Intracranial pressure
It is simply impossible to imagine a woman interested in children's health issues who has not heard of intracranial pressure - ICP.
Phrases like “we have intracranial” or “we treat intracranial pressure” have become so firmly entrenched in the vocabulary of the average visitor to a children's clinic that many have simply stopped thinking about the meaning of these words.
Nevertheless, the frequency of conversations, the frequency of diagnosis and the frequency of treatment do not at all indicate that the very concept of “intracranial pressure” or the diagnosis of “increased intracranial pressure”, in turn, is understandable to the broad masses of workers.
Although at first glance everything seems obvious. And the essence of the problem (from the point of view of the average person) looks something like this. There is a head. There is a brain inside, blood vessels, there is pressure in the blood vessels - everyone knows this - both grandmother and grandfather have pressure. But grandparents have damaged hearts, but for a child everything is different. The heart is healthy, but the pregnancy was unsuccessful, there was not enough oxygen during childbirth, or the umbilical cord got wrapped around, or some other illness happened, or he hit his head, or they gave him the wrong medicine - so the vessels were damaged, now the pressure in the head is high, hence the heap problems: headache, crying, doesn’t listen to mom, doesn’t sleep well, trembles chin, jerks leg, walks on tiptoes, speaks poorly (wrongly), fights in the sandbox, sucks thumb, refuses to eat and dozens, if not hundreds of other consequences of these injuries -promotions. And since the above complaints and symptoms are possible to one degree or another in almost every child, the presence of, in fact, an epidemic of intracranial pressure becomes easily explained, and this epidemic is gaining momentum. Of course, doctors are actively fighting this, and most children recover safely - thanks to medicine, or as the classic used to say: “Glory, glory to Aibolit! Glory to the good doctors!
A doctor’s attempt to approach the problem of intracranial pressure competently, in a modern way, and to treat it like in the best clinics in the world cannot be implemented. Because the epidemic of ICP treatment that has swept the CIS countries is limited to these countries. That is, our overseas friends are somehow disconnected from this topic - either they misunderstand and do not care about the neurological health of children, or they do not diagnose it, or their children are different?
There must be something wrong here: how can there be a disease that pediatric neurologists in our clinics detect in at least 50% of children (this is the most optimistic figure), and at the same time a disease that is completely absent outside the CIS .
No, the phrase ICP exists, its increase is discussed in scientific articles, moreover, tactics to combat this very dangerous phenomenon are being studied, but the list of conditions accompanied by an increase in ICP is very small, and these are increasingly such terrible horror stories that can be easily made conclusion: having increased ICP, you can sooner end up in the intensive care unit than wait in line for an appointment with a pediatric neurologist at the district clinic.
That is, globally, here and there, the approaches to ICP are fundamentally different: there it is a very rare, very dangerous (life and health threatening) condition, usually requiring hospitalization and emergency care, but in our country it is an extremely common disease, easily diagnosed, almost always easily treatable and almost always on an outpatient basis.
No, something is definitely wrong here. And it seems that we need to figure it out: either we don’t understand something, or we are being misled together, or our children are special - not like those in the rest of the world. Since the last statement seems extremely unlikely, and you don’t really want to be lost and misunderstood, let’s consider the topic slowly and in order.
So, what is ICP and where does it come from? What is the pressure on what and how does it all come out?
In the cranial cavity there is a brain, there is blood, there is a special fluid called cerebrospinal fluid (CSF). Liquor is formed from the blood in special choroid plexuses, circulates, washing the brain and spinal cord, after which it is again absorbed into the blood through special venous sinuses. Liquor performs a number of important functions; without these functions, normal brain function is simply impossible.
Liquor does not stand still, but just like blood, it moves all the time. There are vessels for blood movement. For the movement of cerebrospinal fluid, there are special anatomical cavities - the ventricles of the brain and the spinal canal.
