Most people are accustomed to thinking that blood pressure (BP) levels need to be monitored only by people over 40 years of age. This opinion arose due to the frequent appearance of the term “hypertension”, meaning an increase in blood pressure levels above normal. Indeed, hypertension is more typical for older patients, however, this pathological condition can occur in representatives of every age group.
There is another concept - “hypotension”, which means a decrease in blood pressure below normal. It occurs more often in children and adolescents, as well as young women. That is why periodic monitoring of blood pressure levels should be carried out for representatives of any age category, including the youngest. Further in the article, we consider what the normal blood pressure is in children of different ages, why it needs to be controlled, and what factors influence the deviation of indicators from the norm.
What is pressure and what does it depend on?
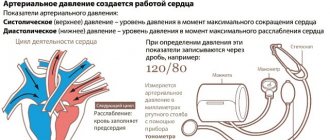
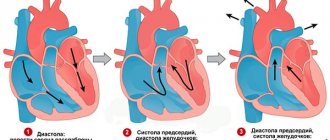
The flow of blood through the vessels of the human body occurs due to its release from the heart and the pressure difference in vessels of different diameters (arteries, veins and capillaries). With each contraction of the heart muscle, a certain amount of blood is released under pressure into the aorta (the largest artery) and the pulmonary trunk. The rhythmic work of the heart ensures periodic fluctuations in blood pressure levels: an increase in values during contraction (systole) of the heart and a decrease during the period of relaxation (diastole).
The highest numbers are recorded during systole, which is why this pressure is called systolic (upper), the minimum during diastole, which means this pressure is called diastolic (lower). Blood pressure levels depend on the age group of the population a person belongs to. Blood pressure in children is lower than in adults. This is explained by the fact that in children and adolescents the walls of the arteries are more elastic.
And also lower rates in childhood are explained by low vascular tone, the presence of short and straight capillaries, as a result of which peripheral resistance decreases. During puberty, a number of changes occur in the body, during which the adolescent’s heart grows faster than the blood vessels. As a result, so-called juvenile hypertension occurs, in which the upper pressure increases to 140 mm Hg. Art., however, this condition is temporary.
No ads 1
Diagnostics
To make a diagnosis, first of all, blood pressure measurements are needed. This is usually done in a sitting position for the first half. The measurement occurs three times, the interval between these is three minutes. Also, it is not done immediately after mental or physical stress, but after an hour has passed. In addition, the following diagnostic methods are used: ECG, ECHO-kg, ABPM, study of autonomic homeostasis, EEG registration, psychological testing, clinical and biochemical blood tests, consultation of the necessary specialists in order to exclude secondary arterial hypotension. To confirm the diagnosis of arterial hypertension, daily monitoring and tests with different types of stress are used. During the study, it is important to identify the cause of the increase in pressure if hypertension is secondary. This is what helps the doctor prescribe effective treatment. If the cause of hypertension is not eliminated, treatment measures will not give the desired effect, the result will be temporary.
Indicators in a newborn and infant
What blood pressure should a child have under one year of age (mm Hg):
- From birth to 14 days – 60-95 (systolic), 40-50 (diastolic).
- From 14 days to 1 month – 80-115 (systolic), 40-75 (diastolic).
- From 1 month to 1 year – 90-115 (systolic), 50-75 (diastolic).
Neonatological and pediatric standards say that you can quickly calculate whether the systolic pressure is normal in a child under one year old using the following formula: 76 + 2n, where n means the baby’s age in months. The diastolic reading should be 1/3–1/2 of the systolic reading.
Standard “home” tonometers are not used to measure blood pressure in newborns
In newborns, a sharp decrease in blood (arterial) pressure is often associated with the development of a state of shock, the causes of which may be:
How to measure your own blood pressure with a mechanical tonometer
- Internal bleeding.
- Birth injury.
- Sepsis.
- Hemolytic disease of newborns (edematous form).
