood elements; upon recovery, it is completely absorbed without leaving a trace; in rare cases, insoluble calcium salts remain, and an “armored heart” is formed.
- Fibrinous - contains a lot of fibrin protein, leaves adhesions.
- Serous-fibrinous - something between the first two.
- Hemorrhagic - containing red blood cells due to injury or tuberculosis.
- Purulent – contains bacteria and neutrophils.
- Putrefactive - contains anaerobic bacteria and neutrophils.
Exudative pericarditis
Symptoms and diagnosis
Pericarditis very rarely develops as an independent disease, more often as a complication of general diseases. Pericarditis is characterized by a slight increase in body temperature. Intense pain in the chest, which in its strength and intensity resembles the pain of angina pectoris or myocardial infarction, but lasts longer.
Painful sensations are not associated with physical activity; they may intensify when inhaling, swallowing, or changing body position.
The pain is sharply aggravated by pressing on the xiphoid process of the sternum and the sternoclavicular joint. Taking nitrates does not relieve attacks of pain. Rhythm disturbances and the development of atrial fibrillation are possible. On auscultation, a friction rub of the pericardium is heard both in systole and in diastole, which significantly increases with pressure on the chest.
Xiphoid process of the sternum
With exudative pericarditis, the symptoms of cardiac tamponade come to the fore. The greater and lesser vena cava swell, the pulse quickens and becomes paradoxical (the pulse disappears on inspiration).
Patients are cyanotic, experience a feeling of lack of air, fear of death, and loss of consciousness. Patients develop stagnation of blood in the systemic circulation, edema develops, and patients experience heart failure. When the enlarged pericardium puts pressure on the phrenic nerve, patients begin to experience hiccups and uncontrollable vomiting.
Patients with exudative pericarditis take a forced position in which they experience the least pain and nausea, bend forward and lean on their hands, and take a knee-elbow position.
As an outcome of tuberculous, purulent and hemorrhagic pericarditis, the development of constrictive pericarditis with the development of Beck's triad is possible: swelling of the jugular veins, ascites, a “quiet” heart with a negative apical impulse. The diagnosis of pericarditis can be refuted or confirmed by ultrasound of the heart.
MACRO PREPARATION No. 18. Fibrinous pericarditis
Page 1 of 3Next ⇒
MACRO PREPARATION No. 18. Fibrinous pericarditis
1. heart
2. the organ is enlarged in size, exudate of loose consistency is localized on the outer layer of the pericardium. The pericardium is dull, covered with rough, grayish-yellow thread-like deposits and very vaguely resembles hair. The overlays are easy to remove.
3. Fibrinous pericarditis (hairy heart)
4. the outcome is unfavorable. Due to the germination of deposited fibrin masses by fibroblasts, adhesions are formed between the layers of the pericardium, which leads to obliteration of the pericardial cavity. Sometimes sclerotic membranes petrify with the formation of an armored heart, which leads to impaired contractility.
5. causes - infectious agents, sublimate poisoning, uremia, inflammatory processes, myocardial infarction
MACRO PREPARATION No. 21. Cardiac hypertrophy
1. heart (cross section through the ventricles)
2. the size of the organ is almost not increased. The wall of the left ventricle is thickened due to concentric narrowing of the cavity. Swollen papillary muscles are clearly visible
3. Cardiac hypertrophy (compensatory, working (tonogenic), concentric)
4. the outcome is favorable (the work of the heart is compensated) complications - some of the cells die, dilated hypertrophy (decompensation) develops - chronic heart failure, hemodynamic disorders, congestion in the BCC, development of bovine heart
5. Cardiac forms of hypertension, aortic valve insufficiency, excessive long-term and emotional stress
MACRO PREPARATION No. 26. Brown myocardial atrophy
1. Heart
2. the organ is reduced in size, there is no subepicardial fatty tissue, the coronary vessels have a pronounced tortuous course, the color of the heart muscle on the section is yellow-brown
3. Brown myocardial atrophy
4. Unfavorable outcome – chronic HF
5. reasons - cachexia, vitamin E deficiency, drug intoxication, increased functional load, debilitating diseases
MACRO PREPARATION No. 28. Gangrene of the small intestine
1. part of the small intestine with mesentery
2. the wall is edematous, thickened, dark brown in color, the intestinal lumen is sharply narrowed. In the lumen of the mesenteric vessels there are thrombotic masses
3. Wet gangrene of the small intestine
4. the outcome is favorable if a small area of the intestine is damaged à resection. But more often unfavorable à perforation with peritonitis
5. causes - thrombosis of the mesenteric arteries and their embolism
MACRO PREPARATION No. 32. PE
1. heart, place of bifurcation of the pulmonary trunk
2. In the main trunk of the pulmonary artery, worm-shaped, dryish gray-red masses are visible. They fill the lumen of the vessel, but are not associated with the intima.