This is, so to speak, elementary, or, to be more precise, superficially primitive anatomical and physiological information.
But now we can understand where intracranial pressure comes from. So, a certain liquid is constantly being formed and is constantly being absorbed. You probably already remembered school mathematics with problems about a swimming pool and two pipes - the same is true with liquor. It flows out of one pipe (choroid plexuses), and flows into another pipe (venous sinuses). While it flows, it puts pressure on the walls of the pool (the inner surface of the ventricles of the brain and the spinal canal).
That's all, actually.
Now for some obvious conclusions.
Everyone has intracranial pressure, just like everyone has noses, hands and butts. The phrase “my child has an intracranial condition” is at least ridiculous and certainly does not indicate that this child has something that others do not have.
Another question is that a specific figure indicating the value of ICP in a specific period of time is not a stable concept, which, in fact, follows from the fact that ICP changes all the time. Both the formation of CSF, and the speed of its movement, and the activity of absorption depend on many factors: whether the child is sleeping or awake, lying, sitting or standing, silent or screaming, normal body temperature or elevated, and in general what the temperature around is - comfortable, or hot, or Cold. The connection between the ICP level and all of the above parameters does not seem obvious at first glance, but an elementary illustration: if the room is hot and the child is actively sweating, blood thickening occurs, as a result, the rate at which the choroid plexuses produce cerebrospinal fluid decreases. It is clear that many manifestations of a wide variety of diseases will, in turn, affect the level of ICP - vomiting, coughing, prolonged crying, painful sitting on the potty due to constipation, and much, much more.
And in this aspect, the analogy between blood pressure and intracranial pressure may be quite appropriate.
In an absolutely healthy child who does not suffer from hypertension at all, the level of blood pressure can fluctuate within a fairly wide range. I went for a run, cried, laughed, got scared - it got better; fell asleep, calmed down, caught my breath - it went down. But the concrete and obvious physiological fact of fluctuations in blood pressure does not make anyone want to run after a child with a tonometer and constantly correct this pressure.
The situation with ICP is exactly the same, but logic and common sense do not answer the elementary question: why is so much attention paid to the level of ICP and its fluctuations? Why is talk about ICP so popular, and its supposed treatment so widespread?
We will give the answer a little later, but now let's talk about really increased intracranial pressure (synonym - intracranial hypertension).
From the point of view of modern, civilized, evidence-based medicine, increased intracranial pressure is one of the manifestations of a number of diseases. Rare and very serious diseases. I emphasize once again: intracranial hypertension is not a disease, not an independent disease, but only a symptom of other very specific and definite diseases. In order for ICP to increase significantly, certain preconditions must be met, for example, a sharp increase in the production of cerebrospinal fluid, which occurs with meningitis and encephalitis. Any damage to the brain substance: stroke, tumor, abscess, injury - also affects all three factors that determine the level of ICP - the production of cerebrospinal fluid, its absorption, and its circulation. Excessive production of cerebrospinal fluid can also be observed in some very serious metabolic disorders, for example in very severe forms of diabetes.
Nevertheless, there is a very specific disease when the increase in ICP is quite tangible - hydrocephalus . Hydrocephalus , as a rule, is associated with congenital abnormalities of the brain, when either there is a very active production of CSF, or the reabsorption of cerebrospinal fluid is impaired, or due to certain anatomical defects its circulation is impaired, or when a combination of these factors occurs. Sometimes hydrocephalus is not congenital, but occurs as a complication after very serious diseases (meningoencephalitis, for example) and neurosurgical interventions.
With hydrocephalus, excess or non-exitable CSF puts pressure on the ventricles of the brain, they seriously expand, the consequence of all this is a rapid increase in the size of the head, a corresponding increase in the size of the fontanelles, and separation of the sutures between the bones of the skull. Hydrocephalus comes in varying degrees of severity. Compensated forms, when mental development does not suffer and symptoms appear moderately, are treated conservatively, with special medications that reduce the production of cerebrospinal fluid and activate its outflow, but in severe cases of the disease, rather complex neurosurgical operations are performed.
