Atherosclerosis of the arteries of the lower extremities leads to narrowing of the lumens of blood vessels. Such atherosclerosis is called obliterating (the abbreviation OASNK is used - obliterating atherosclerosis of the vessels of the lower extremities).
What is atherosclerosis
Atherosclerosis is a chronic systemic disease in which pathological changes occur in the arteries - the vessels through which oxygenated blood is carried from the heart throughout the body. The disease is associated with the deposition in the vascular walls of arteries of modified lipids - low molecular weight, water-insoluble substances, primarily fats, of which cholesterol plays the largest role in the development of atherosclerosis. Lipid deposits form plaques that narrow the lumen of blood vessels, as a result of which the flow of arterial blood is hampered and may even stop completely (vascular blockage).
Atherosclerosis is a systemic disease, that is, with the development of favorable factors, the formation of lipid plaques can occur in various parts of the arterial system. However, as a rule, at the stage of manifestation of symptoms, the disease occurs with primary damage to one or more groups of vessels.
More information about atherosclerosis
Atherosclerosis of the arteries of the lower extremities
is a type of disease characterized by predominant damage to the terminal (end) section of the abdominal aorta and its main branches, including the femoral arteries.
If pathological changes lead to a narrowing of the lumen of blood vessels, then such atherosclerosis is called obliterating (the exact medical diagnosis of OASNK
is
obliterating atherosclerosis of the vessels of the lower extremities
).
Obliterating atherosclerosis is the most common disease of the arteries of the lower extremities. It appears mainly in men, starting from 50-60 years, in women - from 60-70 years. At the age of 65 years and older, obliterating atherosclerosis of the lower extremities is detected in approximately 10% of the population.
Narrowing of blood vessels in the legs: causes
Stenosis is a pathology of the cardiovascular system, often affecting the vessels of the legs. Narrowing of the arteries of the lower extremities is caused by deposits formed inside the vessel. In the vast majority of clinical cases, deposits are formed due to increased concentrations of lipids in the blood plasma. An excess of these fat-like organic compounds forms fat accumulations on the vascular walls. The most famous lipid is cholesterol. By combining with calcium, which plays a structural role, and connective tissue substances, cholesterol is converted into cholesterol plaques. Therefore, stenosis, despite its local nature, is a manifestation of atherosclerosis.
Narrowing of the blood vessels in the legs also occurs for a number of other reasons, independent of disorders in the body’s fat metabolism. A common cause of stenosis is considered to be genetics. A hereditary feature, namely a predisposition to a particular disease, manifests itself depending on the accumulation of pathological genes. As soon as their interaction with environmental factors of varying strength reaches its maximum, a person notices signs of a disease that was previously diagnosed in his close relatives.
Many other pathological processes and diseases are quite capable of causing narrowing of the arteries of the legs. Among them:
- hypertension (disturbs normal blood circulation);
- thyrotoxicosis and diabetes mellitus of any type (provoke metabolic disorders);
- arteritis, vasculitis and various diseases characterized by inflammation of the arteries of the legs (reduces vascular patency);
- calculous cholecystitis in a complicated form (disturbs the functioning of blood vessels);
- diseases of the hematopoietic system;
- oncology, etc.
!
Narrowing of the arteries of the lower extremities can occur under the influence of harmful addictions.
Smoking and alcohol abuse cause vascular spasms, which prevent the normal movement of blood through them. Alcohol negatively affects red blood cells. Under its influence, their shell is destroyed. Red blood cells stick together, forming clots and leading to partial blockage of the artery. Blood cannot freely penetrate through the remaining lumen of the vessel. An incorrectly organized lifestyle (overeating, lack of exercise, unstable emotional background, etc.) leads to metabolic disorders and poor circulation.
Vessels in the legs are also narrowed due to injuries, hypothermia or overheating of the body. Age-related changes, which reduce the elasticity of the vascular walls, also affect their narrowing. The list of causes that cause stenosis of the vessels of the legs is very wide. Therefore, it is extremely important to know the symptoms of the disease. More on this later in our article.
Narrowing of blood vessels in the legs - symptoms
What are the causes of stenosis?
There are many different causes of stenosis. The main ones:
- Congenital malformations (for example, congenital urethral valves, congenital intestinal obstruction due to intestinal underdevelopment).
