Causes of Gestational Diabetes
The exact mechanism of the disease is still not completely clear.
Doctors are inclined to believe that the hormones responsible for the proper development of the fetus block the production of insulin, which leads to disruption of carbohydrate metabolism. During pregnancy, more glucose is required for both the woman and the baby. The body compensates for this need by suppressing insulin production. There are other possible causes of gestational diabetes, such as autoimmune diseases that destroy the pancreas. In principle, any pancreatic pathology can increase the risk of diabetes during pregnancy.
Symptoms
Photo: ruslangaliullin / freepik.com
The clinical picture of gestational diabetes mellitus is quite poor; a woman may not have any complaints at all. It is worth paying attention to the following signs:
- Unmotivated weakness
- Thirst, dry mouth,
- Frequent urination
- Blurred vision.
The dangers of diabetes during pregnancy
This pathological condition threatens the health of both mother and child.
Even before birth, the fetus begins to actively produce insulin to compensate for the increased glucose in the mother’s blood. Such children are prone to low blood sugar from birth, and they have a higher risk of obesity and type II diabetes in adulthood. Gestational diabetes increases the risk of high blood pressure, as well as preeclampsia, a severe form of preeclampsia. It manifests itself as headaches, nausea, vomiting, blurred vision, lethargy, drowsiness or insomnia. This is one of the most severe disorders during pregnancy, affecting the central nervous system.
Another alarming factor is that diabetes during pregnancy contributes to rapid weight gain in the baby during the prenatal period (macrosomia). This causes difficulties during childbirth and poses a threat to the mother. A child over 4 kg is considered large. These babies have a higher risk of birth injuries and are more likely to require a caesarean section. Due to the large size of the fetus, early delivery may be required. At the same time, the risk of premature birth is high.
Also, high sugar in pregnant women increases the risk of cardiovascular and nervous pathologies of the fetus, increases the risk of respiratory distress syndrome in the baby (a condition that makes breathing difficult) and generally increases the frequency of complications during pregnancy and childbirth.
What is its reason?
Diabetes mellitus in pregnant women develops due to the hormonal explosion associated with bearing a child. The hormonal cocktail entering the blood (cortisol, human chorionic gonadotropin, estrogens and progesterone) inhibits the action of insulin, which is required to ensure the flow of glucose from the blood into the cells. This happens because the body tries to save glucose for the growing fetus and provokes “insulin resistance,” when the mother’s cells stop responding to the usual amount of insulin. In response to increasing amounts of glucose in the blood, the pancreas is supposed to produce more insulin, but sometimes it fails. Gestational diabetes occurs.
Up to 39% of all pregnancies are complicated by GDM.
Risk factors for gestational diabetes
- Age under 18 and over 30 years old.
- Unbalanced diet with a lot of fast carbohydrates.
- Bad habits (smoking, alcohol abuse).
- Overweight and obesity. Excess weight obviously implies a violation of metabolic processes.
- Lack of physical activity.
- Previous gestational diabetes or prediabetes. The tendency to diseases of this series does not disappear over time.
- Polycystic ovary syndrome.
- A close relative has diabetes. The risk of gestational diabetes increases twofold or more if close relatives have any form of diabetes.
- Previous birth of a child over 4 kg or a large fetus during the current pregnancy.
- Race. Caucasians have the lowest risk of developing gestational diabetes, and black women are most likely to suffer from this problem.
Unfortunately, GDM can develop in a completely healthy woman without risk factors, so you need to visit a doctor and not skip recommended screenings.
Are there any contraindications to the test?
Yes, I have. Absolute and relative.
Absolute contraindications include:
- Allergy and/or glucose intolerance,
- Diabetes mellitus in the acute phase (then a test is not needed),
- Diseases of the gastrointestinal tract in which normal glucose absorption is disrupted (exacerbation of pancreatitis, gastric surgery).
Relative (temporary) contraindications:
- Early toxicosis (gestosis) of pregnant women,
- Exacerbation of chronic diseases
Important! It is very important to determine the presence of GDM in a timely manner. Screening is recommended for all pregnant women. The glucose tolerance test does not harm the liver and is not something to be afraid of.