3. TELA
4. the outcome is unfavorable; sudden death due to the development of pulmonary-cardiac and pulmonary-coronary reflex à spasm of the coronary arteries; pulmonary-pulmonary reflex à spasm of the pulmonary arteries and bronchi à respiratory and heart failure à death
5. causes - thrombosis of the veins of the lower extremities, pelvis, hemorrhoidal plexus, formation of a blood clot in the right half of the heart and from the vena cava system
MACRO PREPARATION No. 48. Subarachnoid bleeding
1. Brain
2. in the temporal region of the right hemisphere in the base area there is a lamellar hemorrhage 7 x 5 cm with clear boundaries of a dark burgundy color. The convolutions and furrows are smoothed.
3. Subarachnoid hemorrhage
4. relatively unfavorable outcome: development of edema, compression, dislocation of the brain à hypoxia à death of the cortex
5. Hypertension, atherosclerosis, leukemia, trauma, aneurysm
MACRO PREPARATION No. 172. Lipoma
1. adipose tissue (tumor tissue)
2. tumor node of dense elastic consistency in a capsule, with a diameter of about 10 cm, on a section it has a lobed structure, yellow color, greasy appearance
3. lipoma
4. outcomes are different, most often favorable. Complications: malignancy, compression of surrounding tissue
5. reasons are polyetiological
ELECTROGRAM 7. Sarcoma
1. Tumor cell
2. Large, irregularly shaped nuclei with uneven distribution of chromatin along the periphery and an increased number of nucleoli
3. see point 2
4. see point 3
5. Sarcoma
7. ELECTROGRAM 8. Myocardial hypertrophy in the stage of decompensation
1. Myocardium
2. Destruction of giant mitochondria with destruction of cristae, outer membranes, leaching of the matrix. A drop of lipids is located in close contact with the destroyed organelles. Myofibril ruptures in the disc area are visible; glycogen granules and ribosomes are absent
3. see point 2
4. see point 3
5. Myocardial hypertrophy in the compensation stage
MACRO PREPARATION No. 18. Fibrinous pericarditis
1. heart
2. the organ is enlarged in size, exudate of loose consistency is localized on the outer layer of the pericardium. The pericardium is dull, covered with rough, grayish-yellow thread-like deposits and very vaguely resembles hair. The overlays are easy to remove.
3. Fibrinous pericarditis (hairy heart)
4. the outcome is unfavorable. Due to the germination of deposited fibrin masses by fibroblasts, adhesions are formed between the layers of the pericardium, which leads to obliteration of the pericardial cavity. Sometimes sclerotic membranes petrify with the formation of an armored heart, which leads to impaired contractility.
5. causes - infectious agents, sublimate poisoning, uremia, inflammatory processes, myocardial infarction
1Next ⇒
Recommended pages:
Treatment of the disease
Treatment for pericarditis varies depending on what caused it.
For rheumatic, allergic, autoimmune pericarditis, steroidal anti-inflammatory drugs are prescribed; their combination with immunosuppressive drugs is possible.
For purulent pericarditis, antibiotic therapy is carried out depending on the sensitivity of the pathogen. For parasitic pericarditis, anthelmintic drugs are prescribed.
The development of cardiac tamponade is an indication for pericardial puncture and evacuation of its contents. Pericardial puncture must be performed very carefully, under X-ray or ultrasound guidance, to exclude the possibility of heart injury. Pericardiocentesis is not recommended for small effusions when the pericardial layers are less than 1 cm apart.
Cardiac tamponade
Transcutaneous balloon pericardiotomy is the operation of choice when there is a large volume of fluid in the pericardium and when constant drainage of the pericardium is necessary. The operation is performed under local anesthesia, a balloon is inserted through a rigid catheter to widen the hole in the pericardium, and a catheter is installed for constant evacuation of the contents of the heart sac cavity.
The operation is low-traumatic and safe. Good experience in the use of pleural fenestration - a small window (fenestra) is made in the pericardial cavity, which is sutured to the pleural cavity. The pleura has a large surface area, through which excess fluid is absorbed.
Surgery is the only possible treatment for constrictive (adhesive) pericarditis to remove adhesions and allow the heart to contract normally. Surgical treatment is also recommended for purulent pericarditis and serious circulatory disorders.
For edema, diuretics are prescribed, which can reduce the volume of fluid in the cavity of the heart sac. Syndromic therapy is carried out depending on the complications that have developed (restoring the rhythm, eliminating cardiac and respiratory failure, etc.) Pericarditis is a terrible disease that leads to death.
Pericarditis
Pericarditis is an inflammatory disease of the tissue lining of the heart (pericardium), of an infectious or non-infectious nature.
The pericardium consists of outer and inner layers, between which normally there is a small amount of fluid. Fluid is needed to ease friction during contraction of the heart muscle. Pericarditis can act as an independent isolated disease or be a complication of diseases of other organs and systems.
Causes of pericarditis development
- infectious (bacteria, viruses, fungi, protozoa, etc.),
- non-infectious (allergic diseases, systemic connective tissue diseases, some blood diseases, metabolic disorders, injuries, exposure to radiation, treatment with certain hormonal drugs, cancer).