- Proliferative inflammation of the organ wall is an inflammatory process in which tissue proliferation occurs.
- Scarring of the organ wall after damage, inflammation, or ulcers.
- Benign and malignant tumors.
- In vessels, the cause of stenosis is often blood clots and atherosclerotic plaques.
- Compression of a hollow organ from the outside, for example, by a tumor located in a neighboring organ.
- Hypertrophy of the organ wall - for example, this condition often causes narrowing of the pylorus of the stomach.
- Injuries and osteophytes (bone growths) can cause stenosis of bone canals, in particular the spinal canal.
Narrowing of blood vessels in the legs: symptoms and consequences
Vasoconstriction of the lower extremities has several stages of development. And not all of them have clear symptoms. The first stage can be called asymptomatic. The patient does not notice any changes in his condition or does not attach much importance to them.
Vasoconstriction makes itself felt gradually. As the disease progresses, the nutrition of tissue cells deteriorates due to insufficient blood supply. Some patients begin to notice that their legs feel cold and sensitivity is impaired. And only then do they wonder what is happening to them? This means that the symptom complex of the pathology is increasing. In its manifestations, this is called obliterating atherosclerosis and is characterized by the following unpleasant sensations in the lower extremities:
- a feeling of tingling and burning in the feet;
- pain in the ankle and toes;
- intermittent claudication syndrome;
- increased sweating;
- swelling;
- cyanosis;
- hypertension, etc.
Due to the fact that the disease is detected in late stages, the symptoms are already its consequences. Therefore, along with the above symptoms, patients are faced with:
- necrosis and rotting of soft tissues;
- muscular atrophy of the lower extremities;
- dysfunction of the pelvic organs;
- trophic ulcers.
The above consequences mean that the disease is already severe, and may lead the patient to subsequent disability.
Expert opinion
Not only the localization of pathology in the veins of the lower extremities, but also in the arteries can lead to dangerous consequences for the health and even the life of the patient. In particular, stenosis of cerebral vessels deserves special attention. A gradual decrease in the lumen of the veins and arteries that supply the brain leads to a decrease in the volume of nutrients necessary for the normal functioning of the brain. This leads to the development of neurological problems, the most dangerous of which is stroke.
Vascular surgeon, phlebologist
Osipova Ekaterina Yakovlevna
Statistics on the development of deep vein thrombosis by disease
How is the examination performed?
If you suspect stenosis of the lower extremities in the Israeli clinic named after. Rabin carries out a highly informative examination program, which begins with a thorough study of the course of the disease and the patient’s complaints. Ultrasound classification of stenosis is mandatory.
The patient is prescribed:
- Doppler ultrasound;
- duplex ultrasound scanning;
- computed axial tomography;
- magnetic resonance angiography with the introduction of a contrast agent.
The vascular surgeon measures blood pressure in the shoulder and ankle area, determining the frequency and quality of the pulse. The patient undergoes extended blood biochemistry. If there are concomitant chronic diseases, an examination is performed by related specialists of the medical center.
Narrowing of blood vessels in the legs: how is stenosis diagnosed?
What to do if symptoms of the disease are detected? In order to avoid an unfavorable prognosis due to narrowing of the blood vessels in the legs, you should plan a visit to the doctor as soon as possible. During it, the specialist will:
- a thorough survey to judge the development of a particular disease, its possible causes, and also to preliminarily assess the severity of the patient’s condition;
- examination of the legs to assess the condition of the skin;
- palpation of the extremities for pain, pastiness and compaction along the vessels.
After a physical examination, the doctor prescribes the necessary laboratory diagnostics of the patient’s condition. This may include:
- general clinical tests;
- extended hemostasiogram;
- lipid profile;
- immunogram;
- D-dimer test;
- analysis of blood composition for gases and acidity.
Diagnosis of narrowing of blood vessels in the legs
In turn, instrumental diagnosis of the disease is carried out in various ways: Dopplerography, duplex and triplex scanning, sonography, X-ray contrast angiography, electrocardiography, EchoCG, infrared thermography, rheoencephalography, etc. The most informative methods are considered to be contrast angiography and tomography with contrast. The selection of the optimal diagnostic method or their combination is made by the doctor individually in each specific case.