- Severe form of asphyxia.
- Congenital heart defects.
- Severe respiratory distress syndrome.
- Heart failure.
- Hemorrhage into the adrenal gland.
- Pneumothorax, etc.
In such cases, in addition to a decrease in blood pressure, the child experiences pale skin, an increase or, conversely, a decrease in heart rate, and shortness of breath. The lower extremities become cold, urine output is sharply reduced or completely absent.
Important! Most often, a decrease in blood pressure is observed in premature sick children.
Arterial hypertension (increased blood pressure) is not typical for full-term babies who were born healthy. The pathological condition is considered secondary, since it occurs against the background of certain diseases, for example, pathology of the renal apparatus and ureters, patent ductus arteriosus, bronchopulmonary dysplasia. Blood pressure increases in a newborn if the mother took steroid drugs during pregnancy or the baby was prescribed indomethacin after birth.
Symptoms of increased blood pressure in a newborn include irritability and general restlessness, unmotivated crying, shortness of breath and attacks of apnea (short-term cessation of breathing), and convulsions. Adequately selected treatment can return the child’s blood pressure to normal.
No ads 2
Pulse rates
To count a child's pulse, you need to have a simple stopwatch. It is inconvenient to measure the pulse on the hand of a newborn baby, so you will have to place your fingers on the carotid artery.
Before measuring the pulse, the child must be calm and in a comfortable position. Find the artery and feel the pulse. Now mark 60 seconds on the clock and start reporting the beats. Babies have a fairly fast pulse, sometimes even arrhythmic.
| Child's age | Average value | Normal heart rate per minute |
| First month of life | 140 | 110 – 170 |
| From a month to 1 year | 132 | 102 – 162 |
| From 1 year to 2 years | 124 | 94 – 154 |
| From 2 to 4 years | 115 | 90 – 140 |
| From 4 to 6 years | 106 | 86 – 126 |
| From 6 to 8 years | 98 | 78 – 118 |
| From 8 to 10 years | 88 | 68 – 108 |
| From 10 to 12 years | 80 | 60 – 100 |
| From 12 to 15 years | 75 | 55 – 95 |
| From 15 years old | 70 | 60 – 80 |
Study carefully the child’s heart rate in the table by age. Having found the desired age, calculate how many beats per minute the baby should have.
Absence of normal and increased heart rate in a child by more than 20% are symptoms of tachycardia. In general, such symptoms with anxiety, physical activity, fever, blood loss and other problems in a child are normal.
On the contrary, discrepancies with the data in the tables when the pulse slows down by more than 20% of normal are symptoms of bradycardia, a more serious problem that can manifest itself due to shock or heart pathology.
Accelerated
During physical exercise and emotional outbursts, the child experiences an increase in heart rate. The rate of such acceleration can exceed normal rates by 3 - 3.5 times. If the pulse accelerates at rest, then the child has symptoms of tachycardia. Tachycardia appears due to fatigue or previous illnesses and requires treatment.
Delayed
If a child's heart rate is less than 60 beats per minute at rest, these are symptoms of bradycardia. Such signs in the absence of pathologies are the norm. In this case, treatment is not required. Professional athletes, especially swimmers who train their endurance, have a heart rate that does not exceed 40 beats per minute.
If a slow pulse is accompanied by dizziness, severe fatigue and high blood pressure, the child should be shown to a specialist.
When playing sports
During training, the curator must pay attention to the child’s health status. Trainers offer little athletes to count their pulse at the beginning of the lesson and after it ends. In such cases, you need to monitor not only the number of beats, but also their rhythm. Loads affect the frequency of impacts. The greater the load, the more actively the child’s heart works.
There is a special formula for calculation, with which you can find out which pulse does not deviate from the norm: X = 220 - the age of the child. The value must not be exceeded.