When diagnosing GDM, additional tests are sometimes used, including:
- General urine analysis (glucosuria - detection of glucose in the urine, which normally should not be there, as well as ketone bodies - products of impaired glucose metabolism),
- Ultrasound of the fetus (presence of fetopathy - fetal development disorders).
Diagnosis of gestational diabetes
There is good news.
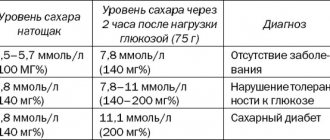
When registering, all pregnant women are required to take a blood test for glucose levels, so if you regularly undergo all prescribed examinations, you will detect the problem at the very early stage. The normal value is 3.3-5.1 mmol/l when testing blood from a vein on an empty stomach. Patients whose glucose levels exceed 5.1 mmol/l are at risk. In this case, the doctor will order a glucose loading test or glucose tolerance test to confirm or refute the diagnosis. It is carried out at 24-28 weeks of pregnancy. Such a study includes two stages: first, a woman takes a regular blood test for glucose on an empty stomach, after which she drinks a special solution containing 75 grams of glucose, and after two hours she takes the test again. If a disease is suspected, the same analysis is repeated again after a few hours.
The diagnosis of gestational diabetes is made if the fasting blood glucose level is less than 7 mmol/l, but above 5.1 mmol/l, and the venous blood glucose level two hours after consuming 75 g of glucose is above 8.5 mmol/l.
Gestational diabetes mellitus - symptoms and treatment
As soon as an endocrinologist or obstetrician-gynecologist has established a diagnosis of GDM, the patient needs to be told about the principles of a rational, balanced diet, the need to keep a food diary, self-monitoring of glycemia and control of ketonuria - ketone bodies in the urine.
Diet therapy
The first step to achieving and maintaining normal glucose levels in GDM is dietary therapy[3][25][26][27]. Its goal is to ensure stable normoglycemia, prevent increases or decreases in blood glucose levels and ketonemia.
A pregnant woman's diet should contain a sufficient amount of carbohydrates, excluding easily digestible ones (found in white bread, sweets, some fruits, etc.). The optimal amount of carbohydrates per day is 175 g. It should be divided into three main meals and 2-3 snacks.
Principles of diet therapy:
- emphasis on the consumption of complex carbohydrates (up to 55% of the recommended daily caloric intake) with low fat content (25-30% of the recommended daily caloric intake);
- the daily amount of fiber should be at least 28 g;
- the amount of fat should not exceed 35% of the daily calorie intake, while the consumption of saturated fats should be limited to 10%, and trans fats should be completely eliminated;
- to prevent the appearance of ketone bodies, the break between the last meal in the evening and the first the next day should be no more than 10 hours [3] [25].
Each meal should contain slowly digestible carbohydrates, protein, mono- and polyunsaturated fats, and dietary fiber. This increases insulin sensitivity, promotes less weight gain, and reduces the frequency of prescribed insulin therapy for GDM. Pregnant women with obesity and pathological weight gain are recommended to limit calorie intake, but not less than 1800 kcal/day to avoid ketosis.
During diet therapy, self-monitoring of glycemia is carried out: measuring blood glucose on an empty stomach, during the day and before main meals, at night (up to 5.1 mmol/l), an hour after meals (up to 7.0 mmol/l).
Dietary recommendations for GDM[2][3][25]:
- Foods that can be eaten in any quantity:
- vegetables - cucumbers and tomatoes, any cabbage, zucchini and zucchini, eggplant, celery, green beans, radishes and radishes;
- soy products;
- herbs - dill and parsley, green onions, sorrel, lettuce.
