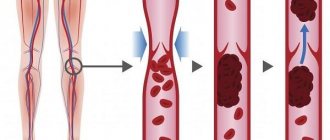
Thrombosis in pregnant women is a pathological condition characterized by the formation of blood clots in the lumen of blood vessels, which are called thrombi. They do not allow blood to circulate freely through the circulatory system, seriously impeding blood flow and causing a number of serious complications. Vein thrombosis in pregnant women is not uncommon. It appears against the backdrop of a number of changes occurring in a woman’s body during this period, and requires special attention both from the woman herself and from doctors.
Prevention of thrombosis in pregnant women and its treatment is one of the areas of work of the CELT Phlebology Department. Our clinic has been operating since 1993 and is multidisciplinary, so phlebologists work closely with gynecologists, achieving the best results. They have at their disposal a powerful diagnostic and treatment base, as well as modern gentle techniques that allow them to maintain the patient’s health and give birth to a healthy baby.
At CELT you can get advice from a phlebologist.
- Initial consultation – 3,000
- Repeated consultation – 2,000
Make an appointment
What is deep vein thrombosis?
Thrombosis (phlebothrombosis) of the deep veins of the lower extremities is the result of the formation of blood clots (thrombi) that obstruct the outflow of blood in the main venous vessels of the thighs and legs. The resulting blood clot blocks blood flow and makes it difficult for venous blood to rise from the legs to the lungs and heart.
Neglect of timely treatment can lead to complications, and in isolated cases, death.
Women are more susceptible to the disease than men, but the risk of developing the disease in women increases when taking combined oral contraceptives.
Treatment of phlebothrombosis: traditional and folk medicine
All of us know the simple truth that treatment of any disease should begin as early as possible. For patients diagnosed with phlebothrombosis of the lower extremities, doctors will provide assistance at any stage from the formation stage to the recanalization stage.
Timely treatment makes the prognosis more favorable - the risk of thromboembolism is significantly reduced, further spread of the blood clot is stopped, the blood clot is resolved with the restoration of the vein lumen to one degree or another, which means that the manifestations of post-thrombophlebitis syndrome are minimized.
How to treat phlebothrombosis? Therapy for this disease is always complex. As mentioned earlier, it depends on the etiology and degree of development of the pathology. The treatment regimen involves conservative therapy and, if necessary, surgical intervention.
Conservative methods include:
- Taking medications. To improve the rheological properties of blood and increase the elasticity of vessel walls, various groups of medications are used: phlebotonics, antiplatelet agents, anti-inflammatory drugs and anticoagulants.
- Carrying out local therapy. The use of ointments and gels that have anti-inflammatory, venoprotective, decongestant and other effects.
- Wearing medical compression stockings or bandaging limbs.
- Nutrition. The diet for phlebothrombosis of the lower extremities excludes alcohol and spicy foods. You should drink at least 2 liters of fluid and eat foods rich in antioxidants.
If conservative therapy methods fail to achieve a positive result, then surgical methods will be used.
In case of acute development of the disease at home, an ambulance call is required as early as possible.
Expert opinion
Until the doctors arrive, it is important to try to fix the limb in a motionless state. This will reduce the risk of a blood clot breaking off.
Vascular surgeon, phlebologist
Osipova Ekaterina Yakovlevna
Phlebothrombosis - herbal baths
Symptoms of deep vein thrombosis of the leg and thigh
The deep veins in the lower extremities (great and common femoral veins, popliteal vein, deep veins of the leg) are located far from the surface, so there are no visible signs of thrombosis in the early stages.
The first symptoms to look out for may be:
- pain and increased sensitivity;
- stiffness of movements;
- feeling of heaviness and pressure in the muscles.
Important:
discomfort in the legs is a reason to consult a doctor.
Make an appointment
With the further development of the disease, obvious signs appear:
- change in skin color;
- swelling starting from the foot;
- expansion of superficial veins;
- local temperature increase.
Important:
If you experience any of the symptoms described above, consult your doctor immediately. The appearance of these signs signals the transition of the disease to the acute stage.
Thrombolysis
Dissolution of venous blood clots with special drugs - thrombolytics. These include streptokinase, urokinase and actilise. Only direct administration of a thrombolytic through a catheter into a thrombus with regular monitoring of the patency of the affected segment is effective. Thrombolysis options may include the use of a special Angiojet device. The thrombolytic solution is supplied through a special probe under high pressure, and then the blood clots are sucked out by a special suction. Another similar device used in our clinic is the Aspirex probe. This is a special spiral suction that gently removes thrombotic masses. The use of Aspirex in the inferior vena cava is limited due to its large diameter, so catheter thrombolysis is the most acceptable method. Thrombolysis is possible only in the first 10 days from the onset of the disease, while the blood clots have not yet healed.