Blood pressure in a child from 1 year to 12 years
The level of blood pressure in the period from 1 year to 5 years practically does not change. Average systolic pressure is 100–115 mm Hg. Art., diastolic – 60–75 mm Hg. Art. Normal baby blood pressure:
- From 6 to 9 years – 100–125/60–80 mmHg. Art.
- From 9 to 12 years – 110–125/70–85 mm Hg. Art.
The formula for calculating upper blood pressure in children after one year is: 90+2n, where n means the number of years. Diastolic should be 1/3–1/2 of the upper value. Up to 5 years of age, blood pressure levels do not depend on gender differences. 6–9 years is the period when boys’ numbers increase by 2–5 mm Hg. Art. more than for girls, and for 9–12 years old it is the other way around.
A persistent increase or decrease in indicators should be alarming, since children usually do not suffer from primary forms of arterial hypo- and hypertension. Any recorded numbers must be rechecked several times throughout the day.
Hypotension
If there are no clinical manifestations, you can think about the physiological variant of hypotension, which does not require medical intervention. This occurs in children with asthenic physique, as well as those who play sports or move actively throughout the day. The pathological form of the condition is manifested by weakness, decreased performance, lack of desire to do favorite things, dizziness, and increased heart rate.
The reasons for a decrease in blood pressure in children aged 1 to 12 years can be various types of anemia, blood loss of varying intensity, pathologies of the thyroid gland, adrenal insufficiency, heart and vascular diseases, as well as overdose of certain medications. The danger of the condition lies in the slowing of blood circulation, which, in turn, leads to the fact that the body tissues do not receive enough oxygen.
Hypertension
There are two main forms of hypertension: primary, the cause of which could not be reliably determined, and secondary, the provoking factor of which was a specific disease. The danger of increased blood pressure is possible damage to the heart, kidneys, retina and brain. And the risk of stroke and heart attack also increases significantly. For a long period of time, parents may not even suspect that their child is developing hypertension.
A sedentary lifestyle is a factor influencing changes in blood pressure readings
Characteristic symptoms:
- Headache.
- Dizziness.
- Sensation of pulsation in the temples.
- Noise and ringing in the head.
- The appearance of "floaters" before the eyes.
Later, visual acuity may decrease, the number of trips to the toilet becomes more frequent, and painful sensations appear in the heart area.
Features of treatment
If deviations from the norm are identified, it is necessary to eliminate all provoking factors: balance the diet, lose excess weight, and add regular exercise.
To lower blood pressure, an atherogenic nutritional profile is required, in which foods are selected in such a way as to reduce the progression of the disease and restore normal metabolism, including lipid metabolism. These are seafood, lean fish, meat, nuts, citrus fruits.
In addition, salt intake is limited to 5 g. The teenager is advised to swim and walk. These simple measures can reduce blood pressure by 5-8 units. In this case, you need to regularly monitor your blood pressure, recording your readings daily.
Traditional recipes, agreed upon with a doctor, require stabilization of arterial parameters. They recommend tea made from rosehip, barberry, and calendula. Freshly squeezed juices of carrots, beets (be sure to dilute with water), lingonberries. Ready-made pharmacy tinctures of hawthorn, motherwort, valerian. For teenagers with discomfort in the heart area, compresses with mustard or apple cider vinegar are applied to the chest.
Only if high blood pressure is resistant to general health measures, herbs, and a balanced diet, the child is treated with medications. The general principles of therapy are as follows:
- use long-acting metabolic antihypertensive drugs;
- the choice of starting agents is dictated by the cause of hypertension;
- the complex necessarily involves ACE inhibitors (angiotensin-converting enzyme inhibitors), they act on the renin-angiotensin system, which secretes angiotensin II, known as one of the most effective hypertensive agents;
- impaired renal function dictates the use of drugs excreted by the liver;
- they begin treatment with minimal doses, and if there is no result, they begin to combine drugs;
- be sure to combine antihypertensive therapy with the prescription of correctors of lipid, carbohydrate, purine metabolism, and antiplatelet agents in order to normalize microcirculation;
- long-term therapy.
