At the initial appointment with a specialist, the patient is given the first measurement of arterial parameters, using a mechanical, semi-automatic or automatic device for measuring blood pressure - a tonometer.
Considering that restoration of intravascular tension can take years, the patient will need to purchase his own blood pressure measuring device in order to determine the cause of poor health in time and take medications.
A tonometer is a modern medical device used for non-invasive measurement of blood pressure (the device causes pain and does not violate the integrity of the skin during examination).
Thanks to this equipment, you can control blood pressure painlessly, quickly and without the help of medical personnel, and avoid complications that can lead to hypotension or hypertension.
Devices for measuring blood pressure non-invasively are divided into several types, this greatly simplifies their operation. Today, semi-automatic and automatic blood pressure monitoring devices are in demand, but the mechanical one is also not inferior to its improved counterpart. Let's consider all the features and advantages of pressure measuring devices: which one is better? It is important to decide how to choose a device that performs high-performance blood pressure measurement.
Why do you need to measure blood pressure?
Blood pressure is the force of blood with which it acts on the walls of arteries and blood vessels.
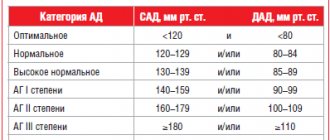
There are diastolic (lower) and systolic (upper) pressure. The norm for an adult is around the boundaries of 120 to 80 mmHg. Significant deviations from these figures often signal the emergence of some disease. Jumps in blood pressure increase the risk of heart attack, ischemia, and stroke.
Increased levels can be observed with the development of the following pathologies:
- heart rhythm disturbances;
- vascular diseases;
- renal failure;
- endocrine diseases;
- neurological disorders.
Low blood pressure is caused by: internal hemorrhages, heart failure, aggravated stomach ulcers, stress, vegetative-vascular dystonia, depression.
It is worth noting that reduced levels may be an individual characteristic of the body. However, high blood pressure almost always signals problems in the body.
To find out exactly the reasons for the jumps, you need to regularly monitor your condition, take measurements, and be examined by a doctor.
Daily blood pressure monitoring - who is prescribed and why, interpretation of results
What is it and how is it done?
Daily blood pressure monitoring is an instrumental study that monitors this indicator throughout the day. It is carried out like this: a cuff is placed on the patient’s shoulder to measure blood pressure. Using a special tube, the cuff is attached to the recorder. This small device pumps air into the cuff at regular intervals and then releases it. During the day, measurements are usually taken every 15 minutes, at night - after 30 minutes. A sensitive sensor determines the time of appearance and attenuation of pulse waves (as with conventional Korotkoff pressure measurement). The results are recorded in the device's memory. After reading them using a computer program, the functional diagnostics doctor analyzes the results and gives a conclusion.
What will this study show?
The study shows a number of important implications for human health.
- Maximum and minimum blood pressure (systolic and diastolic) during observation in the patient's natural environment, and not in the hospital.
- Average blood pressure during daytime and nighttime hours, which will determine whether the patient has hypertension. This is the main indicator for which the study is conducted.
- Circadian rhythm of blood pressure. Failure to lower blood pressure at night is associated with an increased risk of heart attack and stroke.
All this data will help make a diagnosis of hypertension and select the right treatment, and then evaluate its effectiveness.
About self-measurement of blood pressure
Constant self-measurement of blood pressure will provide much less valuable information. It cannot be carried out at night. If a person wakes up on purpose, this leads to an inevitable increase in pressure and distortion of the results.
You need to know that the most accurate results are obtained by measuring the traditional Korotkoff method (determination of tones using a phonendoscope). It is best to use semi-automatic devices with automatic air injection, since manual injection can cause a short-term increase in pressure. Devices that measure pressure on the wrist or finger are much less accurate. We recommend devices that operate on mains power rather than on batteries.
It should be taken into account that in approximately 5% of patients, pressure monitoring indicators differ significantly from self-monitoring data. Therefore, it is very important to carry out control measurements in the diagnostic room immediately after the start of the study.
How to prepare for research?
