Causes of vasoconstriction
Vasoconstriction, also called stenosis, is familiar to a large number of people, especially those who spend a long time at the computer for work. But constant overstrain of the anatomical structures of the neck in a sitting position is far from the main cause of the development of pathology. There can be a lot of reasons, and they are divided, first of all, into:
- Congenital.
- Purchased.
We need to look at the reasons in more detail.
Congenital pathology
In the first case, narrowing of the vessels of the cervical spine is preceded by congenital hypoplasia of the veins and arteries of the cervical spine, as well as stenosis of the carotid arteries and disorders in the development of the spine in this area, vertebral arthrosis. Congenital causes may occur due to:
- distribution of toxins throughout the pregnant woman’s body;
- injuries to a pregnant woman;
- infection of the expectant mother's body.
In general, any stressful situation for a pregnant woman’s body can result in abnormal development of the fetus.
Purchased
In the case of acquired causes of the development of pathology, it is worth noting that the development of the disease is provoked by: atherosclerosis, a decrease or increase in blood pressure, an increase in blood sugar levels, injuries and hernias in the cervical spine, as well as various tumors. In addition, the disease can appear with intense mental or physical work, neglect of sports and even minimal physical activity, bad habits and stress.
Congenital anomalies of vascular development on ultrasound
Hypoplasia, that is, a small diameter of the vertebral arteries, is a fairly common finding in the practice of ultrasound diagnosticians. The most typical form of its manifestation is hypoplasia of one of the vertebral arteries with a decrease in blood flow in its basin. Often there is a high entrance of one or two arteries into the spinal canal, while part of the path of the vertebral artery is not protected by the bone canal and can be compressed when turning the neck. Less common are the absence of any of the vertebral arteries and hypoplasia of the carotid arteries. An ultrasound of the neck vessels will clearly show the presence of hypoplasia, but we will not always be able to say whether this is a congenital anomaly or an acquired narrowing of the vessel due to osteochondrosis. This pathology requires conservative vascular treatment in order to increase the general blood flow of the body so that compensation occurs at the expense of other arteries. The effectiveness of the treatment is usually monitored using a series of control ultrasounds of the neck vessels.
Symptoms
Symptoms of vasoconstriction in the cervical spine do not appear for a very long time, and a person with this disease does not notice any deterioration in well-being. However, later in the development of the disease it begins to manifest itself:
- constant dizziness;
- lack of strength even with constant rest;
- sudden loss of consciousness for no reason;
- flickering before the eyes;
- noise or ringing in the ears;
- pressing or aching pain in the head, particularly in the back of the head, may spread to the neck.
In general, two groups of symptoms can be distinguished. The first group includes manifestations that reduce a person’s level of performance, but do not lead to a desire to visit a doctor. The second group includes obvious pain manifestations and symptoms that indicate significant blockage of blood vessels and the need for urgent hospitalization of the person.
Will an ultrasound of the neck vessels show a tumor?
With an ultrasound of the vessels of the neck, doctors sometimes detect compression of the vessels by tumors.
First of all, it may be metastases of the lymph nodes of the neck. The peculiarity of metastatic tissue is that it is rigid, so it can compress the vessel or grow into its wall and form a tumor thrombus. All this is well visualized by a comprehensive ultrasound examination of the vessels of the neck and ultrasound of the soft tissues of the neck. Initial appointment with a NEUROLOGIST
ONLY 1800 rubles!
(more about prices below)
Diagnostic methods
Neurologist
It is not enough to interview and examine the patient to identify narrowing of the blood vessels of the spine; in any case, additional examinations will be prescribed. These include:
- Duplex scanning
- despite the fact that this is a rather dangerous diagnostic method in this situation, it is informative and accessible, it allows you to determine the degree of narrowing and its nature. - Angiography - the process uses a contrast agent to examine the vessels.
- and MRI
- allow you to obtain layer-by-layer 3D images, with which you can make a diagnosis.
All this will allow the doctor to determine not only the patient’s health status, but also the reasons that led to the occurrence of stenosis.
How does ultrasound show tortuosity and deformation of blood vessels?