Treatment is carried out under the supervision of a doctor. Apply:
- ACE inhibitors (ACE inhibitors): Fosinopril, Spirapril, Omapatrilat;
- calcium channel blockers: Lercanidipine, Nifedipine, Nimodipine;
- beta blockers: Betaxolol, Carteolol, Labetalol;
- diuretics: Hypothiazide, Veroshpiron, Triampur, Spironolactone;
- sedatives: Novopassit, Afobazol, Elenium.
Sympatholytics, adrenergic blockers, and direct vasodilators are currently not relevant in the treatment of hypertension in adolescents.
Each class of medications has its own advantages and contraindications. The choice of drug is made taking into account the cause of hypertension, blood pressure, the patient’s age, and concomitant diseases.
Hypotension is a different story: there is no talk of any traditional treatment. If decoctions and dietary supplements are prescribed, then only from a pharmacy, with a doctor’s prescription. Alcohol tinctures of eleutherococcus, lemongrass, ginseng, echinacea or immortelle. The dosage is of great importance here, so making your own is excluded. In the first place is changing the teenager’s lifestyle.
Normalization of the microclimate in the family, school, and sports team relieves teenage hypotension very well. The correct daily routine, good, sound sleep, a contrast shower in the morning or tonic baths, sufficient rest, alternating with dosed physical or mental activity are the keys to success. You should limit computer games and watching movies.
At home, ginger tea with honey, cinnamon, strong black sweet tea, coffee, and hot chocolate are useful. Hypotension means salty food; sometimes a roach or a sandwich with herring, pickled cucumber, or tomatoes are enough to normalize blood pressure. At the same time, water accumulates in the body, which fills the bloodstream, increasing the volume of circulating blood, increasing blood pressure on the vessels, automatically raising pressure.
Hippotherapy, swimming with dolphins, and simple communication with pets give excellent results. All physical activity is selected under the supervision of a doctor, taking into account concomitant pathologies. Massage of the collar area and hands is possible.
Medicines are used as a last resort. Recommend:
- Adaptogens – strengthen, stimulate, have high biological activity: rosea radiola, ginseng, mumiyo, vitamin and mineral complexes;
- Nootropics - support higher mental brain functions, improve attention, encourage the study of new material: Nootropil, Cerebril, Lucetam, Oykamid;
- Antidepressants - reduce tension, improve mood: Afobazol, Prozac, Paxil;
- Tranquilizers – relieve anxiety and fear: Diazepam, Phenazepam, Mebicar.
All medications are taken in dosages that are appropriate for age.
Teenage years
We are talking about the age of 12–15 years. Normal numbers during this period can be seen in the table.
| Age | Upper (mm Hg) | Lower (mmHg) | ||
| Minimum | Maximum | Minimum | Maximum | |
| 12, 13, 14, 15 years | 110 | 135 | 70 | 85 |
In parallel with blood pressure readings, it is necessary to measure the heart rate (pulse). For the puberty period, the optimal numbers are 55–95 beats/min. Imperfect regulation of autonomic functions, which is typical for adolescence, explains frequent surges in blood pressure. At this time, the body of boys and girls experiences serious overloads, which are also reinforced by changes in hormonal levels. Changes in blood pressure in adolescents are manifested by both its increase and decrease.
In girls, hypertension can be observed from the age of 12, in boys - later, from the age of 14. The most common cause is probably excess levels of adrenaline and aldosterone. A large amount of hormones provokes vasoconstriction, which causes the development of hypertension. Symptoms of the condition may be absent or mild. Provoking factors are also considered to be an irregular daily routine, insomnia, spending a lot of time at the computer, and excessive stress on the body (for example, participation in sports competitions).