On the recommendation of the attending physician, certain medications for the treatment of hypertension may be discontinued before monitoring. If there are no special instructions, you must take all medications as usual. It is advisable to wear a light T-shirt with sleeves up to the elbow, and some loose clothing on top, since the recorder will be placed in a bag and hung around your neck, and there will be a cuff on your arm.
In some cases, it is recommended to bring batteries for the device. Alkaline (alkaline) batteries required.
Before the study, you can eat, drink, and lead a normal lifestyle.
How to behave during research?
Detailed instructions are given by the functional diagnostic nurse. She should give the patient a diary in which he will note his actions and sensations during each blood pressure measurement (except for sleep time), as well as taking medications and sleep time.
At the beginning of each measurement, the patient should stop and extend his arm down along the body, relaxing it. After completing the measurement, the subject must make an entry in the diary and continue the interrupted lesson. If the cuff slips, you need to carefully adjust it. The tube through which air is pumped must not be allowed to bend.
The increase in pressure in the cuff is often quite severe, resulting in pain when squeezing the arm. These feelings must be tolerated.
Indications for research
- “Borderline” blood pressure figures identified during repeated measurements using the Korotkov method.
- Monitoring of selected antihypertensive therapy, including to exclude episodes of severe hypotension after taking medications.
- Suspicion of “white coat hypertension”, when high blood pressure is recorded only when measured by medical staff. Suspicion of “workplace hypertension,” when increased blood pressure occurs at work.
- Severe hypertension resistant to treatment.
Who is recommended to undergo the study?
In the presence of the listed indications, especially valuable information can be obtained from the following groups of patients:
- Pregnant women.
- Patients with type 1 diabetes mellitus.
- “White coat hypertension” and “workplace hypertension.”
- Episodes of hypotension.
- Young people with disorders of the autonomic nervous system.
- Older patients.
- Patients suffering from hypertension without treatment effect.
Contraindications for the study
- Exacerbation of skin disease at the site of application of the cuff.
- Disturbances in the blood coagulation system with a tendency to bleeding during exacerbation.
- Injuries to both upper extremities, excluding the possibility of compression by a cuff.
- Impaired patency of the brachial arteries, confirmed instrumentally.
- Patient refusal.
- The study may be useless if there are significant disturbances in heart rhythm, as well as very high blood pressure values (more than 200 mm Hg).
What is Holter?
During the examination, a special portable device is used - Holter. Its electrodes are attached to the patient’s chest; they record all changes in blood pressure and record an ECG throughout the day.
The diagnostic device is named after Norman Holter, a famous American biophysicist researcher. In 1961, he developed a monitoring technique and put it into practice for the first time. Thanks to the Holter method, today cardiologists can identify disturbances in the functioning of the heart and various hidden diseases that are not visible on a regular electrocardiogram.
Why do you need daily ECG monitoring (Holter)?
Holter monitoring can be prescribed by a cardiologist or a general practitioner in order to confirm the diagnosis, check the effectiveness of treatment, discontinue medications, clarify details, etc.
The Holter method allows you to identify:
- Ischemic ECG changes.
- Heart rate.
- Type of heart rhythm.
- Heart rhythm disturbances: pauses, ventricular extrasystoles and others.
A regular cardiogram is significantly less informative than 24-hour monitoring, since although it can detect heart disease, it is not capable of assessing the frequency of its occurrence and the severity of its course. It is easier for the doctor to select adequate therapy after analyzing the Holter ECG results.
Who is recommended for 24-hour ECG monitoring (Holter)?
Typically, the electrodes of the device are installed in patients for a day; if nothing could be recorded within 24 hours and no deterioration occurred, then the monitoring is extended (maximum period of 7 days).
Indications for use:
- Coronary heart disease of various forms: silent myocardial ischemia, Prinzmetal angina, etc.
- Studies of heart rhythm disorders: Parkinson's, Wolff's, White's syndrome, atrial fibrillation, as well as ventricular tachycardia and sinoatrial block.
- Arterial hypertension.
- Heart defects.
- Treatment control
- Scheduled preventive examination.
In addition, daily ECG monitoring is prescribed if there are patient complaints of discomfort in the left side of the chest, a feeling of a sinking heart, fainting, or a feeling of lack of air. Diagnostics for frequent dizziness is also indicated.