It is clear that hydrocephalus does not happen suddenly - that is, a normal child in all respects was walking, and suddenly hydrocephalus happened to you - out of the blue. Hydrocephalus is a congenital disease, and its symptoms appear in the first months of life.
Since the main symptom of hydrocephalus is a rapid increase in head size, measuring head circumference is included in the standards of any preventive examination, starting, of course, from the moment of birth. It is very important to emphasize here that it is not the specific size expressed in centimeters that matters, but rather the dynamics of this indicator. That is, stating the fact that the boy Petya at 3 months has a head circumference of as much as 45 cm is not at all a reason to become depressed and urgently save this boy. But the fact that the head circumference has grown by 7 cm over the past month is already alarming and dangerous, and requires both serious attitude and active control. Let me emphasize once again - not immediate treatment, but control. And if the trend continues, then measures should be taken.
Nevertheless, hydrocephalus, to which we devoted four whole paragraphs, is a rather rare disease and occurs with a frequency of 1 case in 2-4 thousand children. And problems with intracranial pressure are detected in almost every second child - a paradoxical situation...
Here another problem looms. When a child’s head quickly increases in size, the increase in ICP is visible to everyone - it’s so pressing... And when everything seems to be normal, and the doctor looks and says - high blood pressure, it needs to be treated, then how did he know about it? Based on what parameters, indicators, symptoms?
When it comes to an increase in blood pressure in a grandmother, everything seems to be clear here - they took out a device (tonometer) and measured it - yes, hypertension - 190 to 120. We treated it, measured it again - we see that it has definitely become better - 160 to 90 - that means they were treated for good reason and with the right medications... Plus, the improvement was not limited to just changing the numbers. Grandma was really unwell - she had a headache, she couldn’t even get up, but now where is she, exactly? I ran to the store to get some potatoes - well, that certainly means it helped...
And what to do with ICP - where can I get a magic device to show - here, mommy, look how high the ICP is. Here are the medicines - save yourself. Come back in a week, we'll try it on again, we'll see.
And here we have to sadly admit: there is no such device! Neither magical, nor real, nor expensive, nor cheap - there is none!
With all the amazing progress of medical science, with all the variety of special equipment, ICP can be reliably measured in only one way: insert a needle either into the spinal canal (lumbar puncture) or into the ventricles of the brain. After the cerebrospinal fluid begins to flow out of the needle, a simple pressure gauge is connected - a graduated glass tube. The measurement is carried out according to the same principle as in a regular home alcohol or mercury thermometer: the level of liquid (CSF) corresponds to a specific line and a specific number on a glass tube. Cerebrospinal fluid pressure is usually measured in millimeters of water. By the way, it should be noted that until now there is no clear opinion among scientists regarding what ICP should be considered normal. Some say that the norm is from 80 to 140 mm of water. Art., others insist that the normal limits are much wider and the pressure may well fluctuate from 60 to 200 mm of water. Art. The given standards are for a horizontal body position. If the patient is sitting, the norms are completely different.
But the main thing for us is not a specific figure, but a statement of the fact that there are no simple, accessible, convenient and at the same time reliable methods for measuring ICP. It is clear that any talk about punctures in a clinic is simply not serious.
However, there are examination methods that allow one to draw a conclusion about the value of ICP based on a number of indirect signs.
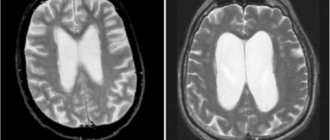
One such method is ultrasound examination of the brain. This method is not used in adults because ultrasound cannot penetrate the skull bones. In children, the situation is completely different, since there is a fontanel - a wonderful window for ultrasound. Neurosonography, which is what ultrasound of the brain is called, is an affordable and absolutely safe method. It allows you to estimate the size of the ventricles of the brain, and an increase in these sizes can well be regarded as an indirect sign of increased ICP. At the same time, as with head circumference, it is not so much the width of the ventricles of the brain that matters, but the dynamics of this indicator.