Primary risk factors for thrombosis:
- frequent or extensive surgical operations;
- wearing a central venous catheter;
- severe injuries to the legs or pelvis;
- prolonged immobility (bed rest, wearing a cast);
- individual blood characteristics (high blood clotting, high levels of homocysteine or fibrinogen);
- oncology;
- heredity (antithrombin deficiency, pathologies of the system, blood circulation or homeostasis, problems with the secretion and absorption of proteins C and S).
Important:
congenital hereditary and individual characteristics are the most dangerous risk factors for thrombosis.
What causes vascular diseases
The main cause of vascular diseases is high blood clotting. Damage to the venous wall and slowing down blood movement also play an important role. In addition, there are a number of aggravating factors:
- bad habits such as smoking;
- lower limb injury;
- overweight;
- pregnancy, childbirth or caesarean section;
- infectious diseases;
- frequent flights or trips;
- advanced age;
- sedentary lifestyle;
- bone fractures, joint surgeries and abdominal surgeries.
Diagnosis of deep vein thrombosis
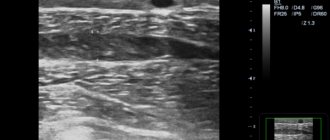
After a visual examination and medical history, the doctor prescribes a general blood test and a coagulogram to determine the patient’s condition and blood clotting indicators. Next, ultrasound duplex scanning of the veins is prescribed to assess hemodynamic parameters and identify structural changes in the walls of the venous vessels. Along with ultrasound, the doctor may perform plethysmography and contrast venography.
If ultrasound is not possible, alternative diagnostic methods are:
- MSCT (multispiral computed tomography);
- MRA (magnetic resonance angiography).
The listed diagnostic tools are sufficient to make a diagnosis and choose an effective treatment method.
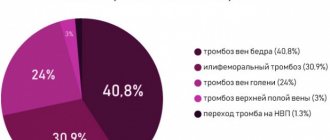
Material and methods
The work is based on the results of complex diagnostics and treatment of 432 patients with acute IPVT of NK who were in the department of vascular surgery of the Republican Scientific Center for Cardiovascular Surgery over the past 8 years (2007-2014). Among those observed there were 289 (66.9%) women and 143 (33.1%) men aged from 19 to 84 years (average age 51.71±2.2 years).
The predominance of females among patients ( n
=289) can be explained by the use of hormonal contraceptives, frequent pregnancies and childbirth, typical for women in the Republic of Tajikistan. The increased weight and low mobility of the patients were of no small importance. The majority (68.75%) of patients with IPVT were in the middle and older age categories.
It should be noted that among the patients living in rural areas, there were 319 (73.8%), urban - 113 (26.2%) residents. Of the rural residents, 57 (17.9%) lived in the high mountain valleys of the Pamirs.
The diagnosis was made based on the clinical manifestations of the disease and the results of duplex ultrasound angioscanning (USDAS).
Ultrasound diagnostic systems were performed with PHILIPS SD 800 (USA, 2005) and DC-3 Mindray (China, 2012) diagnostic systems equipped with sensors with a frequency of 3.5-10 MHz, using B-mode and color Doppler mapping of blood flow.
The state of the hemostatic system was assessed by determining the level of activated partial thromboplastin time (aPTT), prothrombin time (PTT), prothrombin index (PTI), international normalized ratio (INR), thrombin time, fibrinogen, platelet count, Lee-White SSC and kaolin time .
The main objective of this study was an attempt to establish a connection between changes in the hemostatic system and the development of IPVT, as well as the need to influence this system during the treatment of patients.
All data obtained as a result of the study were processed using Microsoft Office Excel 2007. Parametric descriptive statistics were calculated: mean ( M
), standard deviation (σ), mean square error (
m
).
The statistical significance of the differences in indicators was carried out using t
-test.
Differences between indicators were considered statistically significant at p
<0.05.
Conservative treatment methods
Bed rest
Before the examination, all patients are prescribed bed rest. When diagnosing occlusive and parietal forms of venous thrombosis, it is canceled, in other cases it is maintained until blood flow is restored and the threat of thrombus separation is eliminated.
Compression jersey
According to indications for deep vein thrombosis, compression stockings of 2 or 3 compression classes are used.
Important:
Elastic compression can only be used as prescribed by a doctor. In some cases it is contraindicated.
Drug therapy
Injections of direct anticoagulants (sodium heparin, etc.) are mandatory for everyone in the treatment of deep vein thrombosis of the lower extremities. They prevent the formation of blood clots.