There are idiopathic pericarditis (cases of pericarditis where the cause of inflammation cannot be determined). In the development of pericarditis, changes in the composition or amount of pericardial fluid under the influence of the above factors play an important role.
Symptoms of pericarditis Symptoms of pericarditis are cardiac and general, the degree and severity of symptoms depend on the form and stage of the disease. The main cardiac symptom is heart pain, felt in 90% of cases. The pain is usually localized behind the sternum or in the left half of the chest, and can radiate to the left arm. The intensity of pain varies: from almost imperceptible to extremely acute, heart attack-like. The nature and intensity of pain varies depending on the position of the body. The pain decreases when lying on the right side with the legs pulled up to the chest, or when bending forward. This happens because in this position, when the heart contracts, the inflamed walls of the heart sac come into less contact. The pain intensifies when coughing, taking a deep breath, or lying on your back. With some types of pericarditis there may be no pain at all. Another common symptom is the appearance of circulatory failure (shortness of breath on exertion and at rest, edema). Common symptoms include:
- weakness;
- sweating;
- fatigue, lack of or decreased appetite;
- elevated temperature.
If pericarditis has developed as a complication of another disease, symptoms of damage to other organs and systems may be present in the foreground.
Types and forms of pericarditis
- Acute pericarditis – up to 1-2 months from the onset of the disease. Types of acute pericarditis: exudative (effusive), fibrinous (dry).
- Subacute pericarditis – from 2 to 6 months from the onset of the disease. Types of subacute pericarditis: exudative (effusion); adhesive (sticky); constrictive (squeezing).
- Chronic pericarditis – more than 6 months from the onset of the disease. Types of chronic pericarditis: exudative (effusion); adhesive (sticky); constrictive (squeezing); compressive pericarditis with calcification (“shell heart”).
Exudative pericarditis. As a result of the inflammatory process, a large amount of fluid accumulates in the pericardial cavity. The fluid may contain various cellular elements and substances, depending on their presence, exudative pericarditis is divided into several subtypes (purulent, hemorrhagic, uremic, etc.). If the effusion accumulates very quickly, the outer layer of the pericardium does not have time to stretch, compression of the heart chambers occurs, cardiac output drops sharply, and acute cardiovascular failure develops. This process is called cardiac tamponade. Cardiac tamponade is a life-threatening condition that requires emergency hospitalization and treatment. If fluid accumulates slowly in the pericardial cavity, the outer layer of the pericardium has time to stretch, without compression of the walls of the heart and disruption of its functioning. More than 1 liter of fluid can accumulate in the pericardial cavity. An enlarged cardiac sac sometimes interferes with the normal functioning of nearby organs (esophagus, trachea, lungs, recurrent nerve), which is manifested by swallowing disorders, cough, hoarseness and other symptoms.
Fibrinous pericarditis. Fluid (inflammatory effusion) containing fibrinogen forms in the pericardial cavity. Some of the fluid is sucked out through the lymphatic vessels, but fibrin fibers settle on the leaves of the cardiac sac, limiting their movement.
Adhesive pericarditis. With adhesive pericarditis, as a result of the inflammatory process, connective tissue grows on the pericardial layers, forming adhesions.
Constrictive pericarditis. With constrictive pericarditis, as a result of the inflammatory process, the entire cavity of the heart sac is filled with scar tissue, causing compression of the heart chambers and impairing the function of the heart.
Compressive pericarditis with calcification (“shell heart”). With an “armored” heart, as a result of the inflammatory process, the pericardial layers become denser, welded together, and calcium is deposited in them. A rigid and inactive cardiac sac disrupts the functioning of the heart.
Diagnosis and treatment of pericarditis Pericarditis is a very “cunning” disease, due to its non-specific, in the eyes of a layman, symptoms and “disguise” as some other diseases.
If pericarditis is suspected, consultation with a cardiologist is mandatory. With asymptomatic or minimally symptomatic pericarditis, diagnosing the disease is difficult. The key to correct and effective treatment is high-quality diagnostics. It is very important to carry out all the necessary research as quickly as possible. You may need:
- blood test (clinical, biochemical, immunological) – whether there are signs of inflammation in the blood;
- ECHO KG (ultrasound of the heart) - the amount of fluid in the pericardial cavity is visible;
- ECG;
- radiography;
- CT scan of the chest;
- in some cases, diagnostic puncture or biopsy of the pericardium.
Additional tests are often prescribed to clarify the causes of pericarditis. Only an experienced doctor can correctly interpret the examination results and develop a treatment regimen. With proper, timely treatment, the prognosis is usually favorable. Treatment methods for pericarditis are very different and depend on its nature, course, and concomitant diseases. Treatment can be either medicinal or surgical (pericardial puncture, pericardial biopsy, surgical treatment of scars).
Traditional methods of treatment
Do not self-medicate, seek medical help.
Among the traditional methods, taking diuretics at the same time as taking medications is effective and acceptable.
A decoction of lingonberry leaves and bearberry leaves 1 to 1 is recommended as a good diuretic.