There are no contraindications for diagnosis, except perhaps skin lesions in the chest area, which will complicate the procedure for attaching electrodes.
How is the examination carried out?
In the diagnostic room, special disposable electrodes in the amount of 5-7 pieces are fixed to the patient’s chest with an adhesive plaster (depending on the Holter model). Using a wire, the sensors are connected to a recording device. The device is in a special case and is hung on the patient’s neck or belt.
The specialist will provide instructions on how to use Holter and give the patient an observation diary. It must indicate all the events that occurred with the person being examined: deterioration and improvement of the condition, taking medications, physical activity, nighttime, as well as daytime rest. Data must be recorded with precise time reference.
To see how the cardiovascular system reacts to stress, during the study the doctor may advise the patient to walk up the stairs. This will help find a connection between complaints and changes in the electrocardiogram.
Important! If the patient experiences any interruptions in the heart’s function within 24 hours, the rhythm increases for no reason, dizziness or other complaints appear, this must be recorded in the diary.
During diagnosis, you cannot undergo magnetic resonance imaging and x-rays of organs. A day later, the doctor removes the electrodes and deciphers the data obtained.
Monitoring - indications, installation, results, harm
Holter monitoring is a method of functional diagnostics that allows for daily monitoring of the electrocardiogram. ECG recording is carried out continuously from 24 hours to three days. To monitor the ECG, a Holter is used - a small portable recorder that records the round-the-clock work of the heart and records data on its work over the course of a day on a computer. These records are subsequently deciphered by a cardiologist.
Holter monitoring was named after researcher Norman J. Holter, who first put this device into practice in 1961.
When installing a Holter monitor, electrodes are attached to the patient's chest. The electrodes, in turn, are connected to a recording device. Of course, the patient experiences certain inconvenience while wearing the device, however, the study itself is very informative and accurate, which allows the cardiologist to determine an accurate diagnosis.
The data processing program provides analysis and determination of all types of heart disorders, in particular attacks of angina pectoris and arrhythmia, which can significantly improve the effectiveness of treatment of cardiovascular diseases.
Who is Holter monitoring indicated for?
With the help of a Holter, an ECG is prescribed primarily to determine heart rhythm disturbances - episodes of atrial fibrillation, extrasystoles, etc., which are quite difficult to detect during a short study - a regular electrocardiogram.
It happens that some atypical contractions for a healthy heart muscle appear only during periods of active physical activity, severe emotional shock, or in other situations. In these cases, such disturbances cannot be detected using a conventional electrocardiogram, whereas with Holter monitoring the patient can lead his usual lifestyle: engage in a certain sport, work, take any body position, etc.
Also, using a Holter study, you can determine various disorders of the blood supply to the heart muscle, in particular changes in the ST segment during sports or physical activity.
Can a Holter study negatively affect a patient's health?
Holter ECG does not pose any harm to health. There is also no risk of electric shock.
To avoid damage to the device, it is recommended not to take a bath or swim while wearing it to prevent water from getting inside. It is also not recommended to go through a metal detector while wearing a halter.
How is a Holter monitor installed?
Before the device is attached to the patient's body, he is advised to take a shower, since he will not be able to take a bath or remove the monitor for the next day or more.
The doctor attaches the electrodes to the patient’s chest and adjusts their position. Subsequently, the doctor connects the electrodes to the wiring of the recording device, which is attached to the patient’s body using special belts.
The doctor instructs the patient and teaches him to keep a diary. This is necessary for correct decryption of data received from the device. The patient records periods of sleep, wakefulness, physical activity, rest and all symptoms (chest pain, tachycardia, arrhythmia, etc.) with an exact indication of time.
After installing the device and receiving a list of instructions, the patient can return to his usual rhythm of life and daily routine.
Holter monitoring is an absolutely painless procedure. The patient experiences slight inconvenience only when wearing the device, when the wires and box of the device are hidden under clothing. During sleep, it is not recommended for the patient to turn over on his stomach, as the electrodes may become dislodged, which will disrupt data recording.