- Products that need to be completely excluded:
- sugar and honey, candies, milk chocolate and cocoa, jam, jam, jam, any pastries;
- dairy products containing sugar - yoghurts, glazed cheese curds, sweet curds, etc.;
- instant food products - quick-cooking porridges, purees, noodles;
- pumpkin, sweet corn, stewed carrots and beets;
- some fruits and berries - watermelon, melon, cherries, grapes, persimmons, bananas, figs, raisins, dried apricots, prunes;
- white bread, baked goods and flour not made from durum wheat;
- all carbonated drinks, store-bought and freshly squeezed fruit juices.
- Products that can be consumed, but only with restrictions:
- cheese - up to 100 g per day together with vegetables or separately from other food;
- cottage cheese - up to 200 g per day along with vegetables or separately from other foods;
- smoked, spicy, salty foods - up to 50 g per day once a week;
- salt - up to one teaspoon per day;
- red caviar;
- dark chocolate (75% cocoa) - up to 25 g per day;
- 3.5-6% milk - up to 100 ml at a time;
- fermented milk products (kefir, ayran, tan, yogurt) - up to one glass at a time;
- butter - up to 10-15 g per day;
- 10-15% sour cream - up to 100 g per day;
- some berries (aronia, lingonberries, blueberries, blueberries, blackberries, feijoa, currants, strawberries, strawberries, raspberries, gooseberries, cranberries, cherries) - up to 200 g separately from other food or with cottage cheese no more than 100 g, can be eaten for breakfast ;
- some fruits (grapefruit, lemon, lime, kiwi, orange, apples, apricots, peaches, plums, tangerines, pears, pomegranate, mango, papaya) - separately from other foods, without mixing several types of fruits and berries; do not eat before 12:00 and after 22:00;
- potatoes and slightly undercooked beets - up to 100 g per day;
- stewed vegetables - up to 200-250 g per meal;
- vegetable pancakes (cutlets) - up to 150 g per meal;
- raw carrots - up to 100 g per day;
- mushrooms - up to 200 g per day;
- dried apples, pears, plums, apricots - up to 50 g per day separately from other food;
- seeds, nuts - up to 50 g per day separately from other foods;
- bread made from wholemeal flour (it is better that it contains 60 g of carbohydrates per 100 g of product) - up to 150 g per day;
- all cereals - up to 200 g per day three times a week (buckwheat can be eaten daily);
- undercooked spaghetti and durum wheat pasta - up to 150-200 g per day daily.
Dairy products are best consumed as a snack between meals. You can make berry smoothies with kefir and milk.
Recommendations for fat consumption[2][3][25].
| Fatty acid | Acceptable daily intake from RSKP for fats | Food |
| Monounsaturated | > 90% | •⠀Avocado, sesame, olives •⠀Raw almonds, cashews, walnuts, pistachios, peanuts, pine nuts, macadamia, Brazil nuts •⠀Olive, safflower, peanut, canola, corn oil |
| Polyunsaturated | > 90% | •⠀Sunflower and pumpkin seeds •⠀Fish and seafood, fish oil •⠀Walnut oil, flaxseed, soybean, sesame |
| Saturated | •⠀Meat, ham, sausages, lard •⠀Cream, sour cream, milk, ice cream, cheese | |
| Trans fats | 0 | •⠀Margarine, spread •⠀Chips, fast food •⠀Semi-finished products •⠀Low fat cheeses •⠀Industrial sauces |
Physical activity
Exercise helps overcome insulin resistance and control fasting and postprandial hyperglycemia. They complement dietary recommendations to lower maternal glucose levels.
There is no ideal type of exercise for GDM, but most often they recommend walking in the fresh air after eating - you need to walk at a moderate pace for at least 30 minutes three times a week [6].
Vitamin therapy
As various studies show, vitamin D affects the production and dysfunction of insulin, and also increases sensitivity to this hormone.
Recent studies have shown that taking vitamin D during pregnancy reduces the risk of GDM[29]. To prevent this condition, pregnant women are recommended to receive native forms of vitamin D at a dose of 1200 IU/day[31]. If GDM does develop, then additional treatment with a high dose of vitamin D (50,000 IU every two weeks) can improve insulin resistance [30].
