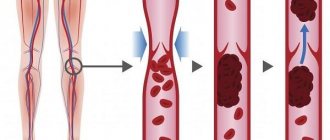
Phlebitis is an inflammatory disease that affects the walls of venous vessels. The disease can occur in acute and chronic form. Phlebitis often develops against the background of progressive varicose veins. As a rule, the lower extremities are affected by inflammation, but the development of phlebitis of the hands is possible. If the treatment of venous phlebitis is inadequate or untimely, blood clots form after the inflamed venous wall changes. At this stage, phlebitis develops into thrombophlebitis, which is more difficult to treat and can cause serious complications. Treatment of phlebitis is conservative, involving the use of medications and physiotherapeutic procedures. At the Hemostasis International Clinic, experienced phlebologists with many years of experience treat such vascular diseases. Our specialists successfully treat even advanced forms of pathology, so if you need qualified medical care, contact us.
General information about the disease
Phlebitis is an inflammation of the venous walls, which in most cases is a consequence of advanced varicose veins. The disease mainly affects the superficial veins, but in the absence of adequate therapy it spreads to the deep vessels, causing phlebitis of the deep veins. As the disease progresses, nearby tissues may become involved in the pathological process. According to the latest statistics, the disease is diagnosed mainly in elderly patients over 50 years of age. Moreover, women suffer from phlebitis more often than men.
Basic methods of treating veins
After introducing the cytostatic into the cells, all that remains is to wait for the completion of the side process and help recovery.
The pathophysiology of drug-induced toxic phlebitis has been little studied, no clinical studies have been conducted on the problem, all recommendations are based only on the personal experience of medical personnel. In each case and after each administration, it is necessary to consult with the attending physician who knows the specifics of the local interaction of the cytostatic and the range of local adverse reactions.
To relieve pain and reduce inflammation, NSAIDs are best suited - non-steroidal anti-inflammatory drugs, but the benefits of any one drug have not been proven; it is better to rely on the patient’s “everyday” preferences, because sensitivity to pain is different, and the analgesic effect is also individual.
If there is a high risk of pulmonary thromboembolism, the patient is prescribed a special “blood thinning” therapy, usually long-term - at least a week and with regular monitoring of coagulation.
You can use ointments with heparin to rub into the area of the damaged vessel. Hepatrombin™ gel consists of heparin and prednisolone, the latter has an anti-inflammatory effect, the drug is not officially certified for use in peripheral phlebitis and thrombophlebitis.
Troxevasin™ ointment has a good reputation , which simultaneously reduces inflammation and swelling of tissues, changing the rheological properties of blood towards dilution, but less than is typical for heparin. However, studies have shown that the drug is capable of dissolving microthrombi.
Indovazin™ gel is a mixture of troxerutin and the NSAID indomethacin, therefore it reduces the severity of pain and does everything that is inherent in Troxevasin™. It is not advisable to combine both ointments, since the spectrum of action of the combined drug is greater, but with Indovazin™ it is quite possible to alternate the application of Hepatrombin™. The absorption of ointments is microscopic; they do not replace NSAIDs and anticoagulants taken orally, but they help to endure the unpleasant consequences of treatment.
Pathogenesis
The inflammatory process can be caused by various etiological factors, such as:
- infection;
- allergy;
- mechanical damage, etc.
The disease can also develop after a chemical burn to a vessel. In certain situations, phlebitis can be caused artificially. For example, during the treatment of varicose veins in phlebology, a technique called sclerotherapy is often used. The principle of operation of the procedure is based on the introduction of a special drug that causes aseptic phlebitis, which promotes subsequent gluing of the venous walls.
Classification
Depending on the location of inflammation in the venous wall, the following types of phlebitis are distinguished:
- Periphlebitis. Characterized by inflammation of the outer venous membrane. It often develops when the inflammatory process of the surrounding tissues spreads to the walls of the veins.
- Endophlebitis. With this pathology, the inflammatory process is localized on the inner lining of the vessel. Occurs due to damage to the inner lining of the vein or trauma to the vessel. The main causes of endophlebitis: catheterization, prolonged stay of the needle in the vessel during drip administration of drugs.