If the acute phase of pericarditis is already behind you and you are under the supervision of a doctor, to alleviate the consequences of pericarditis, you can take “Goodbye pericarditis of the heart” balm: mix 200 ml in a dark glass container with a ground-in lid. tinctures of spring adonis, birch leaves, hawthorn fruits, peony, trifoliate, add 100 ml. valerian root extract and peppermint. Add 5 tablespoons of linden honey to it. Take a tablespoon 10 minutes before meals 3 times a day.
Forecast for life and health
The prognosis for life with purulent, and especially putrefactive pericarditis is extremely unfavorable.
Even with full surgical treatment with drainage of the pericardium and mediastinum, and the use of modern intensive care reserve antibiotics, the mortality rate reaches 50% or more.
Hemorrhagic pericarditis without timely medical treatment is fatal. The most favorable prognosis for returning to a normal lifestyle is given if pericarditis is diagnosed and treated on time, and if it does not become constrictive.
Adhesive pericarditis leads to disability, however, with modern surgical treatment, patients return to work. In case of “armored heart”, frequent recurrent adhesive pericarditis, encysted effusion, a total or subtotal pericardectomy is performed.
What is pericarditis
This is a large and risky cardiac surgery, the mortality rate during the operation is 6-12%, and only 60% of patients experience improvement in hemodynamic parameters.
Acute idiopathic pericarditis, pericarditis caused by a viral infection, pericarditis in rheumatic diseases, with timely treatment, disappear without leaving a trace and do not in any way affect the quality of life and performance.
Sick Vladimir, 55 years old, does not work, is an alcoholic. Constant hiccups developed for 2 days, and the hiccups were accompanied by indomitable vomiting, which did not bring relief. He was hospitalized by ambulance to the therapeutic department of the district hospital. A diagnosis was made: Alcohol intoxication. Disturbances of water-electrolyte and acid-base balance. Detoxification and restorative therapy was carried out. After a day in the therapeutic hospital, the patient developed a clinical picture of alcoholic delirium - severe agitation, fear, auditory and visual hallucinations. A psychiatrist was called. Against the background of excitement, clinical death occurred. Full resuscitation measures carried out did not bring results.
At autopsy: edema-swelling of the brain, herniation of the brain stem into the foramen magnum. A sharply enlarged pericardium was detected, the volume of pericardial fluid was 1 liter 600 ml. The liquid is straw-yellow in color, odorless. Protein content 1.8 g/l. Blood cells (leukocytes, erythrocytes) were not detected. Pathological diagnosis: Acute idiopathic pericarditis. Acute heart failure.
Brief information: pericarditis, a complication of many diseases, is not diagnosed in a timely manner due to the lack of specific complaints and clinical manifestations, and is a pathological finding in 5% of autopsies.
So, inflammation of the membranes of the heart is a common disease, a complication of many pathological processes. Depending on the nature of the effusion and the causes that led to pericarditis, the severity of the disease varies.
Only timely medical treatment aimed at eliminating the cause of inflammation of the heart membrane can protect the patient.
Modern surgical methods of treatment in cases of purulent, voluminous and adhesive pericarditis make it possible to save life in a short period of time, restore the patient’s health and return him to his previous lifestyle. The administration of glucocorticosteroids for rheumatic and idiopathic inflammation of the cardiac membrane leads to complete recovery.
Similar articles
What is kyphosis and how to cure it?
Heart neurosis: causes, features, forms, diagnosis and treatment
Causes and diagnosis of left atrium dilatation
Condition of hypertrophic cardiomyopathy: causes, development and treatment
Author of the article:
Elena Demidova
about the author
Did you like the article?
Let us know about it -
rate
Radiation diagnosis of pericarditis of tuberculous etiology
SonoAce Ultrasound Magazine
Contains current clinical information on ultrasonography and is aimed at ultrasound doctors, published since 1996.
Introduction
Damage to the inflammatory process of the pericardium occurs in 3-6% of autopsies, i.e. it occurs relatively often, but during life it is poorly recognized even in hospital conditions. This is due to the wide variety of forms and clinical manifestations of the disease, often masked by symptoms of concomitant diseases. This diversity is presented in detail in complex classifications that reflect the etiology and clinical and morphological features of pericarditis [1].
In recent years, there has been an increase in the incidence of tuberculosis and its more severe course, which is accompanied by an increase in complications. In this case, tuberculous pericarditis is suffered by up to 1/10 patients with pulmonary tuberculosis [5]. Timely diagnosis of tuberculous pericarditis is of great importance, especially with constriction of the heart, since surgical intervention will help to radically change the prognosis.
The frequency of tuberculous pericarditis, according to pathological studies, ranges from 1.1 to 15.8% [3]. Of course, the number of actual cases of illness is greater than the number of deaths.
Tuberculosis can cause any known form of pericarditis. Clinical symptomatology depends on the course of pericarditis (acute, chronic), on the amount and nature of fluid in the pericardial lining, on complications of pericarditis and mainly on the nature of the underlying tuberculous process [5,6]. As is known, pericarditis can be the first clinical manifestation of tuberculosis and occur against the background of tuberculous damage to other organs. In the first case, pericarditis is characterized by a certain set of symptoms, in the second, it is masked by the underlying tuberculosis disease.
