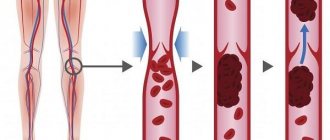
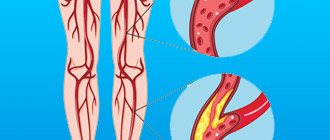
Deep vein thrombosis (DVT) occurs when a blood clot (thrombus) forms in one or more deep veins in your body, usually in the legs. Deep vein thrombosis can cause leg pain or swelling, but may be asymptomatic.
- Symptoms of deep vein thrombosis
- Causes of deep vein thrombosis
- Risk factors
- Complications of DVT
- Prevention of thrombosis
DVT may be associated with diseases that affect the blood clotting process. A blood clot in your legs can also form if you have not moved for a long time, such as after surgery or an accident. But walking over extremely long distances can lead to the formation of blood clots.
Deep vein thrombosis is a serious condition because blood clots in your veins can travel through your bloodstream and become lodged in your lungs, blocking blood flow (pulmonary embolism). However, pulmonary embolism can occur without evidence of DVT.
When DVT and pulmonary embolism occur at the same time, it is called venous thromboembolism (VTE).
Symptoms
Signs and symptoms of DVT:
- Swelling of the affected leg. In rare cases, swelling appears in both legs.
- Leg pain. The pain often begins in the calf and may feel like cramping or soreness.
- Red or discolored skin on the leg.
- Feeling of warmth in the affected leg.
Deep vein thrombosis may occur without noticeable symptoms.
When to see a doctor
If you have signs or symptoms of DVT, contact your doctor.
If you develop signs or symptoms of pulmonary embolism (PE), a life-threatening complication of deep vein thrombosis, get emergency medical help.
Call 103
Warning signs and symptoms of pulmonary embolism include:
- Sudden shortness of breath
- Chest pain or discomfort that gets worse with deep breathing or coughing.
- Feeling dizzy or dizzy or faint
- Rapid pulse
- Rapid breathing
- Coughing up blood
Do you suspect deep vein thrombosis? Contact the professionals.
Treatment of deep vein thrombosis in Moscow
At this stage, many government institutions in Moscow are involved in the treatment of deep vein thrombosis of the lower extremities, but only in the Yusupov Hospital will patients be able to undergo full comprehensive diagnostics and outpatient clinical treatment. The clinic employs phlebologists specializing in deep vein thrombosis, engaged in scientific research and developing new approaches to the treatment of this disease. Thanks to international cooperation with large European and American centers, the hospital has the opportunity to use the most effective and high-quality drugs for the treatment and prevention of thrombosis.
The doors of the Yusupov Hospital are open around the clock. No one is turned away here and they help the most difficult patients. The clinic invites everyone to undergo a phlebological check-up and receive advice from doctors of the highest category. The cost of a comprehensive program includes a full package of services: daily examinations, round-the-clock consultation, drug and surgical treatment, in some cases, even rehabilitation measures. The hospital guarantees all patients examination not only by one specialist, but also by a whole galaxy of competent experts: therapist, cardiologist, surgeon, endocrinologist, nutritionist, neurologist, etc. For the purpose of psychological support, a psychotherapist provides consultations at the clinic. Treatment of deep vein thrombosis of the lower extremities at the Yusupov Hospital costs from 40,000-60,000 rubles.
Nursing and junior medical staff are the pride of the Yusupov Hospital. Highly qualified nurses will always come to the rescue, at any time of the day. Having an incalculable amount of work experience behind them, they know all the nuances of the course of a particular disease down to the smallest detail. Comfortable surroundings and a cozy atmosphere will make your stay in the hospital a joyful and quick one.
Treatment of patients at the Yusupov Hospital is carried out only with the help of innovative techniques used throughout the world.
Risk factors
Many factors can increase your risk of developing DVT, which include:
- Age. At age 60, the risk of DVT increases, although it can happen at any age.
- Sitting for long periods of time, such as while driving or flying. When your legs remain motionless for several hours, your calf muscles do not contract. Muscle contractions promote blood circulation.
- Prolonged bed rest, such as during a long hospital stay or paralysis. Blood clots can form in the calves if the calf muscles are not used for a long time.
- Trauma or surgery. Injury to the veins or surgery may increase the risk of blood clots.
- Pregnancy. Pregnancy increases pressure in the veins of the pelvis and legs. Women with an inherited bleeding disorder are at particular risk. The risk of blood clots from pregnancy can last up to six weeks after the baby is born.