Vasoconstriction of the lower extremities: treatment
If, after going through all the stages of the examination, the doctor diagnoses a patient with narrowing of blood vessels in the legs, then the question arises, how and with what to treat it? Treatment methods depend on the causes that caused it, the stage at which vasoconstriction of the lower extremities was detected, and the patient’s concomitant diseases. So, for example, treatment for a patient with diabetes will differ from the therapeutic regimen prescribed for a patient with heart disease. Therefore, the choice of treatment should be made only by a doctor who can take into account all available and possible nuances.
At the moment, patients who are found to have narrowing of the blood vessels in their legs are offered medication, physiotherapy and surgical treatment. In consultation with your doctor, additional treatment with folk remedies is possible.
Let's start with the fact that special importance is given to maintaining a healthy lifestyle and rational food intake.
!
It is important to give up bad habits, get moderate physical activity, have a harmonious daily routine and eat right.
So, to strengthen the walls of blood vessels, you should add nuts, berries, fruits (no more than 2 fruits per day), legumes, cruciferous vegetables, garlic, bone broths, etc. to your diet. If these recommendations are not followed by the patient, then any treatment method will be ineffective .
The drug treatment method primarily involves taking medications that increase elasticity and reduce vascular permeability. Narrowing of the blood vessels in the legs requires combined treatment with medications. Therefore, when considering how to help a patient with pain in the legs, the doctor may prescribe antispasmodics, analgesics and non-steroidal anti-inflammatory drugs. In addition, antiplatelet agents, diuretics, antihypertensive and other drugs are prescribed. With an integrated approach, treatment with folk remedies is acceptable to cleanse the vessels of the lower extremities and reduce the pathological signs of the disease. For these purposes, infusions of peony, motherwort, valerian, rowan, etc. are used.
Treatment of vasoconstriction in the legs
In some cases, physiotherapy methods are used to achieve maximum therapeutic effect. First of all, these are therapeutic exercises and massage, which can be performed even at home. Electrophoresis and laser therapy are also used in hospital settings.
What to do if vasoconstriction in the legs is detected in the later stages? If the disease is detected at stage 2 and beyond, then you will still have to take medications, but surgery cannot be avoided. With stenotic disorders at these stages, the narrowing of the blood vessels in the legs reaches 50% or higher, which can lead to death. Surgical treatment methods include: endarterectomy, bypass surgery, prosthetics, thrombectomy. The result of treatment will be the expansion of the lumen between the walls of blood vessels and improved blood supply to the lower extremities.
Treatment
First of all, when treating vascular stenosis, it is necessary to follow a diet, increase physical activity and give up bad habits. In addition, the patient is prescribed medications to dilate blood vessels, accelerate blood flow, and lower cholesterol levels. In some cases, surgery is recommended.
Stenting can quickly and effectively restore blood flow and eliminate stenosis. This is one of the most modern methods of treating vascular diseases accompanied by impaired arterial patency. It is characterized by minimal trauma to the patient. In this case, the effect on the vessel is carried out from the inside, using a special catheter inserted through a micropuncture into the artery. The essence of such operations as stenting of the carotid arteries, heart vessels or limbs is that an endoprosthesis (stent) is installed at the site of narrowing, which acts as a frame and holds the vascular walls. These operations are the safest and give the best results.
Video: What is vasoconstriction and how to deal with it
is not responsible for the accuracy of the information presented in this video clip. Source - Medservice Izhevsk
Sources:
- Karpenko A.A., Starodubtsev V.B., Ignatenko P.V., Zoloev D.G. Hybrid surgical interventions in patients with multilevel atherosclerotic lesions of the arteries of the lower extremities // Angiology and Vascular Surgery. 2014. T. 20, No. 2.
- Bondarenko M.A., Lebedeva E.A., Artyushin B.S. Biomechanical method for studying the influence of atherosclerotic lesions on hemodynamics in the arteries of the lower extremities // Proceedings of St. Petersburg Electrotechnical University "LETI". 2015. No. 9.
- Begun P.I., Krivokhizhina O.V., Sukhov V.K. Computer modeling and biomechanical analysis of critical condition and correction of structures of the vascular system (Part I) // Management in medicine and biology. 2005. No. 6.
- OBLITERATING ATHEROSCLEROSIS OF THE LOWER LIMB IN ELDERLY PEOPLE. Polyakov P.I., Gorelik S.G., Zheleznova E.A. // Bulletin of new medical technologies. – 2013. – No. 1. – P. 98-101.