Radiation diagnostic methods (traditional X-ray diagnostics, ultrasound methods, computed tomography and radionuclide diagnostics) today are the main ones in identifying pathology of the cardiopulmonary system in general and the pericardium in particular. Despite the fact that recently, among the methods of radiological studies in the diagnosis of pericarditis, the emphasis has shifted towards ultrasound location, traditional X-ray diagnosis of this pathology in patients with tuberculosis has not lost its importance and still remains the primary stage (verification fluorography) [4]. In the presence of clinical manifestations and suspicion of cardiac pathology (since all patients are admitted to the hospital with already available X-ray data), a preliminary assessment of the cardiovascular system can be given using a regular plain radiograph.
The main clarifying method for diagnosing cardiac pathology in our clinic is ultrasound, which is especially effective in identifying inflammatory processes in the pericardium, allowing one to assess the movement of the pericardial layers, their echogenicity, the presence of inclusions in the pericardial fluid, and hemodynamic disorders [1, 6, 7].
Materials and methods
From January 1997 to August 2001 at the Research Institute of Phthisiopulmonology MMA named after. THEM. Sechenov examined 3224 patients, of which 1896 (58.8%) had respiratory tuberculosis. Pericardial pathology during a comprehensive examination was identified in 240 (7.4% of the total number of patients), of which 108 were diagnosed with tuberculous pericarditis (45%). Since 1997, in patients with pulmonary tuberculosis, there has been a tendency to increase the number of pericarditis: 1997. - 4.9%, 1998 - 6.4, 1999 - 7.0, 2000 - 8.2%.
Pericarditis of tuberculous etiology was observed in primary tuberculosis in 20 (18.5%) and in secondary forms in 88 (81.5%) cases. In primary tuberculosis, the course of pericarditis was acute: in 85% (15 cases) dry pericarditis and in 15% (5 cases) exudative pericarditis. In secondary forms of tuberculosis, the clinical course of pericarditis was chronic: in 90.9% (80 cases) exudative and 9.1% (8 cases) constrictive pericarditis.
In primary tuberculosis, pericarditis, emanating from the lymph glandular component of the primary complex, occurred in the case of progression of the process during the period of generalization. The pericardium was affected predominantly by the lymphogenous route, and in the genesis of pericarditis, not only the infectious, but also the allergic factor (damage to the serous membranes like polyserositis) was important.
In secondary forms of tuberculosis, pericarditis developed as toxic-allergic (serous-fibrinous or serous) in most cases during the period of exudative-caseous exacerbation of the process. In patients with pleural empyema, damage to the pericardium occurred through contact.
The main methods of radiological diagnosis of pericarditis were ultrasound and x-ray.
Research results
Analysis of the results showed that each case of tuberculous pericarditis presents great diagnostic difficulties, especially if the tuberculous lesion is limited only to the pericardium and the effusion remains small.
Example 1 illustrates the presence of acute dry pericarditis in a patient with tuberculosis of the peripheral and intrathoracic lymph nodes (Fig. 1).
A 22-year-old man was treated as an outpatient in the consultation department for 2 months. In the last 2 days, complaints have appeared of a dull, pressing pain in the heart area, intensifying with inspiration and movement; shortness of breath. The examination revealed a systole-diastolic, not associated with heart sounds, pericardial friction murmur, which was heard in the second and fourth intercostal spaces on the left. The boundaries of relative cardiac dullness have not changed.
An X-ray examination of the chest organs did not reveal focal or infiltrative changes in the lungs, the roots were structural, the shadow of the heart was not changed (Fig. 1 a).
The electrocardiogram (ECG) data also turned out to be uninformative (Fig. 1b): only moderately pronounced diffuse changes in the myocardium of the left ventricle are determined (the T wave is flattened and smoothed in all leads).
An echocardiographic (ECHOCG) study revealed hyperechoic inclusions on the internal surfaces of the pericardial layers, the absence of echo-negative space behind the anterior wall of the right ventricle, behind the posterior wall of the left ventricle and the apex; parallel anteroposterior movement of the pericardial layers; impaired diastolic function of the left ventricular myocardium (Fig. 1c, d).
Rice. 1.
A patient with dry pericarditis.
A)
X-ray of the chest organs.
b)
Electrocardiogram.
V)
Echocardiogram.
G)
Echocardiogram.
During a cardiointervalographic study using the method of R.M. Baevsky determines the hyperdiastolic variant and the tension of the compensatory forces of the body (Table 1).
Table 1
. Indicators of the cardiointervalographic study method according to R.M. Baevsky.
| Mo1 | 0,80″ | Mo2 | 0,56″ |
| Amo1 | 23% | Amo2 | 42% |
| ΔX1 | 0,44″ | ΔX2 | 0,61″ |
| IN1 | 65 USD | IN2 | 468 USD |
Results of the rhythmogram analysis: blood pressure (BP) lying 120/80, standing 110/90 mm Hg. Art. Autonomic reactivity (VR) - 7.2 c.u.