- Birth control pills (oral contraceptives) or hormone replacement therapy. Both factors can increase the blood's ability to clot.
- Exposure to drugs or chemicals. Certain drugs can cause blood clots. Consult your physician before use.
- Overweight or obese. Excess weight increases pressure in the veins of the pelvis and legs.
- Smoking. Smoking affects clotting and circulation, which may increase the risk of DVT.
- Cancer. Some forms of cancer increase levels of substances in the blood that cause blood clotting. Some forms of cancer treatment also increase the risk of blood clots.
- Heart failure. Increases the risk of developing deep vein thrombosis and pulmonary embolism. Because people with heart failure have limited heart and lung function, symptoms caused by even a small pulmonary embolism are more noticeable.
- Inflammatory bowel diseases. Bowel diseases such as Crohn's disease or ulcerative colitis increase the risk of DVT.
- Personal or family history of DVT or PE. If you or someone in your family has had one or both of these, you may be at greater risk of developing DVT.
- Genetics. Some people inherit genetic risk factors or disorders, such as factor V Leiden, that make their blood clot more easily. The hereditary disease itself may not cause blood clots unless it is combined with one or more other risk factors.
- Risk factor unknown. Sometimes a blood clot in a vein can occur without an obvious underlying risk factor. This is called unprovoked VTE.
What is the difference
The pathology differs in the size of the blood clot:
- Occlusive . The thrombus completely covers the venous lumen. The outflow of blood from the lower extremities is completely stopped. This condition leads to necrosis and gangrene.
- Non-occlusive . The venous lumen is partially blocked. The outflow of blood is difficult, but it happens.
There is another type of pathology – floating thrombosis. The thrombus is partially attached to the venous wall and dangles in the lumen of the vessels. This form is no less dangerous than the occlusive one, since a blood clot can break off at any time, block the functioning of the heart or lungs, which will lead to death.
Complications
Complications of DVT may include:
- Pulmonary embolism (PE). PE is a potentially life-threatening complication associated with DVT. This occurs when a blood vessel in your lung is blocked by a blood clot that travels to the lung from another part of your body, usually your leg. If you have signs and symptoms of PE, it is important to seek medical help immediately. Sudden shortness of breath, chest pain when inhaling or coughing, rapid breathing, rapid pulse, feeling weak or faint, and coughing up blood may occur with PE.
- Postphlebitic syndrome. Damage to the veins by a blood clot reduces blood flow to the affected areas, causing leg pain and swelling, skin discoloration, and skin ulcers.
- Complications of treatment. Complications may arise from blood thinners used to treat DVT. Bleeding is a side effect of anticoagulants. It is important to have regular blood tests when taking these medications.
Surgery
In the case of severe occlusive thrombosis, the only way to save the patient is surgical intervention. There are several types of operations:
- Thrombolysis . Through a special catheter, a fibrinolytic is injected into the damaged artery, destroying the thrombotic mass and restoring blood flow through the clogged vessels. This is the only technique that can completely dissolve the blood clot and preserve the venous valves.
- Angioplasty . A special balloon is inserted into the damaged area, which expands under pressure and destroys the blood clot. In the case of atherosclerosis, the patient is additionally fitted with a metal stent, which maintains the patency of the vessel in the future.
- Installation of a vena cava filter . A device is implanted into the venous lumen to capture blood clots migrating with the bloodstream.
It is extremely important to carry out intervention in a timely manner to prevent the development of serious complications. Any of the above operations is performed by vascular surgeons in a hospital setting.
After endovascular intervention, the patient will undergo rehabilitation. The doctor will definitely prescribe anticoagulants, wearing compression stockings, limiting physical activity, and diet.
The thrombolysis procedure has a number of contraindications:
- rehabilitation period after recent surgical interventions;
- extensive internal bleeding, organ damage;
- blood pressure over 200\120 mm Hg, which cannot be corrected;
- pericarditis, pancreatitis;
- previous stroke;
- severe chronic pathologies of the liver and kidneys.
The method of treating thrombosis is determined by the doctor after a comprehensive diagnosis and assessment of the general condition of the patient’s body. If the pathology threatens the patient’s life, the operation will be performed regardless of the presence of contraindications (with the consent of the patient or his relatives).