- DIAGNOSTICS OF THROMBOTIC PROCESSES IN THE VEINS OF THE LOWER LIMB IN OUTPATIENT PRACTICE. Vlasova I.V., Tleubaeva N.V., Vlasov S.V., Pronskikh I.V. // Polytrauma. – 2011. –№3. – P. 65-75.
- https://iliveok.com/health/disease-peripheral-vessels-legs_112749i16070.html
- https://medlineplus.gov/ency/article/000170.htm
For an accurate diagnosis, contact a specialist.
Dear patients!
Obliterating atherosclerosis, causes
Obliterating atherosclerosis is the appearance of cholesterol plaques in the thickness of the walls of the arteries, leading to narrowing and blockage (obliteration) of the artery and disruption of the blood supply to the organ or tissue that the altered artery supplies.
Atherosclerotic plaques can occur in any arteries of the human body, including those found in the arteries of the lower extremities. This leads to the development of a disease - obliterating atherosclerosis of the lower extremities.
The occurrence of atherosclerotic plaques occurs due to many reasons. The role of metabolic disorders in this process, in particular disorders of fat metabolism in the body, is important. Genetic predisposition to this disease also plays a role, as well as such important factors as smoking, diabetes, poor diet, sedentary lifestyle, obesity, high blood cholesterol, and arterial hypertension. Among patients with obliterating atherosclerosis of the lower extremities, men significantly predominate.
According to the Ministry of Health of the Russian Federation, 5-15% of the population suffers from chronic obliterating diseases of the lower extremities.
The main age of patients with obliterating atherosclerosis of the lower extremities is 60-69 years in men, 70-79 years in women, but atherosclerosis has recently become rapidly “younger”.
Symptoms of obliterating atherosclerosis of the arteries of the lower extremities
The most common symptom of atherosclerotic lesions of the arteries of the lower extremities is intermittent claudication. Patients note pain, cramps, numbness that occurs when walking and goes away at rest, in the muscles of the thigh, gluteal region (high intermittent claudication), and lower leg (low intermittent claudication). This is a sign that at rest the muscles of the lower limb are sufficiently supplied with blood, and during physical activity the narrowed artery cannot deliver enough blood, and oxygen starvation occurs.
With further narrowing of the artery, up to its complete blockage (occlusion), pain begins to appear even with less load (a clear criterion is the distance traveled after which pain appears), then they continue to bother you even at complete rest. In this case, a lower position of the leg helps relieve pain. Pain at rest indicates a complete blockage of the artery; in this case, the blood supply is provided by collaterals - small arteries running in parallel, bypassing the blocked (occluded) artery.
With further aggravation of the condition, non-healing ulcers begin to appear on the skin, they gradually increase in size and deepen until they die completely - gangrene. Gangrene usually begins with the toes; in the absence of adequate treatment, the height of the spread of gangrene is determined by the level and degree of changes in the arteries.
One of the simplest and most objective studies of the extent of arterial damage is ultrasound duplex scanning of the arteries. Using an ultrasound sensor, you can see both the narrowed areas and the degree of their narrowing. When, due to the deterioration of the patient’s condition, it becomes clear that surgery is no longer possible, angiography is performed - an X-ray examination of the vessels through a puncture, using a catheter and a contrast agent.
Treatment of obliterating atherosclerosis of the lower extremities
Treatment tactics for each patient are developed individually and depend on the level, extent and extent of arterial damage, and the presence of concomitant diseases. However, there are general patterns that correspond to the severity of symptoms:
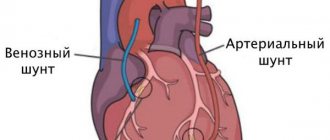
Intermittent claudication suggests the presence of a narrowed section of the artery. In most situations, endovascular treatment is effective: dilatation or stenting of a narrowed arterial vessel.
For pain at rest, it is assumed that there is a completely blocked section of the artery with blood supply to the leg through collaterals. In this case, endovascular treatment is used if it is possible to pass a catheter through the blocked area - which is often only possible with small blockages (occlusions). For long occlusions, surgical treatment methods are more applicable: open removal of atherosclerotic plaques (endarterectomy), or replacement of the affected area with a vein or tissue prosthesis (bypass surgery). In case of multiple lesions, combined operations are often used - bypassing the occluded section of the artery and dilatation (or stenting) of the narrowed one.