Having passed the acute stage, they switch to indirect anticoagulants (warfarin, etc.)
In addition to anticoagulants, thrombolytic therapy may be prescribed, aimed at restoring blood flow and destroying formed blood clots.
Sometimes in the acute stage a combination of direct and indirect anticoagulants may be used, depending on the specific case.
Surgery
Surgery for deep vein thrombosis of the legs is rarely required.
The operation is prescribed for:
- restoration of vein patency;
- maintaining the function of venous valves;
- preventing pulmonary thromboembolism.
Establishing diagnosis
Diagnosis of the disease is required to establish the affected area based on direct and indirect signs. To do this, the doctor performs an external examination and refers the patient to the appropriate examination.
- An examination by the attending physician allows you to clearly establish the fact of this disease. Upon external examination or examination of photographs of phlebothrombosis of the lower extremities, a change in the skin to a bluish or white color is noted, depending on the nature of the lesion of a particular vessel. The leg is edematous, swollen, sometimes ulcers and roughness of the epidermis can be seen;
- Doppler ultrasound or duplex angioscanning can detect a specific vessel blocked by a thrombus. The monitor will show a narrowing of the lumen of the vein and stagnation of blood;
- Contrast radiography is an effective method that allows you to take pictures with the introduction of a special substance into a vein, which allows you to see the narrowing of its lumen;
- A blood test for formed elements and specific proteins is necessary to diagnose disorders of the qualitative composition of the blood, leading to the formation of blood clots.
As soon as the diagnosis of phlebothrombosis is confirmed, the patient is urgently hospitalized.
Methods for diagnosing pathology
Consequences of the disease: what is the danger of deep vein thrombosis of the lower extremities?
Postthrombophlebitic syndrome (PTPS)
Acute thrombosis of the lower extremities leads to a complex of hemodynamic disorders and the development of chronic venous insufficiency, united under the abbreviation PTFS. The consequences can be assessed after completion of the subacute stage of deep vein thrombosis of the legs (3 months after the end of the acute stage).
PTSD is expressed in the following symptoms:
- heaviness and pain in the area of maximum venous stagnation;
- swelling;
- phlebeurysm;
- trophic disorders (pigmentation, dermatitis, eczema, tissue compaction, trophic ulcers).
Pulmonary thromboembolism
Deep vein thrombosis is scary because the detached blood clot has a direct path to the lungs. Entering the pulmonary arteries through the right side of the heart, the thrombus causes disruption of gas exchange and provokes oxygen starvation. Depending on the size of the blood clot, the consequences can be different: from a normal cough with fever to pulmonary infarction, hypotension, tachycardia and fainting.
Venous gangrene
An overgrown blood clot can completely block a venous vessel and lead to stagnation of blood in the leg below the formation of the blood clot. Stopping blood flow causes tissue necrosis. The prognosis for the preservation of the affected areas is unfavorable. Delay threatens amputation and blood poisoning.
Thrombosis in a pregnant woman: causes
During pregnancy, a number of serious changes occur in the female body. First of all, they are associated with hormonal changes, which affect the functioning of the blood coagulation system, causing the blood to become more viscous and thick. Another reason is the increase in the size of the uterus. It begins to exert a compressive effect on the inferior vena cava, causing disruption of the blood flow, leading to stagnation in the vessels of the legs. Another factor is increased body weight. The above leads to the development of thrombophlebitis. It can occur either as an independent disease or as a complication of thrombosis. Aggravating factors in this case are:
- The woman is over 35 years old;
- Congenital antithrombin deficiency;
- Long-term use of contraceptives;
- Serious injuries in the past;
- Presence of autoimmune diseases.
Prevention
Recommendations for the prevention of deep vein thrombosis of the lower extremities: diet, exercise, clothing.
To prevent thrombosis, you need to pay attention to three things.
- Proper food: sufficient fluid in the diet and a healthy, balanced diet.
- Movement: morning exercises, five-minute walk every hour during sedentary work or static load on the legs.
- Care: compression stockings if there are risk factors and comfortable shoes.
Other articles by the author
- Chronic venous insufficiency
- Thrombophlebitis
- Deep vein thrombosis of the lower extremities
- Phlebeurysm
- Telangiectasias (vascular networks and spider veins on the legs)
The risk group for the development of phlebothrombosis includes:
- Pregnant women, especially in the second - early third trimesters, and women in the postpartum period.
- People who are overweight and lead a sedentary lifestyle and sedentary work.
- Elderly people especially with diseases of the musculoskeletal system.
- Patients with cancer.
- Patients with decompensated forms of cardiovascular diseases.
- Persons whose activities involve heavy lifting or changes in atmospheric pressure.