Prevention
Measures to prevent deep vein thrombosis include the following:
- Don't sit still. If you have had surgery or were on bed rest for other reasons, try to get back to work as soon as possible. If you sit for any period of time, do not cross your legs as this can block blood flow. If you are traveling long distances by car, stop every hour or so and take a walk. If you're on an airplane, stand or walk occasionally. If you can't do this, stretch your shins. Do some exercises. Try raising and lowering your heels while keeping your toes on the floor, then lifting your toes while pressing your heels into the floor.
- Do not smoke. Smoking increases the risk of developing DVT.
- Do exercises and control your weight. Obesity is a risk factor for DVT. Regular exercise reduces the risk of blood clots, which is especially important for people who sit a lot or travel frequently.
Conservative treatment
In cases where the condition of the patient’s vascular bed is not critical, conservative therapy may be indicated. It can stop or slow down the progression of the disease.
A conservative approach is:
- Wearing compression stockings . Thanks to a certain level of compression, the mechanisms of progression of varicose veins are eliminated, swelling disappears, pain and increased fatigue of the limbs are reduced. It is important to choose the correct size of medical knitwear and wear it regularly, as prescribed by your doctor.
- Course treatment with anticoagulants . The minimum duration of taking the drugs is 3 months. Medicines must be taken comprehensively, and the selection of blood thinning drugs is carried out only by a doctor.
- Local application of ointments , taking non-steroidal anti-inflammatory drugs.
- Physiotherapeutic procedures . They are also prescribed by a doctor. They do not have proven effectiveness in terms of treatment, but they help eliminate the unpleasant symptoms of the disease and have a preventive effect.
Often, patients with cardiovascular problems and an increased risk of blood clots are required to undergo annual hospitalization for 2-3 weeks. During this period, they undergo intensive cardiotonic and hemorheological therapy.
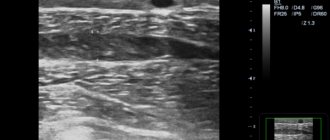
Tests for thrombosis
Laboratory indicators play a significant role in the timely diagnosis of thrombosis.
Thus, guidelines for the management of patients with a new coronavirus infection provide for stratification of the risk of coagulopathy in patients with COVID-19 based on simple laboratory tests: D-dimer, prothrombin time, platelet count, fibrinogen level [1,9]. A clinical blood test can detect inflammation. It also determines the level of platelets, that is, the very substrate of thrombosis.
Additionally, the level of inflammation in the blood and the risk of thrombosis is indicated by an increased level of C-reactive protein.
Biochemical analysis primarily demonstrates blood glucose levels. It can be used to judge the presence of diabetes, one of the most serious risk factors for thrombosis.
Also, a biochemical analysis can determine the level of protein C, which also characterizes the severity of the risk of thrombosis.
Elevated levels of homocysteine in the blood are also a currently proven risk of thrombosis, leading to miscarriage and cardiovascular events (heart attacks and strokes).
D-dimer is a laboratory marker of fibrin formation [8]. It also indicates the presence of inflammation, just like C-reactive protein. The level of D-dimer is a control indicator of COVID-19 and its complications, including those associated with thrombosis.
You can take tests under the comprehensive Thrombosis program, which includes determining the levels of Antithrombin-III, D-dimer and genetic factors of cardiac diseases and platelet levels. This program allows you to determine the fact of thrombosis occurring somewhere in the body, as well as determine the genetic predisposition to it. This program, like other tests, is offered by the CITILAB network of clinics.
Additional determination of homocysteine and C-reactive protein levels will help determine the biochemical risk of thrombosis.
Recovery after thrombosis
Recanalization is the restoration of the capacity of an artery or vein after thrombosis. It can occur through medical intervention or naturally. Recanalization occurs no earlier than after 6 months with long-term treatment. It requires constant prevention.
After thrombosis, the clot in the vein goes away over time and normal blood flow is restored. Sometimes recanalization does not occur. Even after complete cleansing, the vein cannot function normally.
Thrombosis destroys its internal valves, and they are responsible for the outflow of blood in one direction. As a result, the outflow of blood from the limb is disrupted, the pressure in its venous system increases, and the disease develops again. Therefore, signs of recanalization of thrombosis may be short-lived.
Expert opinion
Unfortunately, thrombosis of the veins of the lower extremities has a tendency to recur even after the clot has resolved. Therefore, it is extremely important to make lifestyle changes and follow the preventive measures recommended by your doctor to reduce the risk of recurrent blood clots.