The coefficient of compensatory capabilities of the left ventricular myocardium (L), calculated according to the formula we proposed using indicators of heart rate (HR), ejection fraction (EF) and tension index (SI) to identify hidden heart failure, was equal to 10.8 conventional units (cu).
An enzyme immunoassay of blood gave a weakly positive reaction, and according to the results of the NCT test (modified by M.P. Gracheva, 1986), data on active specific inflammation were obtained.
Thus, according to echocardiography and cardiointervalography studies, the patient was diagnosed with acute dry pericarditis with the presence of latent heart failure.
Example 2 illustrates the presence of acute exudative pericarditis with signs of cardiac tamponade in a patient with bronchial tuberculosis (Fig. 2).
Rice. 2.
A patient with exudative pericarditis.
a, b)
X-rays of the chest cavity.
V)
Electrocardiogram.
G)
Echocardiogram.
d)
Echocardiogram.
e)
Echocardiogram.
A 49-year-old man was admitted to the department with complaints of increasing shortness of breath, palpitations, and pressing pain in the heart area. The face was puffy, the skin was pale, and the neck veins were swollen. From the anamnesis it was known that the patient was treated in an anti-tuberculosis dispensary for 3 weeks and was sent to the clinic to clarify the diagnosis and treatment.
A survey X-ray of the patient's chest cavity organs reflects the classic signs of exudative pericarditis (Fig. 2a): all sizes of the cardiac shadow are increased to very significant, its contours are rounded in the shape of a “decanter”, the shadow of the vessels is shortened, atelectasis of the lower lobe of the left lung is observed (Evert’s symptom).
With exudative pericarditis, the ECG showed a total decrease in the voltage of the QRS complexes in all leads, atrial overload, arrhythmia (ventricular extrasystole), but these signs are not specific (Fig. 2 c).
The cardiointervalographic study data reflect the hyperdiastolic variant and the breakdown of the body’s compensatory forces (Table 2).
table 2
. Indicators of the cardiointervalographic study method according to R.M. Baevsky.
| Mo1 | 0,56″ | Mo2 | 0,52″ |
| Amo1 | 57% | Amo2 | 46% |
| ΔX1 | 0,10″ | ΔX2 | 0,12″ |
| IN1 | 1017.85 USD | IN2 | 737.2 USD |
Results of the rhythmogram analysis: blood pressure lying 180/116, standing 160/130 mm Hg. Art. BP - 0.72 USD
The coefficient of the body's compensatory capabilities is L=71 cu, which corresponds to severe heart failure.
An echocardiography study revealed 1.5 liters of fluid in the pericardial cavity (Fig. 2 d), compaction and thickening of the pericardial leaves up to 8 mm, separation of the leaves behind the anterior wall of the right ventricle up to 26 mm and the posterior wall of the left ventricle up to 12 mm were noted (Fig. 2 d, f), the presence of inclusions of fibrin and platelets in the pericardial fluid; Collapse of the anterior wall of the right ventricle and the anterior wall of the right atrium in diastole, a decrease in systolic and impaired diastolic function of the myocardium of the right and left ventricles, and regurgitant flows in the inferior vena cava and hepatic veins were present.
Culture of pleural fluid revealed Mycobacterium tuberculosis (++); An enzyme immunoassay of blood and the results of the NCT test provided data on specific inflammation.
Thus, the diagnosis of acute exudative pericarditis with signs of tamponade and severe heart failure was made according to X-ray examination, echocardiography and cardiointervalography study. Sufficiently convincing signs of pericarditis of tuberculous etiology were tuberculin skin tests, as well as enzyme immunoassays of blood and pleural fluid.
Example 3 illustrates the good result of specific therapy in a patient with chronic exudative pericarditis and pleurisy of tuberculous etiology (Fig. 3).
A 56-year-old woman was admitted to the surgical department with a diagnosis of chronic exudative pleurisy of tuberculous etiology, which she had suffered from for 5 years. The patient was admitted to the clinic to practice treatment tactics during an exacerbation with complaints of pain in the right side and behind the sternum, aggravated by coughing and changing body position; shortness of breath on exertion, low-grade fever for 2 weeks.
An X-ray examination of the chest organs revealed an effusion in the interlobar fissure, paramediastinal and in the infero-posterior parts of the right pleural cavity; the costophrenic sinus is not differentiated, the pulmonary pattern is emphasized, the structure of the right root is preserved. The left lung is unchanged. The size of the cardiovascular shadow is not increased. The cardiac arches along the left contour of the heart are not clearly differentiated (see Fig. 3 a, b).
ECG data revealed a decrease in the amplitude of the waves in all leads, an increase in the load on the right atrium and moderately pronounced diffuse changes in the myocardium of the left ventricle (see Fig. 3c). During the cardiointervalographic study, asympathicotonic autonomic reactivity and the hyperdiastolic variant of the cardiointervalographic study were determined (Table 3).