The presence of ulcers or gangrene is a sign of extensive arterial occlusions, multi-level lesions of arteries with weak collateral blood flow. Surgical treatment options in this case are reduced. Endovascular treatment can be used in combination with open surgery. If it is impossible to perform arterial reconstruction, or if it is ineffective, amputation of the affected limb is performed.
Important! The smaller the atherosclerotic damage to the artery, the simpler, more successful and cheaper the treatment. Therefore, the most favorable stage for treatment of obliterating atherosclerosis of the lower extremities is the stage of intermittent claudication.
If the described symptoms occur, urgent consultation with a vascular or endovascular surgeon is necessary. By postponing the start of treatment “until better times,” you contribute to the progression of the disease and increase the likelihood of amputation in the near future.
Endovascular treatment of obliterating atherosclerosis of the arteries of the lower extremities
In the cath lab, under completely sterile conditions, the endovascular surgeon punctures the femoral or other artery and inserts a catheter into the artery. The catheter is brought to the affected arterial area, a contrast study is performed - angiography, which makes it possible to clarify the extent and degree of narrowing (occlusion). A conductor is passed through the affected area - a metal string with a soft tip. A catheter balloon is installed along the guide into the affected area - a catheter with a plastic balloon inflated under high pressure to a strictly defined diameter. Then the balloon is inflated (dilated) at the site of narrowing. In this case, atherosclerotic plaques are pressed into the artery wall and smoothed out evenly, the lumen of the vessel increases. Control angiography is performed. If restoration of arterial patency is satisfactory, the procedure is completed. If a narrowed or closed area remains (elastic narrowing, external compression, bending), a stent is installed at the site of the lesion - a mesh metal structure, expanded by a balloon and reinforcing the lumen of the artery from the inside, preventing it from collapsing. After the patency of the artery is restored, the endovascular instruments are removed from the artery, the puncture site is pressed with a hand for 5-10 minutes (until bleeding from the puncture site stops), then a pressure bandage is applied and bed rest is prescribed until the next morning. Anticoagulants (heparin, fraxiparin, clexane) can be prescribed for several days, after which the patient continues to take the long-term antiplatelet agent prescribed for this disease (thrombo-ASA, aspirin-cardio, cardiomagnyl, cardio-ASA).
results
Immediately after restoration of arterial patency, the volumetric velocity of blood flow in the arteries of the limb increases, and the pulse is restored in the underlying arterial segments. If a limb has been left for a long time under conditions of insufficient blood supply, restoration of blood flow can lead to the so-called hyperperfusion/reperfusion syndrome. Unusually high blood flow causes redness of the limb, swelling, and sometimes pain. This condition goes away after a few days, after the limb “gets used” to the new conditions of blood supply.
Side effects, complications, relapses
In the presence of arterial lesions of both lower extremities, restoration of blood flow in one of them can lead to depletion of blood flow in the other. As a result, after surgery, intermittent claudication may appear on a limb that was previously considered healthy (which is a manifestation of the presence of previously undiagnosed obliterating atherosclerosis in it). Therefore, it is important to initially examine both limbs, even if painful symptoms are present on only one side.
The most common complication during endovascular interventions is puncture site hematoma. This complication does not require additional hospitalization; in the vast majority of cases it is treated conservatively.
Complications at the site of arterial damage (arterial thrombosis, partial or complete rupture of the artery) are relatively rare, their frequency depends on the experience of the surgeon, the quality of equipment, instruments and the severity of arterial damage. For example, the presence of calcification (long-existing arterial plaques accumulate calcium) increases the likelihood of rupture of the arterial wall when it dilates. In most cases, such complications can be eliminated endovascularly, or, if necessary, with open surgery.
Re-emergence or worsening of symptoms of arterial insufficiency can be caused by repeated narrowing of the dilated arterial segment or growth of the intima (inner lining of the artery) at the site of the stent. In this case, repeated endovascular interventions are performed, and if they are ineffective, surgical treatment is performed. However, most often, repeated narrowing of the arteries of the lower extremities is associated with the progression of atherosclerosis.