The relationship between GDM and B vitamins has also been established. According to the study, homocysteine concentrations in women with GDM are higher than in pregnant women without GDM[32]. This amino acid accumulates when the folan cycle, a complex cascade process, is disrupted. This cycle can be normalized with the help of B vitamins, including folic acid, B2, B6 and B12.
According to the clinical protocol of MARS (International Association of Reproductive Specialists), women need to take folates (vitamins B9) for three months before pregnancy and at least during the first trimester of pregnancy, optimally as part of folate-containing complexes at a dosage of 400-800 mcg/day[33 ].
Insulin therapy
Insulin therapy is indicated if it was not possible to normalize glycemic values during diet therapy for two weeks (more than 2 non-target values), as well as in the presence of signs of diabetic fetopathy according to ultrasound data [3] [25].
Any hypoglycemic drugs taken orally are contraindicated for pregnant women. In the Russian Federation, short- and medium-acting human insulin preparations and biosynthetic analogues of ultra-short and long-acting insulin are permitted[25].
The insulin therapy regimen is selected individually by the endocrinologist depending on the indicators of glycemic self-control:
- if glycemia increases an hour after a meal, therapy with ultra-short or short-acting insulin is prescribed;
- if fasting blood glucose increases, use long-acting insulin therapy;
- for newly diagnosed (manifest) diabetes mellitus - insulin therapy in a basal-bolus mode (imitation of insulin production by the body);
- in case of ultrasound signs of diabetic fetopathy, nutritional correction is carried out immediately; it is recommended to monitor glycemia two hours after meals to identify a possible shift in the peaks of hyperglycemia when consuming large amounts of fat and protein; the issue of preprandial insulin (on an empty stomach) is considered if hyperglycemia is confirmed.
During insulin therapy, self-monitoring of glycemia is carried out at least seven times a day:
- before meals;
- an hour after eating;
- at night;
- if necessary, titrate the dose of long-acting insulin at 03:00 and 06:00.
Treatment goals for glycemia remain the same: fasting glucose, during the day and before main meals, at night up to 5.1 mmol/l, one hour after meals up to 7.0 mmol/l, two hours after meals up to 6.7 mmol/l[3][24][25].
Insulin lispro (Humalog)[34] and insulin aspart (NovoRapid)[35], as studies show, do not cross the placenta and are approved for use during pregnancy. They are analogues of human insulin, ultra-short-acting, so they can be taken immediately before meals. They provide greater flexibility in meal timing compared to short-acting human insulin, which must be taken 20-30 minutes before meals.
NPH insulin (suspension of insulin and protamine) has an average duration of action (12-16 hours). It can be combined with short-acting insulins.
Long-acting biosynthetic insulin analogues are available and used to simulate basal levels (insulin glargine 100 IU/ml, insulin detemir). These long-acting insulin analogues do not have a peak effect and last about 24 hours. They are not inferior to NPH insulin in terms of glycated hemoglobin HbA1c [36][37][45].
Treatment of diabetes in pregnant women
The first step in treating GDM is a balanced diet and moderate exercise.
The main goal of the diet is to reduce sugar to normal values, so the expectant mother will have to give up sweets and fast carbohydrates. Pregnant women are recommended:
- Eat little, but often.
- Exclude foods with a high glycemic index (sugar, honey, potatoes, white bread, baked goods, bananas, grapes).
- Avoid fast food and fatty sweet pastries.
- Drink enough fluids if there are no contraindications from the kidneys.
- Diversify your diet with fresh vegetables, lean meats, and cereals.
Like all pregnant women, it is important for patients with GDM to receive the full range of vitamins and minerals that are necessary to maintain their own health and the proper development of the fetus.
Walking, swimming, water gymnastics, physical therapy for pregnant women - any light activity will be beneficial.
If diet and exercise do not help lower blood sugar levels, insulin therapy is prescribed.
Important: with high sugar, a woman should check her glucose level daily. Measurements are taken on an empty stomach and an hour after each meal using a home glucometer.
Why is GDM dangerous?