Results of rhythmogram analysis: blood pressure lying down 160/95, standing 150/100 mm Hg. Art. BP - 0.68 USD
The coefficient of the body's compensatory capabilities is L=41.3 cu, which corresponds to moderately severe heart failure.
Rice. 3.
A patient with chronic tuberculous pleurisy and pericarditis before and after treatment.
a, b)
X-rays of the chest cavity before treatment.
V)
Electrocardiogram before treatment.
G)
Echocardiogram before treatment.
d, f)
X-rays of the chest cavity after treatment.
and)
Electrocardiogram after treatment.
h)
Echocardiogram after treatment.
Table 3
. Indicators of the cardiointervalographic study method according to R.M. Baevsky.
| Mo1 | 0,66″ | Mo2 | 0,58″ |
| Amo1 | 57% | Amo2 | 48% |
| ΔX1 | 0,10″ | ΔX2 | 0,14″ |
| IN1 | 863.63 USD | IN2 | 591.13 USD |
An echocardiogram examination of the patient revealed: thickening and compaction of the pericardial leaves, areas of adhesion behind the posterior wall of the left ventricle, separation of the pericardial leaves behind the anterior wall of the right ventricle of 9 mm, unevenness of the internal contour of the pericardial leaves, a moderate increase in the amount of fluid in the pericardial cavity up to 110 ml with inclusions fibrin, early diastolic movement of the interventricular septum, impaired diastolic function of the left ventricular myocardium (type I), decreased systolic function of the myocardium of the right (EF=50%) and left (EF=56%) ventricles (see Fig. 3d).
After 3 months of anti-tuberculosis treatment, the patient showed significant positive dynamics. During an X-ray examination of the chest organs, the amount of fluid in the mediastinal pleura decreased significantly, and a tendency towards the organization of pleural effusion was noted. Noteworthy is the increase in the intensity of the pleural shadow adjacent to the cardiac shadow, which indirectly indicates the involvement of the pericardium along with the pleural layers in the process (see Fig. 3 e, f).
A cardiointervalographic study reveals a hypersympathicotonic variant of a cardiointervalographic study with sufficient autonomic reactivity (Table 4). The coefficient of compensatory capabilities of the body is L = 3.1 c.u., which corresponds to the norm.
Table 4
. Indicators of the cardiointervalographic study method according to R.M. Baevsky.
| Mo1 | 1,0″ | Mo2 | 0,86″ |
| Amo1 | 33% | Amo2 | 43% |
| ΔX1 | 0,24″ | ΔX2 | 0,12″ |
| IN1 | 137.5 USD | IN2 | 471.5 USD |
Results of the rhythmogram analysis: blood pressure lying down 140/80, standing 150/85 mm Hg. Art. VR - 3.4 USD
According to echocardiography, compaction of the parietal layer and still persisting thickening of the visceral layer of the pericardium, absence of adhesion areas behind the posterior wall of the left ventricle, a decrease in the amount of fluid in the pericardial cavity to 89 ml, normalization of the diastolic function of the left ventricle myocardium, an increase in the systolic function of the right myocardium (EF=62) were noted %) and left (EF=75%) ventricles (see Fig. 3 h). The absence of clear positive dynamics on the ECG (Fig. 3g) is characteristic of the course of chronic pericarditis.
Thus, according to echocardiography and cardiointervalography studies, the patient was diagnosed with chronic exudative pericarditis with moderately severe heart failure before treatment and in the stage of partial resorption without signs of heart failure during anti-tuberculosis therapy.
Another observation of ours demonstrates the difficulties of clinical and radiological diagnosis of constrictive pericarditis of tuberculous etiology.
Example 4. A 55-year-old patient was admitted to the therapeutic department for examination and treatment with a diagnosis of cirrhotic pulmonary tuberculosis, pulmonary heart failure (Fig. 4). His condition began to deteriorate 6 months before admission to the hospital. From the anamnesis it is known that the man has been ill with tuberculosis for more than 20 years, and for the last 5 years there have been no exacerbations.
Upon admission, the condition was serious. Complaints of severe shortness of breath at rest, dry cough, swelling. On examination, the skin is pale, ascites, swelling of the legs and feet. Auscultation - harsh breathing, no wheezing, no breathing in the upper left regions. Heart sounds are dull, the boundaries of the heart are not expanded.
On survey radiographs (Fig. 4 a, b), the upper lobe of the left lung is reduced in volume, intensely heterogeneously darkened due to gross fibrous changes and massive pleural layers, against which intensive, clearly defined foci of varying sizes are identified. An area of coarse linear fibrosis is also detected in the upper lobe of the right lung. The left root is pulled upward and is not structured. The mediastinal organs in the upper section are shifted to the left. The shadow of the heart is located vertically, the 2nd arch bulges on the right. Conclusion: pleuropneumocirrhosis of the lungs.