Continued growth of atherosclerotic plaques may create the need for repeated endovascular or surgical interventions. Therefore, it is especially important for patients with obliterating atherosclerosis to correct risk factors for the progression of atherosclerosis: strive to normalize blood pressure and blood cholesterol levels, quit smoking, follow a certain diet, change the mode of physical activity - that is, completely, sometimes radically change their lifestyle. All this is necessary in order to stabilize and slow down the further development of atherosclerosis. Only in this case, the results of any treatment for arterial insufficiency of the lower extremities will be long-term.
Clinical cases
Clinical case No. 1
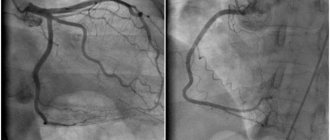
A patient complained of intermittent claudication and pain in both legs occurred at a walking distance of 50 m.
The angiogram shows pronounced stenoses of the common iliac arteries on both sides (Fig. 1).
Balloon-expandable stents were installed into the areas of stenosis under local anesthesia through radial access (puncture on the forearm) (Fig. 2 and 3).
rice. 1 pic. 2 fig. 3
Stenoses were completely eliminated (Fig. 4).
Pain in the legs with minimal exertion no longer bothers the patient.
The pain-free walking distance has increased significantly.
rice. 4
Clinical case No. 2
A patient with diabetes mellitus complained of a non-healing trophic ulcer on the foot, in the bed of the removed 3rd toe (the toe was removed at the place of residence due to its gangrene), incipient gangrene of the 1st and 2nd toes of the right foot.
The angiogram shows occlusion of one of the tibial arteries at the level of the right ankle joint, its subocclusion in the lower third of the leg; the blood supply to the foot is provided by a single artery (Fig. 5).
rice. 5 (before intervention) Fig. 6 fig. 7
rice. 8 fig. 9
Balloon angioplasty of the arteries on the leg and foot was performed (Fig. 6, 7, 8, 9).
The main blood supply to the foot has been completely restored (Fig. 10 - angiogram of the right foot and lower third of the leg). Good conditions have been created for the healing of fingers and trophic ulcers. See photos of the foot before, one month, 3 months after angioplasty (the initially long-term non-healing bed after removal of the gangrenous toe quickly healed after angioplasty; the incipient gangrene of the 1st and 2nd toes was stopped - the toes were completely healed).
rice. 10
Photo of the foot before angioplasty Photo of the foot 1 month after angioplasty
Photo of the foot 3 months after angioplasty
Clinical case No. 3
The patient was admitted with critical ischemia of the only left lower limb due to acute thrombosis of the main arteries of the limb (incessant pain in the leg at rest, the leg below the inguinal fold is cold, marbled in color). In 2010 he had already been admitted with a similar condition of the right lower limb, when, despite the full scope of treatment, including a thrombectomy (removal of blood clots) performed by a vascular surgeon called from the republican hospital, gangrene of the limb eventually began to develop, and it had to be amputated.
In the present situation, clinical thrombosis of the arteries of the limb occurred 2 weeks ago, but the patient presented only 2 weeks later as a result of progressive deterioration of the limb.
The angiogram shows thrombotic occlusion of the arteries of the limb below the level of the inguinal fold (Fig. - top row). The patient underwent selective thrombolysis (administration of a drug that dissolves blood clots) through a catheter inserted under local anesthesia through radial access (wrist puncture) and lowered into the left lower limb to the level of thrombosis. The thrombolytic drug was administered for 1 day. Despite the 2-week period of thrombosis, the blood clots were completely dissolved, and the main blood supply to the limb was completely restored (Fig. - bottom row). The patient's complaints completely resolved. Thus, it was possible to save the limb from amputation, and the patient was discharged in satisfactory condition. Photo below: top row - before the intervention, bottom row - the result of treatment.
Clinical case No. 4
Similar example. The patient was admitted with critical ischemia of the left lower limb due to thrombosis of the main arteries of the limb (incessant pain in the leg at rest, the leg below the inguinal fold is cold, marble-colored).
Clinically, thrombosis of the arteries of the limb also occurred 2 weeks ago, but the patient came only 2 weeks later as a result of a progressive deterioration in the condition of the limb.