After the fontanel is closed, the size of the ventricles of the brain can only be seen and assessed using tomography - computed tomography (CT) or magnetic resonance imaging (MRI). At the same time, tomography is a serious, unsafe, expensive method, it is used infrequently - only in cases of real suspicion of serious intracranial pathology.
Another method - outdated, but still widely used - is echoencephalography (EchoEG). Using a special device (echoencephalograph), using the same ultrasound, a number of parameters are assessed, including the pulsation of the blood vessels of the brain. In this case, the amplitude of oscillations of the ultrasonic signal is considered as an indicator capable of assessing ICP.
We emphasize once again: all of the listed methods are not reliable, they do not state, do not confirm, but only admit the possibility, suggest, allow one to suspect an increase in ICP.
This is the result: the examination methods that exist today only give the doctor additional information to think about, but they cannot dot the i’s. This means that you have to rely mainly on specific symptoms. This has its own problems: this is not your grandmother, who, when her blood pressure is high, lies down, and when her blood pressure is normal, runs around shopping. This is a young child, or rather a little month old, who is unreasonable and does not complain about anything in particular.
But the problems are not only due to age and the inability to point with a finger to the place where it hurts. The main problem is that almost all the symptoms that make it possible to suspect an increase in ICP in a child can occur in completely healthy children.
For example, a child’s restlessness, trembling of limbs, and screaming may be manifestations of increased ICP, but may well have nothing to do with ICP at all. And any mother can confirm this, because it is simply impossible to find a child who is always calm and who never shakes anything. Another symptom of increased ICP is strabismus, but it is well known that in children of the first year of life, the extraocular muscles have not yet formed and infant strabismus is often a physiological phenomenon, that is, absolutely normal.
It should, however, be recognized: words such as “anxiety,” “trembling,” “screams,” and “squint” are not capable of seriously frightening the average domestic mother, since everyone hears them and often uses them in everyday life.
It’s a completely different matter when such terrible expressions as “Graefe’s symptom” or “spontaneous Moro reflex” are heard from the doctor’s lips or found in the outpatient card - there is no time for jokes and no time for calm: it is clear that the situation is serious.
Let us try to explain the essence of these wise words.
The essence of Graefe's symptom is the lag of the upper eyelid when the eyeball moves downward. In an additional translation into Russian, this means that when a child looks down and gets scared, several millimeters of the white of the eye are visible above the iris. Looks like a bulging eye. If the child is looking straight, then everything is fine.
The German ophthalmologist Graefe, who lived in the 19th century, described this symptom as typical for patients with goiter (damage to the thyroid gland). In people who do not have goiter, Graefe's symptom can also occur and be a constitutional feature; it can be found in premature infants.
The Moro reflex, or hug reflex, refers to the physiological reflexes of the newborn period. Occurs when hitting the table on which the child is lying, with a sudden loud sound, or when patting the baby on the buttocks or thighs. The reflex consists of two phases. In the first, the child leans back, turns his shoulders, and spreads his arms to the sides. In the second phase, he brings his arms together on his chest. It is clear that the spontaneous Moro reflex is when there were no special external stimuli, and the child throws back his hands... But the absence of “special external stimuli” is a conditional concept. For such a not at all “special”, but quite significant irritant, could well be a doctor’s office - a new environment, an unfamiliar table, a strange aunt-doctor...
It seems that we are completely confused: we promised to explain why the diagnosis of increased ICP and its treatment are so common, but we came to conclusions that were completely opposite. It turns out that additional research methods and examination data in the vast majority of cases do not allow one to confidently diagnose increased ICP. And in situations where such confidence is present, we are almost always talking about extremely dangerous diseases (hydrocephalus, meningitis, tumors, traumatic brain injury) and extremely disturbing symptoms (sharp bulging of the fontanel, disorders of consciousness, vomiting, paralysis).