Holter study results
The holter is removed directly by a cardiologist or nurse. The patient provides the physician with a diary of activity and symptoms, which the physician examines along with device data.
Depending on the situation, the doctor makes a final diagnosis or sends the patient for additional examination. If the results of a Holter study within a day do not allow the doctor to form a definite picture, he can prescribe the patient to temporarily wear a heart rate recording device, which the patient himself will activate during the onset of alarming symptoms.
Why is ABPM necessary?
Blood pressure is an extremely unstable indicator. It can change during the day, depend on the emotional state, and differ during sleep and wakefulness.
It is worth mentioning the term "EBH", the white coat effect, the essence of which is that some patients experience undue anxiety simply because they are in the doctor's office.
Their blood pressure rises, which does not correspond to the true blood pressure level. A lot of negative factors can influence measurement deviations: a cold stethoscope, crossed legs, excitement. To prescribe the “correct” doses of antihypertensive drugs, it is extremely important to know the exact blood pressure standards obtained in the patient’s usual environment outside the doctor’s office.
An objective picture is provided by 24-hour blood pressure monitoring (ABPM) using a fully automated device mounted on the patient’s arm. The device records blood pressure values for 1-2 days under normal human conditions.
By analyzing the data obtained, the doctor confirms or denies the presence of hypertension. ABPM has a number of advantages over traditional studies.
The following disadvantages inherent in clinical measurements are excluded:
- the influence of an alarming reaction, which entails overdiagnosis of blood pressure and incorrect medical therapy for patients with EHD;
- rounding the measurement result, usually to tens;
- subjective assessment, when the researcher (doctor) is pre-set on a certain result, which he believes the patient “should have”;
- inability to take into account blood pressure fluctuations within 24 hours.
Daily monitoring is also useful for patients with already diagnosed arterial hypertension, when the study is combined with taking medications
Indications for use
The ABPM technique is indicated for:
- ineffectiveness of antihypertensive treatment;
- high blood pressure numbers in patients without signs of target organ damage (kidneys, myocardium, fundus, brain) and without identified risk factors for arterial hypertension (AH);
- normal blood pressure in patients with established risk factors for hypertension or existing target organ damage;
- high variability of blood pressure during self-measurement or during repeated visits to the doctor;
- frequent episodes of hypotension (low blood pressure) in older patients with type 1 diabetes;
- suspected preeclampsia.
ABPM is used in clinical practice not only in patients with hypertension, but also in patients with cardiac arrhythmias.
Preparatory activities
The first step is to make an appointment with a cardiologist. At the Family Doctor Children's Center for ABPM, you can undergo an examination without a doctor's prescription, but it is better to stock up on a referral, since a specialist must evaluate the results of the examination.
ABPM requires a free machine, so pre-registration is required.
In our center you are accepted without a queue and by appointment, but in public medical institutions you will have to wait several weeks. No special preparation is needed. The device will be installed by a doctor. He will select the “correct” cuff depending on the circumference of the patient’s shoulder.
A cuff that is too short or, conversely, long will distort the readings. The bag with the monitor (reading mechanism) is attached to the patient’s belt. The cuff is placed on the non-working arm: for right-handers - on the left, for left-handers - on the right.
The doctor will check the device for accuracy by alternately measuring blood pressure on one arm with a monitor and on the other with a regular tonometer. If the numbers match, the patient is sent home.
From this moment on, the device will periodically measure your pressure and “remember” the data. ABPM allows you to obtain fairly accurate daily blood pressure dynamics, provided that the patient adheres to the doctor’s recommendations.
The result will be distorted if the patient does not inform the doctor about the medications currently taken.
Who is contraindicated for 24-hour blood pressure monitoring?
ABPM is a non-invasive technique that does not require serious intervention in the body. However, there are a number of contraindications for it.
Diagnosis is not possible if:
- upper limb injury;
- skin diseases localized in the arms and shoulders;
- rigidity of the vascular system, since the accuracy of the test is impaired;
- pregnancy;
- heart disease and other serious pathologies that interfere with diagnostics;
- high blood pressure levels;
- blood clotting disorders.
In these cases, the diagnosis of ABPM will have to be abandoned, turning to traditional blood pressure measurement.