Hypotension can also be observed in completely healthy children, for example, after overeating, when being in a stuffy room, in adolescents with an asthenic body type. Low physical activity and prolonged exposure to stress can also be reasons.
No ads 3
Hypotension
Low blood pressure does not have the best effect on your well-being. The disease is diagnosed if the values of systolic and diastolic pressure are underestimated from the normal limits by 15 mmHg. Art. Most parents associate the first symptoms of low blood pressure with overwork at school. The child becomes lethargic, loses interest in studying, complains of a headache that is localized in the temporal region, weakness and nausea.
One of the symptoms of hypotension is loss of appetite
As the disease progresses, the symptoms intensify, fainting begins, during which the child can be injured, for example, hit his head. Before losing consciousness, the child turns pale, pain occurs in the abdomen, the eyes become dark, the muscles become weak, and there is not enough air. Consciousness is usually restored after fainting on its own. In some cases, emergency assistance is necessary.
The reasons for the development of hypotension are as follows:
- Hereditary predisposition (the tendency to low blood pressure is most often passed on to the child on the maternal side).
- Complications during childbirth (hypotension usually develops in premature babies, as well as children whose mothers suffered from low blood pressure during pregnancy).
- Climatic conditions (pressure is traditionally low among residents of high mountain areas).
- Lack of essential microelements and vitamins in the diet.
- Salt-free diet.
- Accelerated or delayed physical development, as well as physiological characteristics (hypotonia is typical for people of asthenic physique).
- Chronic diseases and pathologies (diabetes, heart and kidney failure, heart defects).
If blood pressure is usually normal, and attacks of hypotension occur sporadically, it is necessary to find out what causes the condition. Perhaps the child is overtired due to workload at school or plays intense sports. Girls are more likely to experience low blood pressure at primary school age. Signs of hypertension are more often diagnosed in boys.
Recording indicators
Diagnosis of arterial hypo- or hypertension is based on threefold measurement of indicators. To correctly measure blood pressure in children, it is necessary to select a tonometer according to the child’s age. The table values will help you choose the optimal cuff width, according to the All-Ukrainian Health Organization.
| Age category | Cuff width (cm) |
| Newborns and infants | 2,5 |
| 1–3 years | 5–6 |
| 4–7 years | 8–8,5 |
| 8–9 years | 9 |
| 10–13 years | 10 |
| 14–16 years old | 13 |
How to measure blood pressure in children and adolescents:
- It is necessary to give the child time to adapt to the conditions in which the measurement will take place (5–10 minutes).
- The arm on which the measurement will be taken should be at heart level, the back should rest against the back of the chair, and the legs should not be crossed. The sleeve should not squeeze the arm above the place where the cuff is fixed.
- The stethoscope is applied to the area of the ulnar fossa at the site of the projection of the brachial artery.
- The cuff is fixed 2.5 cm above the cubital fossa. Close the bulb valve, making sure that the readings are at 0 mmHg. Art.
- Inflate air into the cuff until the pulsation disappears, adding 20–30 mmHg. Art. Next, the valve of the bulb is slowly opened, carefully monitoring the number at which the pulsation becomes audible again. This is the first indicator - systolic pressure.
- The moment the pulsation disappears is the second indicator (diastolic pressure).
- Record the indicators on paper or in medical documentation.
Subtleties of measurement
You can rely on the accuracy of the indicators obtained during measurement only if the following recommendations are followed:
- Blood pressure in children (as well as in adults) is not measured directly after eating.
- The manipulation is carried out only after the child has rested for at least half an hour - an hour after physical activity.
- To measure blood pressure in a child, a special cuff is used that corresponds to the width of the small patient’s arm.
- The arm should be extended, palm facing upward.
- When fastening, it is necessary to leave a space between the hand and the cuff into which the finger can freely pass.