The angiogram shows occlusion of the arteries of the limb below the level of the knee joint ( Fig. - top row ). Over the course of 1 day, the patient underwent selective thrombolysis (administration of a drug that dissolves blood clots) through a catheter inserted under local anesthesia through an access on the wrist and lowered into the left lower limb to the level of thrombosis. This method of treatment made it possible to completely dissolve blood clots, despite the 2-week period of thrombosis, the main blood supply to the limb was completely restored ( Fig. - bottom row ). As a result, the patient's complaints resolved completely. Thus, it was possible to save the limb from amputation, and the patient was discharged in satisfactory condition. Photo below: top row - before the intervention, bottom row - the result of treatment.
Clinical case No. 5
The patient was admitted with critical ischemia of the right lower limb due to thrombosis of the main arteries of the limb (incessant pain in the leg at rest, the leg below the inguinal fold is cold, marbled in color).
In the present situation, clinical thrombosis of the arteries of the limb occurred 3 days ago, but the patient came only 3 days later as a result of a progressive deterioration in the condition of the limb.
The angiogram shows a short occlusion of the femoral artery above the level of the knee joint, occlusion of all arteries of the limb below the level of the knee joint ( Fig. - top row of photos ). The patient underwent selective thrombolysis through a catheter inserted under local anesthesia through radial access and reduced to the level of thrombosis in the right lower limb. The thrombolytic drug was administered for 1 day. Despite the 3-day period of thrombosis, the blood clots were dissolved, the main blood supply to the limb was restored, with the exception of the local area below the knee ( Fig. - second row of photos ). Balloon angioplasty of this area was performed, after which the main blood supply to the limb was completely restored (Fig. - third row of photos) . The patient’s complaints completely resolved. Thus, it was possible to save the limb from amputation, and the patient was discharged in satisfactory condition. Photo below: top row - before the intervention, bottom row - the result of treatment.
Clinical case No. 6
A patient complains of intermittent claudication, pain when walking, mainly in the muscles of the right leg below the knee at a walking distance of 100 m. The angiogram shows a short occlusion of the right femoral artery at the level above the knee joint. Balloon angioplasty of the occlusion area was performed with good angiographic and clinical results. The pain-free walking distance increased significantly. Photo below: the progress of the surgical intervention (before angioplasty - the moment of balloon inflation - the result of balloon angioplasty).
Clinical case No. 7
A patient complains of intermittent claudication, pain when walking, mainly in the muscles of the right leg below the knee, and a progressive decrease in the pain-free walking distance. In the past, the patient underwent femoral-popliteal bypass surgery using his own vein. The angiogram shows critical stenosis of the shunt at the level above the knee joint. Balloon angioplasty of the area of critical stenosis was performed with a good angiographic and clinical result. The pain-free walking distance increased significantly. Photo below: the progress of the surgical intervention (before angioplasty - the moment of balloon inflation - the result of balloon angioplasty). Angioplasty in this situation extended the life of the venous shunt and made it possible to avoid repeated open vascular surgery.
Clinical case No. 8
A patient complains of pain in the muscles of the right leg below the knee. The angiogram shows chronic occlusion (blockage) of the popliteal artery. Recanalization and balloon angioplasty of the occlusion area were performed. However, the result of angioplasty was regarded as insufficient and the intervention was supplemented with stenting with good angiographic and clinical results. The rest pain disappeared. Also, after the intervention there was no intermittent claudication. Photo below: the progress of the surgical intervention (the first row of photos is the area of occlusion before and after angioplasty, the flexion test shows the absence of compression of the stent when bending the knee joint; the following photos show blood flow below the knee joint before and after intervention).
Endovascular treatment of obliterating atherosclerosis. conclusions
Steady progress in manufacturing technologies for endovascular instruments, the emergence of new devices, improvement of catheterization techniques and the emergence of new treatment methods in recent years have led to a significant expansion of indications for endovascular reconstructive operations on the arteries of the lower extremities, improved treatment results and reduced the number of complications and relapses.
The experience accumulated by specialists allows us to recommend endovascular methods for the treatment of obliterating atherosclerosis to everyone who is faced with the problem of choosing a method of treating this disease.
You can ask questions related to angiographic and X-ray endovascular interventions at Medservice LLC:
Tel.
Email mail
Ivanov Andrey Gennadievich (head of the department of x-ray surgical methods of diagnosis and treatment, doctor of the highest category in the specialty “endovascular diagnostics and treatment”)