GDM can cause various pregnancy complications, which is dangerous for both mother and baby.
Danger of GDM for mother
The health risk to the expectant mother is associated with excess glucose in the blood and its deposition in tissues and organs. Like any type of diabetes, GDM can contribute to:
- Diabetic retinopathy – damage to blood vessels and retinal receptors with gradual deterioration of vision (Fig. 1).
- Diabetic nephropathy is damage to the glomerular and tubular apparatus of the kidneys, in which blood plasma is filtered to form urine. As a result, chronic renal failure develops.
- Arterial hypertension is high blood pressure that occurs due to damage to blood vessels, kidneys and changes in hormonal levels with the development of diabetes. All this increases the risk of miscarriage and abnormalities in the fetus.
Figure 1. Diabetic retinopathy. Source: WikiMedia
Risk to the child
An increased level of glucose in the blood of a pregnant woman can harm not only herself, but also the unborn child, contributing to:
- diabetic fetopathy (a disorder of carbohydrate metabolism in an unborn child, which can develop into neonatal, infant diabetes mellitus);
- the birth of a large fetus - macrosomia (increases the risk of cesarean section and injury to the child during childbirth);
- neonatal hypoglycemia (low blood sugar in the newborn and respiratory problems, which can lead to death);
- intrauterine fetal death (this is the worst consequence of GDM);
- polyhydramnios (dangerous due to premature birth, incorrect position of the fetus, loss of umbilical cord loops and their compression, placental abruption due to rupture of the membranes);
- an increase in the size of the liver and heart in the fetus.
- disruption of the growth and development of the child after birth.
GDM also increases the risk of miscarriage - the blood vessels of the placenta are “saturated” with glucose, which leads to impaired blood flow and hypoxia (oxygen starvation) of the fetus, which provokes premature labor in the uterus.
Preventing Gestational Diabetes
Unfortunately, there are no 100% effective measures that would protect against this disease.
But the more useful habits a woman develops before pregnancy, the easier pregnancy and childbirth will be:
- From the first days of pregnancy, eat healthy foods: choose foods high in fiber and low in fat. Focus on vegetables and whole grains. Strive for variety and watch portion sizes.
- Stay active. Try to devote 30 minutes to sports every day. Take daily walks, ride a bike, or go swimming.
- Plan your pregnancy at a healthy weight and don't gain more than recommended. Excessively rapid weight gain can increase the risk of gestational diabetes.
Although there is no universal protection against GDM, you can reduce your risk of developing it through a healthy lifestyle.
The most important thing is to detect the problem in time and prevent it from developing. Author:
Baktyshev Alexey Ilyich, General Practitioner (family doctor), Ultrasound Doctor, Chief Physician
After childbirth
Gestational diabetes is a disease characteristic of pregnancy. After childbirth, GDM goes away as hormonal levels return to normal.
However, we must not forget that GDM is a risk factor for the development of type 2 diabetes mellitus and recurrent disease during the next pregnancy.
Immediately after birth, if insulin therapy was prescribed, it is canceled. During the first days, glucose levels are monitored by collecting venous blood. If there are no abnormalities, a glucose tolerance test is performed 6–12 weeks after birth to rule out type 2 diabetes.
If GDM was diagnosed during pregnancy, it is necessary to follow a diet and engage in dosed physical activity. Otherwise, there are no restrictions; after GDM you can breastfeed as usual.
Features and nuances during pregnancy
A woman should psychologically prepare for the fact that carrying a child with diabetes will require many restrictions, hospital visits and constant monitoring. At the beginning of the period, the patient’s tolerance to carbohydrates should improve and therefore the amount of insulin consumed is reduced.
Already in the middle of pregnancy, it will return to its original level, because the placenta actively begins to function and produces counter-insular hormones - prolactin and glycogen.
The dangerous period is the fourth gestational month. At this time, the baby’s pancreas is already functioning and responding to maternal blood. If the amount of sugar is increased, the fetal pancreas injects insulin, which causes glucose to break down and be converted into fat. As a result, the child rapidly gains weight.