Are measurements being taken for the first time? Do not be nervous when you see numbers on the tonometer monitor that differ from the norm. The reason that caused blood pressure fluctuations could be a change in weather, nervous stress, and even certain foods. You can clarify the results by measuring the pressure on the other arm after 4-10 minutes. The most accurate value will be the minimum value.
Important! If blood pressure rises or falls regularly, and the child’s well-being causes some concern, you should contact a specialist who will prescribe an examination and be able to determine the cause of the condition.
By eliminating fast food, fast carbohydrates, and sweet soda, you can prevent obesity, which traditionally accompanies pressure changes
How to avoid blood pressure surges in children
It is important to follow the following recommendations from experts. First of all, it is necessary to change the child’s daily routine, spend more time in the fresh air, get full sleep at night; daytime sleep is also important for children. In the morning, it is advisable to do light exercises so that the body has time to wake up.
Blood pressure is an important indicator that must be monitored even in childhood
The next step is to normalize your diet. Children, left without parental control, love to eat fast food, chips, and nuts. It is important to explain that such food is not good for the body. You should increase the amount of fruits and vegetables consumed, cereals, dairy products, and reduce salt intake (the last recommendation for hypertensive patients).
If you are prone to hypertension, massage of the collar area, head and face is useful. For hypotension – lumbar region, abdomen, buttocks and lower extremities. And experts also recommend paying attention to water procedures: for hypertension, warm baths with herbal infusions and decoctions are considered useful; for hypotension, on the contrary, a contrast shower is needed, which will have a tonic effect. And experts may also advise giving the child medications that are prescribed on an individual basis.
How to normalize blood pressure
{banner_banstat4}
Blood pressure should always be within age norms. If frequent jumps down or up are observed, specialists prescribe special treatment and adjust the child’s lifestyle.
Table “Methods of normalizing pressure”
| How to lower blood pressure | Follow the daily routine. Getting up in the morning and going to bed at night should be at the same time every day |
| Limit the consumption of pickled and canned foods. Reduce the daily dose of salt (food should be lightly salted) | |
| Improve your sleep. The need for a child’s body to sleep at night is at least 8–9 hours a day. Preschool children should be put to sleep during the day (1.5–3 hours) | |
| Treatment with antihypertensive drugs (diuretics, antispasmodics, calcium channel blockers, ACE inhibitors). Medicines are selected by the doctor individually, based on the underlying disease | |
| Avoid overwork. Physical activity should be moderate, and training should be dosed | |
| Maximum limitation of stress factors, emotional stress | |
| Spend more time outdoors | |
| In adolescence, avoid the abuse of weak alcoholic drinks and smoking | |
| How to increase blood pressure | Balance the diet so that the young body receives all the necessary substances. The child should eat more fruits, vegetables, meat, fish, dairy products, legumes and cereals. Meals must be divided into fractions (5–6 times a day) |
| To live an active lifestyle. Running, swimming, cycling, gymnastics, and dancing help increase low blood pressure. The main thing is to take into account the interests of the child | |
| Strengthen the body's defenses. Long walks in the fresh air (at least 40 minutes) and good nutrition will help with this. | |
| Use adaptogens (after consultation with your doctor). Tincture of lemongrass, ginseng or eleutherococcus increases the tone and elasticity of blood vessels | |
| Use physical therapy. A contrast shower and underwater massage help a lot. Normalization of pressure using similar methods occurs after 7–10 sessions | |
| Massotherapy. Conducted by a specialist. Restores normal functioning of the heart, blood vessels and nervous system, stabilizes blood pressure |
Preventive measures and specific therapy help restore normal functioning of the heart and blood vessels, strengthen the defenses of the young body and improve the general condition of the child. The main thing is to first examine and identify the causes of deviations, and then begin treatment.