Ultrasound of the vessels of the neck and head quite accurately shows changes in the shape and location of the arteries and the effect of these changes on blood flow. Most often in the practice of doctors, tortuosity of blood vessels occurs. Vascular tortuosity is an adaptation of the body to increased or unstable pressure and to various changes in the spine, which can sag in its height. This pathology is primarily associated with age-related characteristics or high blood pressure. In most hypertensive patients, ultrasound of the neck vessels will show either T-shaped or S-shaped tortuosity. Not all vascular tortuosity poses a threat to the health of patients. It is important for the neurologist to exclude loops and kinks in the arteries. The bending of the arteries at an acute angle is a kind of stenosis, which does not allow blood to pass through and requires surgical intervention. The results of the ultrasound scan will answer the question of whether this tortuosity is obstructing blood flow, since this determines the form and urgency of treatment. If the tortuosity severely deforms the vessel, when it bends at an acute angle or twists in a loop, the neurologist should refer the patient for a consultation with a vascular surgeon to decide on the need for surgical intervention.
Treatment
The method of treating narrowing of blood vessels in the cervical spine is prescribed depending on the degree of progression of the disease. The earlier the condition is detected, the easier it is to get rid of it; in the later stages, only surgery is indicated.
Drug treatment
It is prescribed if the manifestations of stenosis are not yet very pronounced. In such a situation, the patient will have to take a large number of medications, among which will be:
- antioxidants;
- vasodilators;
- statins;
- fibrates;
- antidepressants.
Treatment with medications for vasoconstriction of the cervical spine involves quickly relieving pain and stopping the progression of the disease.
Operation
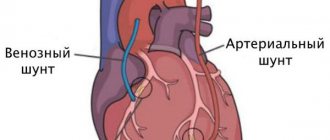
If the doctor determines vascular spasm and their occlusion by more than 70%, only surgical intervention will be indicated. There are several options to solve the problem:
- Carotid endarterectomy - the vessels are “cleaned” of plaques by scraping them out.
- Angioplasty - the lumen of the vessel is increased thanks to a special catheter.
- Stenting - a special frame is installed, which leads to straightening of the narrowed section of the vessel.
The possibility of performing each type of operation is determined by the doctor individually, since each type has its own indications and contraindications. Everything will depend on the diagnostic results.
Cerebral circulation disorders in cervical osteochondrosis
Osteochondrosis is a degenerative-dystrophic disease of cartilage tissue that develops as a result of impaired metabolism of glycosaminoglycans. It can begin in almost any articular joint of the body, but most often it affects the intervertebral discs of the most mobile segments of the spinal column - the cervical and lumbar.
Since the intervertebral joints do not contain blood vessels, their nutrition and water supply occurs in a diffuse manner (by exchange with nearby soft tissues). With age, metabolic processes in the body slow down significantly or are disrupted, which leads to gradual dehydration and destruction of cartilage fibers, and, consequently, subsidence and thinning of the intervertebral discs.
Deformed joints are no longer able to fully perform their shock-absorbing functions, and with certain physical activities, pinching of nerve roots and blood vessels, pain, limited mobility and other complications occur. For the cervical spine these are headaches, dizziness, cerebrovascular accidents, hearing and vision disorders, etc.
Pathogenesis of the disease
Chronic pain syndrome, inflammation, spasms and discomfort when moving the head cause a response from the body, as a result of which growths of bone marginal plates (osteophytes) are formed. With sudden physical exertion or awkward movements, intervertebral hernias or protrusions may occur, when the dense shell of the disc cracks, releasing a gelatinous substance (nucleus pulposus). Quite often, it is osteophytes or hernial protrusions that compress the spinal blood vessels or nerve endings.
The cervical segment of the spine is designed in such a way that almost all the vital highways of the body that feed the brain lie in it, but it is supported and protected only by a very thin muscular corset.
As a rule, vascular pathologies are based on two main factors: compression of the vertebral or basilar arteries, as well as damage to the vasomotor (vasomotor) center located in the medulla oblongata. It is damage to the latter that causes dysfunction of the innervation of all smooth muscles of blood vessels (including the spinal cord and brain), which is fraught with sudden changes in blood pressure, hypoxia, ischemia, stroke, etc.
A decrease in the tone of the blood vessels of the brain, as well as the whole body, causes thickening of their walls or stenosis of the lumen of the canal, which can provoke disturbances in blood microcirculation, and, consequently, a slowdown in metabolic processes. In some cases, restoration or compensation of blood circulation occurs due to developed networks of collaterals, but they are not always durable.