During pregnancy, a woman spends some time in a hospital setting:
- for the first time in the period from 8-10 weeks, for examination and identification of contraindications;
- then 5-6 gestational months, the child’s condition and possible pathologies are assessed;
- at 8 months to determine the type of delivery: cesarean section or natural way.
Pregnancy progresses differently, depending on the form of diabetes. Insulin dependent is more common. Women with this diagnosis need to take insulin for nine months; the exact dosage will be prescribed by an endocrinologist. Usually the following scheme is supported:
- at the beginning of gestation, the amount of the hormone is reduced by 25-30%;
- second trimester - on the contrary, increase the daily dose, it is approximately 80-100 units;
- before childbirth it is lowered again.
The non-insulin-dependent form of the disease in women giving birth practically does not occur. This is due to the fact that such diabetes develops after 40 years, and conception at this age occurs very rarely.
Another type of pathology that develops exclusively during pregnancy is gestational diabetes mellitus. After childbirth it completely disappears. It usually develops at the end of the term and the causes of its occurrence still remain unexplored. Doctors are more inclined to believe that it appears due to the heavy load on the pancreas.
Symptoms of complications:
- constant hunger;
- acute desire to drink;
- swelling;
- frequent urination;
- increase in blood sugar.
To diagnose this type of pathology, it is necessary to pass a glucose tolerance test. The referral is issued by the attending physician. Often the patient does not suspect that she has a latent form of diabetes, and the symptoms are usually attributed to simple malaise during pregnancy.
Therefore, you need to know what contributes to pathology:
- overweight;
- polycystic ovary syndrome;
- gestational diabetes in previous pregnancies;
- the presence of sugar in urine before conception and at the beginning of pregnancy.
Diabetes diagnosed in time can be corrected.
Preventive measures to prevent the development of diabetes mellitus during pregnancy
It is quite difficult to prevent the development of gestational diabetes mellitus with a high degree of probability. Often, women at risk do not develop diabetes mellitus during pregnancy, but pregnant women who do not have any prerequisites may develop the disease. However, planning a pregnancy if you have already had gestational diabetes mellitus once must be done responsibly and perhaps no earlier than 2 years after the previous birth. To reduce the risk of recurrence of gestational diabetes mellitus, several months before the expected pregnancy, you should begin to monitor your weight, include physical exercise in your daily routine, and monitor your blood glucose levels.
Taking any medications must be coordinated with your doctor, since uncontrolled use of certain medications (birth control pills, glucocorticosteroids, etc.) can also provoke the subsequent development of gestational diabetes mellitus.
1.5-2 months after birth, women who have had gestational diabetes need to be tested to determine blood glucose levels and undergo a glucose tolerance test. Based on the results of these studies, the doctor will recommend a specific diet and physical activity regimen, and will also determine the timing for control tests.
Prevention
Photo: olezhkalina / freepik.com
The main measure to prevent GDM is weight control and careful planning of pregnancy.
Obesity is one of the main risk factors for the development of GDM. The more fat there is in the body, the less responsive its cells become to insulin's commands to capture glucose from the blood.
Important! Trying to lose weight during pregnancy is not worth it. You must eat enough so that the fetus does not suffer from lack of nutrients.
Forecast
Timely treatment of GDM with insulin reduces the risk of complications by 98%. Severe consequences after the disease are observed if the diagnosis is not made in time and there is no treatment.
Important! GDM occurs unnoticed, but can cause great harm to the child, causing:
- various fetal malformations,
- Macrosomia (large fetal size),
- Hypoglycemia and respiratory disorders in a newborn,
- Cardiovascular and neurological diseases,
- Metabolic syndrome (carbohydrate metabolism disorder).
The worst outcome is intrauterine fetal death and miscarriage.
However, GDM increases the risk of developing type 1 and type 2 diabetes in the future. The probability of developing type 1 diabetes is 5.7% over the next 7 years, type 2 - up to 50%.
A child born to a mother with GDM also has an increased risk of obesity and diabetes.