- Panphlebitis. Characterized by damage to all the membranes of the vessel.
Taking into account the etiological factor, the following forms of phlebitis are distinguished:
- Allergic. Develops as a result of an allergic reaction of the body to the introduction of a foreign agent. This type of phlebitis often becomes chronic.
- Painful. Develops in women after childbirth. It affects the lower extremities, is characterized by an acute course, accompanied by pronounced pain symptoms.
- Migratory. This disease mainly affects young men. The pathological process involves the superficial veins of the lower or upper extremities. Migrating phlebitis is often accompanied by damage to the arteries and is characterized by a long, chronic course.
- Cerebral. Inflammatory processes are localized in the vessels of the brain. Phlebitis of cerebral vessels is mainly the result of an infection.
- Pylephlebitis. It is characterized by inflammation of the collar vein and is often a complication of the inflammatory process occurring in the abdominal cavity.
- Infectious. Can affect any part of the human body.
According to the nature of the flow, they are distinguished:
- Acute phlebitis. It is characterized by pronounced symptoms and an acute course. Requires emergency medical attention.
- Chronic phlebitis. It is characterized by sluggish current symptoms, and with a confluence of unfavorable factors, it is prone to relapses.
How veins are restored after IVs: useful procedures
They try to reduce local irritation of the mucous membrane lining the inner wall of the vein by large dilutions and slow administration in droppers, literally over hours. Not all cytostatics can withstand high dilution and long administration; some lose their properties, so they are administered as a bolus using a syringe. In this case, immediately after chemotherapy, the vein is “washed” with saline, trying to reduce its damage.
Be sure to check the patency of the vessel and the possibility of extravasation - the spread of cytostatics in the tissue during microscopic ruptures of the vascular wall - before administration and during the drip.
It is recommended not to administer chemotherapy to the same vein; it is better to alternate hands, giving the vessel more time to restore its mucous membrane. The prophylactic use of ointments with heparin or troxerutin before chemotherapy has no pathomorphological basis, that is, it is useless.
When planning multi-month chemotherapy, it is advisable to think about installing a venous port; its service life is at least five years. The device completely eliminates such a side effect as drug phlebitis, but only taking anticoagulants can save you from thrombosis.
Causes of phlebitis
Phlebitis of the superficial veins begins to develop as a result of an inflammatory process that affects the walls of the vessel. Factors contributing to its occurrence:
- tendency to allergic reactions;
- immune dysfunction;
- vascular injuries;
- chronic venous insufficiency;
- blood clotting disorder;
- violation of lymphatic flow;
- varicose veins;
- physical inactivity, which contributes to the development of stagnant processes;
- obesity, which increases the load on the lower limbs;
- a job in which a person is forced to constantly be on his feet.
Post-injection phlebitis of the upper extremities also often occurs against the background of varicose veins. The pathology may be a consequence of trauma to the vessel during injection or drip intravenous administration of the drug, as well as prolonged placement of a catheter in the vein. Post-injection phlebitis is mainly encountered by people who use injecting drugs, as well as those undergoing chemotherapy.
Features and reasons for development
Under certain conditions, the inflammatory process affects the walls of blood vessels of any location, but in the vast majority of cases the disease affects the veins of the lower extremities, and primarily the superficial vessels deformed by varicose veins. Deep veins, along with superficial ones, become inflamed in approximately 10% of patients. The clinical picture is formed under the influence of a number of factors: an increase in the blood clotting index under the influence of changes in its composition, blood flow speed, the presence of deformations or damage to the vascular wall, etc.
The causes of thrombophlebitis include:
- genetic predisposition factor;
- varicose veins, which leads to stagnation of blood in the veins of the legs;
- wound or injury of the lower limb, accompanied by a purulent process;
- postoperative recovery period (including after medical abortion);
- postpartum period;
- long stay of the catheter in the vein;
- bed rest or immobility of the patient;
- dehydration of the body;
- age after 40 years.
The development of the inflammatory process is promoted by any disease or condition associated with decreased immunity.