Vascular surgeon, phlebologist
Osipova Ekaterina Yakovlevna
Reasons for development
- Changes in blood composition due to increased viscosity. This happens, for example, with hereditary diseases, oncology, after surgery or serious injuries. Blood viscosity also increases during pregnancy or due to taking medications: hormonal contraceptives, drugs for treating oncology or stopping bleeding.
- Damage to the vessel wall. This happens with injury, burns, serious infection, or after long-term damage to the vascular wall by cholesterol plaques. Radiation or chemotherapy and even the installation of a catheter for administering intravenous drugs also affects.
- Change in blood flow. This can happen with heart rhythm disturbances. Arrhythmias cause turbulence in the blood flow and clots form. Another option is to slow down the blood flow. This happens when there is a lack of movement, for example, after a long flight.
Signs of thrombosis depending on the location of the thrombus
- The portal vein facilitates the flow of blood from unpaired organs in the abdominal cavity (from the stomach, intestines, spleen, pancreas). From them the blood is sent to the liver (where it is cleansed). If thrombosis occurs in the portal vein, the risk of liver disease increases.
Symptoms of portal vein thrombosis include abdominal pain and bloating, intestinal distress, vomiting, rarely black stools, and an enlarged spleen.
- The pulmonary artery becomes blocked after blood flows from the veins of the legs and pelvis. The number of clots, the reaction of the lungs to them and the action of the homeostasis system are important. The smaller the clot, the less severe the symptoms. Large blood clots interfere with gas exchange in the lungs, and hypoxia develops.
Symptoms: chest pain; the skin turns pale and blue; veins swell in the neck; a cough with bloody discharge and wheezing appears; loss of consciousness.
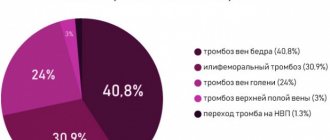
- Thrombosis of the lower extremities accounts for up to 70% of the total number of thromboses. It is especially dangerous when the deep veins in the thighs and below the knees are thrombosed (it is necessary to monitor for signs of lower leg thrombosis). The first symptoms are invisible.
Swelling, pain when walking or bending the lower leg, pain in the inner thigh and foot, reddened skin and cramps are all signs of the development of the disease. If the acute form occurs, the person begins to suffer from shortness of breath, his temperature rises, he becomes dizzy and loses consciousness. You can compare the signs of thrombosis of the lower extremities from the photo, but the diagnosis must be made by the attending physician.
- In the upper extremities, thrombosis is less common (subclavian vein thrombosis), and it is difficult to distinguish its initial symptoms from arm injury. They manifest themselves in swelling, pain and blueness. The patient feels a burning sensation, his hands go numb, and his skin becomes insensitive.
- The vessels of the brain connect with veins and arteries, where blood clots can also appear, and this leads to a stroke. Symptoms of cerebral thrombosis are more pronounced than with thrombosis of other vessels. The disease is accompanied by headaches, dizziness, decreased hearing and visual acuity, loss of consciousness, and periodic convulsions. The person is feeling sick.
- Blood clots also settle in the veins of hemorrhoids, this is considered a complication of hemorrhoids. Signs of thrombosis of hemorrhoids (Haemorrhoids): pain, the affected area itches, fever, swelling.
- The central retinal vein is also affected by thrombosis. Signs of the disease may not be expressed, and the person loses vision as a result.
- Thrombosis of the mesenteric veins of the intestine is manifested by prolonged abdominal pain. Other signs: bloating, high fever, vomiting and nausea. In the early stages, it is difficult to determine the disease by symptoms. Usually they talk about a complication of the pathology.
- If the femoral and iliac veins are affected, then we are talking about ileofemoral thrombosis. It is accompanied by swelling of the legs (the skin changes color from reddish to blue), when pressure is applied, brown marks appear, the legs and groin hurt, and the body temperature rises.
Treatment and diagnosis of venous thrombosis
What is this
Thrombosis is a condition in which blood clots form in blood vessels. If they do not dissolve naturally, they can cause harm. Such clots block blood flow and lead to serious complications. If the thrombus blocks more than three quarters of the lumen of the vessel, then oxygen starvation of the tissue begins. And if completely, it can lead to a heart attack, stroke or limb damage, depending on the location of the formation.
The first mention of thrombosis as a disease appears in 1271, but it was not until the early nineteenth century that scientists linked swelling of the legs with a blood clotting disorder. The phenomenon of thrombosis was understood and described in scientific articles and books by the German scientist and doctor Rudolf Virchow in the mid-nineteenth century. He also formulated the main reasons for its appearance, which are called Virchow’s triad in his honor.