Let's summarize the main results.
1. Increased ICP is not a disease, but a symptom of certain diseases.
2. Increased ICP is a rare and very dangerous symptom of rare and very dangerous diseases.
3. Treatment of increased ICP has nothing to do with outpatient medicine and almost always requires hospitalization and emergency care.
TTT
To conclude the article, let’s take a break from medicine for a moment and turn to… linguistics. The goal is the curious features of the use of the word “intracranial” itself. The fact is that the phrase “intracranial pressure” in everyday communication among medically savvy mothers is found less and less often. The word “pressure” is omitted as unnecessary, and everyone unanimously “checks the intracranial”, “treats the intracranial” and “complains about the intracranial”.
Specialists in the field of linguistics (linguists) call such things conversion, or the transition of one part of speech to another. This phenomenon is not at all unique. Let us at least recall “ice cream”, “jellied” or closer to medical topics - “laxative”, “ambulance”, “newborn”. Well, who says “sleeping pills” now? Nobody talks, because it’s already clear what they’re talking about. Instead of a children's room - just a children's room, instead of a bakery shop - a bakery that has already become familiar.
The main thing that conversion indicates is the extreme prevalence of a certain word. Conversion in relation to long-suffering intracranial pressure is, alas, a sad phenomenon, because it confirms a rather unpleasant trend: they began to talk about intracranial pressure too often, unreasonably often. This concept is expertly used by the grandmothers on the benches. They will make a diagnosis based on the circumference of the head, more precisely, by the size of the cap, and they also know how to treat. I really wish there were fewer such conversions in our lives. So that the phrase “intracranial pressure” was sometimes uttered by specialists, but grandmothers did not know about intracranial pressure at all, focusing their attention on sleeping pills and aspic.
author Komarovsky E.O. published 06/06/2008 09:08 updated 21/03/2017 — Diseases and treatment
what is birth trauma
Birth trauma is damage to the tissues and organs of a child during childbirth caused by mechanical forces, and a holistic response to these damages on the part of the body.
Conventionally, all traumatic injuries to a child during childbirth are divided into: mechanical (caused by external influences) and hypoxic (due to mechanical influence, the child develops oxygen starvation of the brain, which leads to injury to the central nervous system). In turn, injury to the central nervous system is a consequence of injury to the cervical spine, since when it is damaged, the blood vessels supplying the brain are affected.
Birth trauma can affect different structures of the cervical spine. Depending on its location, there are: trauma to the vertebrae, joints, ligaments; injury to soft tissues (skin, muscles).
Coronavirus in children from 1 year to 5 years
Children aged 1 to 5 years can react to coronavirus infection with a sharp rise in body temperature. Changes in the child's behavior are possible, such as increased moodiness or tearfulness, lethargy and sudden changes in mood.
You can suspect the development of coronavirus in a child based on the following symptoms:
- severe weakness;
- slight cough;
- loss of appetite;
- a sore throat;
- nasal congestion;
- increased body temperature;
- changes in the rhythm and frequency of breathing;
- chest pain;
- dyspnea;
- conjunctivitis;
- gastrointestinal disorder.
The main danger in the form of complications of Covid in children is multisystem inflammatory syndrome (MSI). This is an excessive immune response of the body to the penetration of the virus.
As a rule, DMV develops 1-6 weeks after the acute phase of the disease, even if children have had a mild or asymptomatic form of COVID-19. By this time, in the majority of children who have recovered from coronavirus, PCR tests for covid give a negative result, but antibodies to coronavirus are detected.