Symptoms of phlebitis
With inflammatory damage to the superficial veins, local symptoms come to the fore, such as:
- severe pain, tension in the area of the affected vein;
- redness and thickening of the skin over the inflamed area;
- formation of red stripes along the affected vessel;
- increase in body temperature.
Signs of deep vein phlebitis will vary. First of all, the patient’s body temperature rises, pain and severe swelling occur in the affected area. The skin over the affected area turns pale, acquiring a marble-white hue. If there is no treatment for acute phlebitis, the risk of developing thrombophlebitis increases, in which blood clots form on the inflamed walls of the vessel. In case of chronic course
Tests and diagnostics
The superficial form of phlebitis is determined already during the initial examination. The affected limb looks swollen, hyperemic, and upon palpation a thickening is felt over the inflamed area. To diagnose superficial and deep phlebitis, a comprehensive diagnosis is prescribed, consisting of the following types of procedures:
- Hemostasiogram. This is a laboratory blood test to determine hypercoagulability and susceptibility to thrombosis.
- Ddimer - marker - thrombus formation
- Platelet aggregation. Blood test indicating the risk of thrombosis and the need for treatment
- Blood test for the presence of an infectious pathogen.
- Ultrasound duplex scanning of blood vessels. Allows you to evaluate the structure and patency of the veins, as well as evaluate the nature of blood flow through them, determine the exact localization of the pathological process in the veins, and assess the nature of blood flow through the affected vessel.
- Ultrasound examination of veins Doppler examination allows you to assess the degree of their patency and identify areas with impaired blood circulation.
Additionally, computed tomography or magnetic resonance imaging may be prescribed, which will allow a detailed examination of the veins, their location, and to see areas of inflammation.
Treatment of phlebitis
Treatment of phlebitis of the arm or leg can be carried out on an outpatient basis or in a hospital setting. It all depends on the nature of the disease, its type, and the presence of associated complications. If superficial phlebitis of the vein is diagnosed, treatment is carried out on an outpatient basis. To relieve the inflammatory process and accompanying symptoms, as well as strengthen the venous walls and normalize blood flow, the following groups of medications are used:
- Nonsteroidal anti-inflammatory drugs. They help eliminate the inflammatory process, swelling, hyperemia, and have a pronounced analgesic effect.
- Venotonics. Strengthen vascular walls, increasing their elasticity, and help normalize blood circulation.
- Anticoagulants. They have a blood-thinning effect and prevent thrombosis.
If necessary, broad-spectrum antibiotics and antihistamines are used. After stopping the inflammatory process, phlebitis of the lower extremities can be treated using physiotherapeutic procedures, which:
- restore tissue trophism;
- stimulate regeneration processes;
- increase local immunity;
- prevent relapses;
- have a general strengthening effect.
The following physiotherapy methods are effective for phlebitis:
- medicinal electrophoresis;
- magnetic or laser therapy;
- darsonvalization;
- diadynamic currents;
- mud applications;
- Ural Federal District;
- UHF;
- acupuncture, etc.
To prevent relapses, it is recommended to regularly use compression hosiery, which will protect the veins from overstretching, help normalize blood circulation and intravascular pressure, and minimize the risk of the spread of pathology.
How to treat
To treat thrombophlebitis, modern medicine uses various methods, from drug therapy to surgical intervention, depending on the severity of the disease and its stage. Most patients are usually prescribed conservative therapy, the goal of which is to stop the inflammatory process and reduce the risk of vascular thrombosis. For this purpose, the doctor prescribes:
- anti-inflammatory non-steroidal drugs;
- anticoagulant medications;
- enzyme therapy;
- treatment with phlebotonics;
- local compresses and ointments;
- in the presence of a purulent process - antibiotic therapy.
The patient is prescribed bed rest, but he can be treated at home if there is no risk of complications. Mechanical support of the blood vessels is important: it is necessary to bandage the affected limb with an elastic bandage and/or wear special compression garments. If there is a risk of disease progression and transition to deep veins, surgical removal of the thrombosed vessel is prescribed.