The patient underwent computed tomography (Fig. 4 d, e), which revealed no fresh infiltrative and focal changes in the lungs. Conclusion: CT scan shows cirrhotic pulmonary tuberculosis. Atherosclerosis of the aorta. Fluid in the pericardial cavity, pleural cavities, compaction of the pericardial layers, and pericardial adhesions are not detected.
The ECG shows pronounced sinus tachycardia (heart rate = 120 beats/min, deviation of the electrical axis of the heart to the right with a clockwise rotation around the longitudinal axis, systolic overload of the right parts of the heart, pronounced diffuse changes in the myocardium of the left ventricle (Fig. 4c).
Rice. 4.
A patient with constrictive pericarditis.
a, b)
Survey radiographs.
V)
Electrocardiogram.
G)
Computer tomogram.
d)
Computer tomogram.
e)
Echocardiogram.
In a cardiointervalographic study, there is an asympathicotonic autonomic reactivity and a hyperdiastolic variant of a cardiointervalographic study (Table 5). The coefficient of compensatory capabilities of the body L = 92 cu, which corresponded to severe heart failure.
Table 5
. Indicators of the cardiointervalographic study method according to R.M. Baevsky.
| Mo1 | 0,56″ | Mo2 | 0,48″ |
| Amo1 | 43% | Amo2 | 41% |
| ΔX1 | 0,08″ | ΔX2 | 0,12″ |
| IN1 | 479.9 USD | IN2 | 355.9 USD |
Results of rhythmogram analysis: blood pressure lying down 160/100, standing 150/115 mm Hg. Art. BP - 0.74 USD
An echocardiography study (Fig. 4f) revealed thickening up to 8 mm and compaction of the pericardial layers, absence of echo-negative space behind the posterior wall of the left ventricle and behind the anterior wall of the right ventricle, parallel anteroposterior movement of the pericardial layers, diffuse hypokinesis of the interventricular septum, dyskinesis of the interventricular septum, diffuse hypokinesis posterior wall of the left ventricle, a significant decrease in the systolic function of the myocardium of the left and right ventricles: LV ejection fraction (EF) = 39%, LV shortening fraction (SF) = 19, RV EF = 35, RV EF = 17%. It was not possible to assess left ventricular diastolic function due to severe tachycardia. Dopplerography revealed a decrease in early mitral flow at the beginning of inspiration, a slowdown in the time of isovolumic relaxation, and a decrease in early tricuspid flow with the beginning of expiration. The absence of changes in the diameter of the inferior vena cava during inspiration, regurgitant flows in the inferior vena cava and hepatic veins indicated the development of pulmonary hypertension (systolic pressure in the pulmonary artery was 84 mm Hg).
Thus, according to echocardiography and cardiointervalography studies, a diagnosis of constrictive pericarditis with signs of severe heart failure was made, and the patient was sent to the surgical department.
From example 4 it is clear that the duration of the period from the appearance of the first signs of the disease to the start of antibacterial therapy is of great prognostic significance.
Analyzing the above clinical observations, I would like to note that of the entire range of radiological research methods, ultrasound is the leading one in the diagnosis of pericarditis. It should be noted that a thorough analysis of clinical data, supplemented by such radiation, functional and laboratory research methods as radiography, ECG, cardiointervalography study, tuberculin skin tests, enzyme immunoassays of blood and pleural fluid, allowed us to avoid serious diagnostic errors and once again confirmed the well-known thesis domestic clinician prof. I. A. Kassirsky: “Yes to technology, no to technicalism.”
Conclusion
The development of medicine is inextricably linked with the improvement of instrumental methods of functional, ultrasound and x-ray diagnostics and the deepening of knowledge in these disciplines.
However, correct interpretation of instrumental data and obtaining a general idea of the pathology is impossible without a preliminary clinical and laboratory examination of the patient. Only in the hands of a clinician is it possible to correctly assess the data of the anamnesis, complaints and objective status in each specific case, and compare with them the information obtained using instrumental methods. The latter provide the most complete information about the disease.
Literature
- Diagnosis and treatment of internal diseases / Under. ed. HER. Gogin. M.: Medicine, 1991. T. I. S. 383, 388-390.
- Clinical guidelines for ultrasound diagnostics. T. 5. M.: Vidar, 1998.
- Malaya L.T. Diagnosis and treatment of heart and vascular diseases caused by tuberculosis. Kyiv, 1969. P. 43.
- Ratobylsky G.V., Ovchinnikov V.I. X-ray diagnosis of pericarditis in patients with end-stage chronic renal failure using computed tomography and color interpretation // Therapeutic archive. T. 61. 1989. N 6. P. 102-105.
- Sumarokov A.V., Moiseev V.S. Clinical cardiology: A guide for doctors. M., 1995. P.127.
- Khomenko A.G. Tuberculosis: A Guide to Internal Medicine. M.: Medicine, 1996.
- Feigenbaum H. Echocardiography. M.: Vidar, 1999.
- Keller E. Beitr. Klin. Tuberk., 1963. N 82. R. 213-219.
SonoAce Ultrasound Magazine
Contains current clinical information on ultrasonography and is aimed at ultrasound doctors, published since 1996.