As a rule, the first sign of multisystem inflammatory syndrome after Covid in children is a sharp increase in body temperature to high levels (above 38 degrees). Hyperthermia can last for a day or more. A rash may be observed on the body (all over or in certain areas) - macular and/or papular. Characteristic signs of multisystem inflammatory syndrome may include conjunctivitis, scleritis, swollen lymph nodes, and swelling of the palms and feet. One of the common symptoms of DMV is a red or crimson tongue and swollen, bright scarlet lips. The syndrome can lead to damage to the gastrointestinal tract, causing abdominal pain, vomiting, nausea, and diarrhea.
The result of DMVS can be cardiac, renal, hematological, dermatological disorders, as well as damage to the central nervous system, respiratory failure associated with lung damage.
Inflammatory syndrome after covid is more often observed in children from 2 to 5 years old, but older children are susceptible to it.
Most often, coronavirus in children under 6 years of age is asymptomatic . But the asymptomatic course of the disease is not a reason to relax and not monitor the child’s condition. The virus, penetrating the body, causes an immune response and can affect other systems. Therefore, children should be under outpatient supervision of a pediatrician for several months from the onset of infection with a new coronavirus infection.
COVID-19 in children from 6 to 12 years old
Symptoms of Covid in children aged 6 to 12 years are similar to the typical clinical picture of ARVI - sore throat, nasal congestion, cough. A rise in temperature from 37 to 38 degrees occurs more often in them than in younger children. Added to the clinical picture are symptoms in children aged 9 to 12 years, such as aching muscles and joints, conjunctivitis, a purple-red rash, loss of appetite, myalgia (muscle pain) and headache. The course of the disease in children of this age group is more reminiscent of the symptoms of coronavirus in adults. COVID-19 in adolescents
In children over 12 years of age, the classic clinical picture of coronavirus infection is more common. They may develop an intense dry cough, sore throat, runny nose, loss of smell and taste, and distorted perception of odors. Unlike patients in younger age groups, adolescents may experience malaise with headache and muscle pain. COVID-19 is especially dangerous for those teenagers who have previously been diagnosed with heart disease. Under the influence of the virus, the myocardium is damaged, which leads to serious consequences related to the functioning of the heart.
Even if the main symptoms are not observed, it is better to consult a pediatrician , who will prescribe an additional examination and establish the correct diagnosis.
You can call a pediatrician at the Euromed Kids clinic at home by calling +7 812 331 00 00
Are there vaccines for children? Is there a coronavirus vaccine for children?
Currently, none of the available Russian coronavirus vaccines is approved for use in children under 18 years of age, as studies have not been conducted among this age group.
However, on June 22, 2021, the World Health Organization announced for the first time that some coronavirus vaccines may be safe and approved for children. For example, the WHO Strategic Advisory Group of Experts (SAGE) concluded that the Pfizer/BionTech is suitable for use in people aged 12 years and over .
In Russia, clinical studies of the COVID-19 vaccine for adolescents 12-17 years old are planned to be conducted by the Center named after. N.F. Gamaleya. The corresponding tests must be approved by the Ministry of Health of the Russian Federation.
Coronavirus in newborns (0 to 4 weeks) children
To date, there has been no evidence of intrauterine infection caused by mother-to-child transmission. All cases of coronavirus infection are considered acquired after the birth of the baby. As the incidence rate increases, the number of newborns infected by mothers with coronavirus infection has increased. Worldwide, only 5% of all recorded cases of COVID-19 occur in children under one year of age. Most often, infants experience an asymptomatic or mild course of the disease, which may be accompanied by a slight rise in body temperature.
Medical practice describes such symptoms of coronavirus in children in the first weeks of life as “groaning” breathing, increased work of the respiratory muscles, apnea, cough and tachycardia. Sometimes weak sucking, lethargy, regurgitation, diarrhea, and bloating are observed. Cases of covid pneumonia are extremely rare. Most often, a severe form of coronavirus occurs in children with congenital malformations. The risk of complications increases in the case of: prematurity, birth injuries, pulmonary dysplasia and tumors.