Differential diagnosis of poisonings accompanied by miosis
| Symptoms | Psychoactive substances | |||
| Opiates | Ethanol | Barbiturates | Benzodiazepines | |
| Pupil | Miosis | Miosis | Miosis | Miosis |
| Level of consciousness | Oppressed to coma | Excitement gives way to depression | Drowsiness, coma | Drowsiness, coma |
| Skin and mucous membranes | Pale, wet, sticky | Hyperemia gives way to pallor. Profuse sweating, hypersalivation. | “Barbiturate burn” - bubbles at the point of pressure | Sweating |
| Convulsions | Eat | Possible (a dangerous harbinger of coma) | No, muscle relaxation | No, muscle relaxation |
| Heart rate, pulse | Bradycardia, then thready pulse | Tachycardia gives way to bradycardia | Not changed | Not changed |
| HELL | Hypotension | Hypertension then hypotension | Hypotension | Hypotension |
| Breath | Depressed to the point of apnea | Tachyhypopnea | Oppressed | Oppressed |
| Pulmonary edema | Available | No | Eat | Eat |
| Bronchorea | No | No | No | No |
| T body | Demoted | Not changed | Not changed | Not changed |
| Abdominal pain | No | No | No | No |
| Dyspepsia | Vomit | No | Nausea, vomiting | Nausea, vomiting |
Differential diagnosis of poisonings accompanied by mydriasis
| Symptoms | Psychoactive substances | ||||||
| Tricyclic antidepressants | Cocaine | Ecstasy | Amphetamines | Hashish | LSD | Mushrooms are hallucinogens | |
| Pupil | Midriaz | Midriaz | Midriaz | Midriaz | Midriaz | Midriaz | Midriaz |
| Level of consciousness | Visual hallucinations, depression of consciousness up to coma | Excitement auditory hallucinations | Excitement, panic, delirium | Inducing psychosis | Excitement, possible hallucinations, delusions | Excitement, panic, hallucinations rave | Visual and auditory hallucinations |
| Skin and mucous membranes | Dry mucous membranes | Sweating, paleness, scratch marks, “cocaine bugs” | Sweating | Regular | Injected scleral vessels | Sweating | Sweating, hypersalivation |
| Convulsions | Possible | No | Reduction of jaws | No | Muscle reduction | No | No |
| Heart rate, pulse | Tachycardia, sudden cardiac arrest | Tachycardia | Tachycardia | Tachycardia | Tachycardia | Tachycardia | Bradycardia turns into tachycardia |
| HELL | Not changed | Hypertension | Not changed | Hypertension, then hypotension | Hypertension | Hypertension | Hypertension |
| Breath | Oppressed | Cocaine runny nose | Not changed | Bronchodilation | Not changed | Not changed | Not changed |
| Pulmonary edema | No | No | No | No | No | No | No |
| Bronchorea | No | No | No | No | No | No | No |
| T body | Hyperthermia | Hyperthermia | Hyperthermia | Hyperthermia | Not changed | Fever | Fever |
| Abdominal pain | Intestinal paresis | No | No | No | No | No | Eat |
| Dyspepsia | No | No | No | Nausea, vomiting | No | Nausea | Nausea, vomiting, diarrhea |
| Exicosis | No | No | Eat | No | No | No | Eat |
| Vision | Spasm of accommodation | Not changed | Not changed | Not changed | Not changed | Not changed | Diplopia |
Volume of liquid for gastric lavage
| Age | Single (ml) | Total (ml) |
| Newborn | 15-20 | 100 |
| 1 – 6 months | 60-100 | 500 |
| 7-12 months | 110-150 | 1000 |
| 2-5 years | 200-350 | 3000-5000 |
| 6-10 years | 350-450 | 6000-8000 |
| 11-15 years | 450-600 | 6000-10000 |
| Adults | 5-10 ml/kg | 2-5-10x |
Maximum volume of colloid infusion in the prehospital setting
| Age | Amount of solution in ml |
| up to 1 year | 200 |
| 1-5 years | 200-400 |
| 6-10 years | 400-600 |
| 11-15 years | 600-800 |
| 15 years and older | 1000 |