Prevention
The following rules of prevention will help prevent the development of phlebitis:
- adherence to the basics of a healthy lifestyle;
- quitting smoking and drinking alcohol;
- proper nutrition;
- body weight control;
- engaging in moderate physical activity with a sedentary lifestyle;
- normalization of work and rest regime
- hemostasiogram, DDimer, AT3 – blood test once a year.
If any suspicious symptoms appear, do not self-medicate, but seek professional help from a phlebologist as soon as possible. Only correct and adequate treatment will help stop the progression of inflammation and prevent serious complications.
Forecast
Life-threatening complications are rare. Pulmonary embolism is observed in only 2% of cases of subclavian thrombosis. Even with immediate intervention, some patients do not fully regain arm function and may have residual symptoms or require continued treatment. Severe venous insufficiency of the arm usually does not occur. Thrombosis of the subclavian vein does not pose a serious threat to life. After adequate treatment, the edema decreases significantly, but complete patency is rarely restored. If the causes for subclavian thrombosis persist, relapses of the disease may occur, so it is necessary to identify and eliminate them. As a reminder of the history of venous thrombosis, the patient is left with an increase in the volume of the shoulder and a network of visible saphenous veins in the area of the shoulder joint.
Prevention of phlebitis during pregnancy
During pregnancy, every woman may experience phlebitis, especially if she was previously diagnosed with varicose veins of the lower extremities. During pregnancy, most drugs used to treat phlebitis are strictly contraindicated. Therefore, it is necessary to take all measures to help prevent such vascular disease. Throughout the entire period of bearing a baby, it is useful to follow these simple recommendations:
- take daily walks in the fresh air;
- regularly do exercises that have a general strengthening effect;
- control weight;
- Healthy food;
- If you have suspicious symptoms, consult a doctor rather than wait for the situation to resolve on its own.
Consequences of the disease
If you ignore the need for treatment and do nothing, phlebitis can become thrombophlebitis. As a result, one of the formed blood clots can break off at any moment and block the blood flow, and this can lead to death. Previous phlebitis, in turn, can cause postthrombophlebitis disease.
The most common disease is among:
- athletes;
- people with varicose veins;
- smokers;
- drug addicts;
- people who are given medications over a long period of time using a venous catheter.
Diet
If you have phlebitis, you need to radically reconsider your eating habits and give up foods containing large amounts of salt, animal fats, preservatives and other chemical additives. It is advisable to eat often, but little by little. Prepare dishes using gentle methods: steamed, oven, grilled, or simply boiled in water. Diet for thrombophlebitis For thrombophlebitis, the diet should consist of the following food groups:
- fish, seafood;
- lean meat;
- cereals: buckwheat, rice, oatmeal;
- fresh vegetables, fruits, berries, herbs;
- dairy and fermented milk products;
- freshly squeezed juices, fruit drinks;
- dried fruits, seeds, nuts.
What is prohibited for thrombophlebitis?
If a person develops a disease, he is strictly prohibited from:
- Wear uncomfortable high-heeled shoes.
- Lift heavy objects.
- Engage in sports that involve intense stress on the limbs.
TF of deep veins is a restriction for visiting saunas, drinking bowls and baths. This is due to the fact that high temperatures significantly accelerate blood circulation, which has an extremely negative effect on the course of the disease.
It is strictly forbidden to gain extra pounds, and therefore a person must pay special attention to proper nutrition. Animal fats, which can be replaced with vegetable oils, should be excluded from the diet. The amount of salt consumed should be kept to a minimum in order to eliminate swelling. Quitting alcohol and smoking is mandatory for TF.
Cost of phlebitis treatment
The cost of phlebitis treatment for each patient is calculated separately. The following factors are taken into account:
- the stage at which the disease was diagnosed;
- therapy methods used;
- duration of treatment;
- presence of complications, etc.
To get a more extensive consultation and make an appointment with a specialist at the International Hemostasis Clinic, call +7 or fill out the online form on the website. Ultrasound of blood vessels is performed by an expert, Professor T.V. Balakhonova, treatment is carried out by a phlebologist, Professor A.I. Shimanko.