Stages of disease development
The development of circulatory disorders in the system of vertebrobasilar arteries in osteochondrosis of the cervical spine can be conditionally divided into the following stages:
- Initial or stage of development of dyscirculatory encephalopathy (slowly progressive and/or diffuse damage to blood vessels, small arteries and arterioles of the brain). The patient is worried about dizziness, headaches, decreased attention and memory, difficulty maintaining balance, sleep disorders, fatigue, dysfunction of the organs of vision and hearing. There is a loss of cognitive, spastic, vestibular and autonomic functions.
- Subcompensation or the stage of pronounced neurological disorders, when the symptoms of the disease gradually increase and the patient’s well-being worsens. This is expressed in disorders of thinking and the ability to control subtle sequential movements, slower speech and chewing, deepening of the voice, constant changes in blood pressure, apathy, emotionally depressed state, etc.
- Late stage (decompensation) or stage of development of irreversible disorders in the central nervous system. At this stage, the patient practically becomes disabled, as he loses the ability to care for himself. He develops vascular dementia (dementia), affective disorders, parkinsonism, hypokinesia, involuntary laughter or crying, and quite often there is no ability to control urination and defecation.
Diagnosis and treatment of circulatory disorders in cervical osteochondrosis
A preliminary diagnosis is made during the initial examination of the patient by a neurologist and after collecting the clinical picture. The level of damage to the intervertebral discs is determined after an X-ray of the spinal column. Compression or damage to blood vessels, vascular beds, and nerve endings can be seen on an MRI or CT scan.
Pathologies of the spinal cord or brain are diagnosed using myelography with the introduction of a contrast agent. Dopplerography and ultrasound examination of cerebral vessels makes it possible to determine the patency of the channels and the speed of passage of blood fluid through them.
Treatment of cerebral circulatory disorders with cervical osteochondrosis depends on the location of the pathology, the severity of the lesion and the causes of the disease. First of all, conservative therapy is aimed at improving the patient’s condition (restoring and improving metabolic processes in the body and activating the regeneration processes of damaged cartilage tissue). For these purposes, the following are used: exercise therapy, massage sessions and physiotherapeutic procedures, adequate physical activity, and various water procedures.
Surgical methods of treatment are used quite rarely and only in cases where the patient’s condition sharply worsens or there is a threat to the normal functioning of internal organs.
Special drug therapy, in addition to drugs that relieve pain, muscle spasms, inflammation and swelling of soft tissues in the treatment of classic osteochondrosis, consists of:
- vasoactive drugs that activate cerebral circulation and dilate blood vessels;
- neuroleptics and antidepressants that have a sedative, calming effect, reducing the degree of cognitive (dizziness, vomiting, sweating, etc.) manifestations;
- nootropic agents that improve metabolic processes in the brain, memory, perception, thinking, speech abilities;
- diuretics and antioxidants, which help reduce swelling and activate the body's regeneration processes;
- B vitamins, calcium supplements or other vitamin complexes that improve the condition of the central nervous system and the patient’s entire body.
At home, the patient is advised to reconsider his lifestyle, give up bad habits, devote more time to active recreation and activities, and try to control his weight.
It is advisable to do morning exercises every day, water procedures, special physical exercises, attend sports clubs or take daily long walks at a fast pace.
Follow a daily routine, alternating appropriate periods of stress and relaxation, eat properly and rationally. Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
Nonspecific Tokayasu aortoarteritis on ultrasound of neck vessels
Tokayasu nonspecific aortoarteritis manifests itself at a young age and leads to lifelong hormone therapy. This is a systemic inflammation of blood vessels, leading to thrombosis. Diagnosis of this disease is difficult because it can develop in any part of the human vascular system. Here, it is important for doctors to use ultrasound to identify inflammatory changes in the arteries as early as possible. To do this, a comprehensive examination is carried out - ultrasound of the vessels of the whole body, which will include:
- Ultrasound of the vessels of the neck and head;
- Ultrasound of vessels of the lower and upper extremities;
- Ultrasound of the abdominal aorta;
- Ultrasound of pelvic vessels;
- Ultrasound of renal vessels.
Author: Shogenov Ramish Kurbanovich
Neurologist with 10 years of experience