How is it going?
Diagnostics are carried out for a day or two. The first 2 hours are not taken into account as this is the adaptation time. Your doctor will ask you to keep a diary to record your hours of exercise and periods of rest, times you sleep and wake up, medications you take, heart pain, and other symptoms of discomfort if they occur.
Blood pressure registration occurs once every half hour during the daytime and every hour at night, at least. At the appointed time, the patient comes to the clinic and the device is removed from him. The doctor processes the device readings. The results obtained are interpreted by a cardiologist, comparing them with entries in the diary.
During the examination, the patient should follow simple recommendations:
- monitor the position of the cuff. If it has slipped, correct it;
- at the moment of start, the device emits a sound signal and begins to pump air into the cuff. Try to relax your hand at this time. If possible, do not move, so the readings will be more accurate. At the end of the measurement, a repeat beep will sound;
- do not pinch the tubes connecting the monitor to the cuff;
- stay away from electromagnetic devices;
- Avoid stressful situations. Anxious reactions greatly distort the readings of the device;
- temporarily refrain from swimming;
- don't drink alcohol;
- Protect the device from moisture. If there is an urgent need to remove the cuff, carefully disconnect the tubes from the monitor. Otherwise, when air is pumped, they may burst;
- if you notice that the device has stopped working, inform your doctor;
- stop taking antihypertensive medications (with the consent of your doctor);
- don't forget to keep a diary.
The ABPM technique does not prevent the patient from living his normal life, although it does introduce minor discomfort.
The accuracy of the readings largely depends on the patient's behavior during diagnosis. Listen carefully to the doctor’s instructions before conducting the test and try to follow all recommendations.
Decoding the results
During the study, it was possible to obtain 14 reliable measurements during the daytime and at least 7 during the night. Based on them, the doctor calculates the average blood pressure and pulse rate.
Since the interpretation of average values today does not pose a problem and is carried out on the basis of generally accepted standards, the most important are the “additional” ABPM readings:
- circadian rhythm (CR). ABPM is the only non-invasive study that provides a complete picture of this characteristic. The main indicator of SR is the percentage decrease in blood pressure at night. Violation of this value signals dysfunction of the cardiovascular system (CVS) and damage to target organs by hypertension. A practical problem in using the indicator is its low reproducibility, therefore, to confirm the reliability of identified SR failures, repeated monitoring is required, which is not always convenient for the subject. However, this characteristic must be taken into account in the conclusion based on ABPM results, especially if the procedure is performed for diagnostic purposes;
- ambulatory pulse blood pressure. This indicator is directly related to myocardial and vascular problems. ABPM assesses this characteristic more accurately than clinical studies. The “critical” value of ambulatory pulse pressure is 53 mmHg. Higher values indicate a risk of CV complications;
- blood pressure variability. Elevated values of this indicator may indicate incorrect antihypertensive therapy and the need to change the treatment regimen;
- morning dynamics of blood pressure. It is known that at this time the greatest number of heart attacks, malignant arrhythmias and strokes occur, which can cause sudden death of the patient. The morning increase in blood pressure in hypertensive patients is consistently higher than in healthy people, which is fraught with cardiovascular complications;
- assessment of hypotension episodes in the daily blood pressure profile. For an objective quantitative assessment, it is sufficient to take into account only the minimum blood pressure values;
- smoothing index (SI). Since ABPM provides a large amount of information, it can be used to more accurately assess the effectiveness of antihypertensive drugs. The indicator is calculated based on the hourly effects of the drug: the ratio of the average effect to the deviation from it. An IP of at least 1.2-1.5 is considered optimal.
The listed additional indicators of ABPM are very important. However, their practical use is still limited. The situation should change with the introduction of new generation drugs for hypertension into clinical practice and the widespread use of chronotherapy methods.
Pressure measurement methods
There are 2 types of manipulations for measuring blood pressure: direct and indirect. The direct method is highly accurate, but physically traumatic. A pressure gauge needle is inserted into the wall of the heart or artery. The tube of the device is filled with an anti-clotting agent. The scribe records blood pressure fluctuations in the form of a curve. The technique is used by cardiac surgeons, sometimes in laboratory conditions.
Indirect pressure measurement is a non-invasive method. The measurement is carried out on the peripheral vessels of the elbow or wrist using a tonometer. There may be errors, but the device can be used in any conditions.
Indirect diagnostics of pressure according to the type of technology used (mechanical, electronic) is divided into auscultatory and oscillometric options.
Auscultatory method
Also known as the Korotkoff method. Named after its inventor, surgeon N.S. Korotkova. Mechanical tonometers are used. The cuff is secured to the shoulder and inflated with air through a pear-shaped balloon. The upper and lower limits of pressure are determined by ear using a phonendoscope.
When the cuff is inflated, the blood flow in the artery is blocked, the external pressure exceeds the systolic pressure, and the characteristic sound pulsation stops. The gradual release of air restores blood movement, and tones begin to be heard again. The first beat corresponds to systal (upper) pressure, the last – diastolic (lower).
The Korotkov method is recognized as standard. It has its positive and negative sides. Even an accidental hand movement will not affect the result. However, there is a risk of incorrectly applying the cuff and stethoscope. The objective determination of pressure indicators can be interfered with by noise in the room. The device consists of many parts; during its use, a considerable number of manipulations are expected, so you need to learn how to measure pressure correctly.
Oscillometric method
Electronic tonometers with automatic or semi-automatic control are used. The cuff is attached above the elbow or on the wrist. In a fully automatic system, air is drawn in and released independently. In a semi-automatic machine, you must use a bulb. The indicators are displayed on the display without outside help based on the recorded pulsation.
The advantages of this method include the rapid preparation of the electronic device for operation. In addition, working with it does not require special skills, there is no error in human attention, and the noise in the room is not important.
In order for the indicators to be determined correctly, the hand must be motionless while measuring pressure. It is also forbidden to talk during the procedure.
Recommendations for intravascular measurement technology
It doesn’t matter at all whether your blood pressure is measured with a mechanical or automatic tonometer, or what the device for measuring a person’s blood pressure is called: shoulder, finger or wrist. It will be necessary to measure intravascular tension correctly, otherwise even the best devices will show an erroneous result.
- The test is carried out on an empty bladder, because the desire to visit the bathroom provokes intravascular tension.
- Whatever device you use, a sitting position will be required. You need to lean your elbows on the back of the chair and not cross your legs, but place them firmly on the floor.
- Devices for measuring a person’s blood pressure, namely cuffs, are put on the bare arm so that clothing does not create additional compression.
To protect yourself from the progression of intravascular diseases, you should consult with a specialist and find out how blood pressure is measured in your case.
This reduces the risk of complications such as heart attack, stroke and hypertensive crisis. The patient should regularly monitor his own intravascular condition to ensure a competent approach to therapeutic therapy and the return of blood vessels to normal.
How to measure pressure correctly
The most accurate result of this diagnosis can be obtained by following certain rules. Distorted indicators will not provide the necessary information content and may lead the patient and doctor to a false conclusion.
Preparation for the procedure
It is recommended to measure blood pressure an hour or more after fitness or smoking. Coffee, tea, energy drinks, a hot shower or bath require you to wait 1.5-2 hours. You should also wait 15-20 minutes. after eating.
It is advisable to empty the bladder and intestines before measuring pressure.
Before starting the diagnosis, you need to sit or lie down for 2 to 10 minutes. The posture during the measurement process should be relaxed, sitting, legs not crossed, not tense. The cuff should be placed correctly on the arm at the same level as the heart. The patient must remain silent.
Before measuring pressure, it is recommended to ventilate the room and ensure a comfortable air temperature.
Mechanical measurement algorithm
- Prepare the device. Remove the tonometer from the packaging and place the meter on a flat surface, ensuring a good view of the dial. Straighten all the tubes.
- Put on the cuff. Wrap the material around your bare forearm (2-3 cm above the elbow). Fasten tightly, but not too tight.
- Install a phonendoscope. Place the membrane under the cuff just above the elbow (on the inside of the arm). Insert headphones into your ears.
- Inflate the cuff. Take the bulb in your palm and tighten the valve tightly in a clockwise direction until it stops. Squeeze the bulb with quick movements until the cuff is filled with air and the monometer needle reaches 180 mm Hg. At this stage, a slight numbness of the arm may be felt due to blockage of blood flow in the artery.
- Start the measurement itself. Slowly open the bulb valve counterclockwise, gradually releasing air. In this case, it is necessary to monitor the dial needle and the tone in the ears. The first beat heard will occur at the systolic pressure mark, the last one at the diastolic pressure mark. Remember these indicators.
- Finish the procedure. As soon as the beats in the headphones have completely stopped, you can deflate the remaining air, remove the cuff and stethoscope, and put away the device.
If you were unable to listen to the readings, you can inflate the cuff again during the measurement process. You cannot repeat the manipulation more than once, because this distorts the data.
Electronic measurement algorithm
- Preparing the device. Place the tonometer body on a flat surface and straighten all the tubes well.
- Prepare your hand. Take off your watches, bracelets, roll up your sleeves.
- Put on the cuff. Place the fabric on the forearm above the elbow 2 cm.
- Patient preparation. Take a relaxed sitting position with straight legs. Keep your hand calm, it is better to rest it on the table with your palm up. Shut up and breathe evenly for about 30 seconds.
- Measurement. Press the start button according to the instructions. The cuff will begin to inflate and running numbers will appear on the screen. Without changing position, wait until the air is completely deflated and the readings on the monitor stabilize.
- Remove the device. Remove the cuff and stop the device.
When measuring with a wrist tonometer, you should also remove jewelry from your hand and expose your skin. The cuff is put on with the display up 1 cm above the hand. The hand with the device is placed palm down on the opposite shoulder. This is followed by startup, inflation of the cuff, appearance of indicators and deflation.
For maximum accuracy, the diagnosis can be repeated after 15 minutes.
How to choose a tonometer for home use
Today, there are several options for blood pressure meters on the medical equipment market, each of which has its own advantages and disadvantages. This:
- A mechanical meter characterized by high measurement accuracy and accessibility. Air is pumped into the cuff by squeezing the rubber bulb. Among the disadvantages are: the sensitivity of the device to noise and vibration, the need for the exact location of the phonendoscope. This is the optimal solution for doctors and is not recommended for home use.
- The semi-automatic also works by pumping air with a pear. But all data is displayed on the monitor, which simplifies the assessment of a person’s condition. The device demonstrates not only the values of arterial systolic and diastolic pressure, but also the pulse rate.
- The automatic device is equipped with a compressor that pumps air without human intervention. The best solution for home use, especially when a person measures his own blood pressure.
Before purchasing, you need to pay attention to the following characteristics: availability of service or warranty service, method of powering the device, quality of the bulb (if included), type of cuff and additional options.
Advice! It is worth choosing a device from a reputable manufacturer that can guarantee the quality of its products. Among the best companies holding leading positions in the medical equipment market: Omron, A&D, Little Doctor, B.Well, Microlife, Beurer.
Measurement errors
An important condition is not to touch the phonendoscope membrane and cuff with your hands during the measurement process. Pulse from holding fingers will distort the readings. The tissue between the skin and the cuff interferes with the membrane's receptivity.
You cannot deviate from the level of the heart in the position of the cuff; the numbers will turn out to be too high or too low. The same result will be achieved if the Velcro is fastened too loosely or too tightly, a tired state, a hunched back, or the patient moving and talking.
When using a mechanical tonometer, you should not choose to round the indicators to 0 and 5. Only the actual data shown is taken as truth.
Algorithm for the procedure
The accuracy of the tonometer's readings depends on how high-quality the device is, as well as external factors. For example, it will not be possible to correctly measure blood pressure immediately after a run.
Recommendations for working with electric and other types of tonometers are as follows:
- The recommended time for diagnosis of hypertension is from 7 to 9, and also from 19 to 21 hours. It is during these periods that pressure reaches its peak, and timely identification of deviations makes it possible to respond to the situation in a timely manner.
- Many people do not know how many times they can take their blood pressure. For both hypertension and hypotension, you can limit yourself to two diagnostic procedures per day - in the morning and in the evening, if there are no separate medical recommendations.
- It is important to measure blood pressure in an atmosphere of maximum rest. You should turn down the TV volume and do not talk or move during the procedure.
- Half an hour to an hour before measuring with a special apparatus to accurately determine the values, you should not eat, take medications that can affect the result, drink coffee or strong tea, drink alcohol, engage in physical activity, or smoke.
- The best position for measuring blood pressure is sitting on a chair with a comfortable backrest. You can't cross your legs. The arm on which the cuff is worn should be at heart level. To do this, it should be placed on the table. Lying or standing, blood pressure is measured only in exceptional cases.
- Initially, blood pressure is measured on both arms at intervals of several minutes. On which arm the blood pressure was higher, the cuff should be put on that arm in the future.
- In case of arrhythmia, it is important to take 3 consecutive measurements with a device for home use. If the tonometer is not equipped with an additional function (MAM technology or arrhythmia sensor), you should measure blood pressure, relax the cuff, repeat the manipulation after 2 minutes and after another 2-3 minutes. The average value will be the true pressure reading.
- Data on systolic, diastolic pressure, heart rate, date and time of measurement must be recorded in a journal or device memory for subsequent analysis of the course of hypertension (hypotension) and informing the attending physician about your condition.
Important! It is impossible to independently diagnose hypertension without additional examination. The doctor makes an analysis of the patient’s condition based on blood tests, daily blood pressure monitoring, ECG, and only after that decides on a treatment regimen.
No ads 2
Interpretation of indicators
The blood pressure of an adult is distributed by doctors as follows:
- optimal. 120 by 80 units and slightly lower;
- normally acceptable. Up to 130 to 85;
- moderately elevated. Up to 139 to 89.
Numbers above the moderately elevated limit indicate hypertension.
Children's blood pressure may have different standards depending on age; they are determined by the doctor.
Pressure monitoring
Monitoring refers to repeated measurements over a certain period. This practice is used to select the right medications, control pregnancy, and certain diseases. The doctor may prescribe diagnostics at regular intervals, at set hours, require you to keep a blood pressure diary or wear a smart blood pressure monitor with a memory function. The latter option is more expensive, but is convenient for recording more than 100 indicators with the date and time of measurement without the participation of the patient.
Determining blood pressure using devices is used everywhere in everyday life and medicine. Different tonometers have their own errors and advantages. It is better to buy a specific type after consulting a supervising doctor, taking into account the situation.
Which glucometer is the best?
For a doctor, accuracy is important in a glucometer; for a patient, convenience and ease of use are important.
Accuracy. The accuracy of the instrument is important. International accuracy standards have been adopted for a glucometer for home use. According to ISO 15197, the error compared to the laboratory should be within 20%. This means that by taking 2 different glucometers and measuring blood with them simultaneously, you can get results that differ by up to 40%. There is no need to be scared, it is better to choose one device and use it constantly, this will give a real picture of your sugar level over time and will help you and your doctor.
Convenience. The device should be as gentle and comfortable as possible. A device with capillary blood sampling is considered more convenient. After the puncture, you dip the edge of the test strip into a drop of blood and it itself absorbs the required amount. There are devices where you need to drop a drop of blood into a special field on the test strip; this is more difficult to do, especially for an elderly person.
The display should be bright, with large font so that the readings are easy to read. It is advisable to choose a device where you do not need to enter the coding for calibration manually. This reduces the likelihood of measurement errors.
Younger users can choose glucometers that transmit readings via Bluetooth and have various software and applications. If the user is elderly and writes down data in a notebook the old-fashioned way, these functions can also be useful, but for control by relatives and the attending physician.
There are glucometers that transmit readings via Bluetooth and have various software and applications.
One of the most painful topics is the price of test strips. This is what you need to focus on when choosing a glucometer, among other characteristics. The average price category provides good quality measurements, the main thing is to take them regularly.
Also, when traveling abroad, you need to have a supply of test strips, since the models of glucometers may differ in different countries and strips purchased abroad may not fit your device.
Therefore, it is impossible to say unequivocally which device is better. It is necessary to know who will use it and under what conditions. Based on this price-quality ratio, make a choice.