Phlebitis is an inflammatory process localized on the venous wall. Phlebitis develops under the influence of various factors: infectious diseases, allergic reactions, mechanical irritations and others. But most often the disease occurs as a result of complications of varicose veins of the lower extremities. In most cases, in the absence of proper treatment, inflammation of the venous wall leads to the formation of blood clots, and phlebitis progresses to the next stage - thrombophlebitis.
Classification
There are many pathogenic factors that provoke the occurrence of phlebitis. Depending on them, the following types of disease are distinguished:
- Migratory. Most often observed in men and affects the superficial veins of the arms and legs;
- Infectious. Develops due to the influence of infectious agents and can be localized in any venous vessel of the body;
- Pylephlebitis. Inflammatory process in the portal vein of the liver. Occurs as a consequence of inflammatory processes in the abdominal cavity or is a complication of appendicitis;
- Aseptic. Occurs due to mechanical irritation of the inner lining of the vein. For example, due to the long stay of the catheter in the vein or the administration of an aggressive drug.
Also, depending on the nature of the disease, acute and chronic forms of phlebitis are distinguished.
Complications
Most often, thrombophlebitis is complicated by the spread of blood clots to the deep veins with the development of deep vein thrombosis and thromboembolism. The frequency of this complication is about 10% of all patients.
Purulent thrombophlebitis develops when an infection joins the inflammatory process. Suppuration is characterized by a sharp increase in temperature, chills, and a change in the number of leukocytes in the blood. Purulent thrombophlebitis can lead to the development of sepsis - a general blood infection and therefore requires emergency surgical care.
Symptoms of phlebitis
The disease is characterized by the following symptoms:
- The affected vein is painful and tense;
- The skin over the affected area turns red and thickens;
- Red stripes appear along the inflamed vein;
- In the acute form of phlebitis, severe pain appears, the color of the affected limb may change to white;
- If a vein in the arm is inflamed, the pain becomes more intense when lowering the arm down. In this case, the pain is pulsating in nature and often intensifies at night;
- With pylephlebitis, purulent intoxication is observed, which is characterized by vomiting, weakness, headache, pain in the right hypochondrium;
- Symptoms of cerebral phlebitis are headache, high blood pressure, and various neurological symptoms.
Thrombophlebitis of the superficial veins: diagnosis and treatment
D
This type of pathology is a very common disease of the venous system, which is encountered by doctors of any specialty.
Currently, terms such as phlebothrombosis and varicothrombophlebitis are also often used in medical practice. All of them are legal to use, but the following points should be taken into account. Phlebothrombosis is considered as an acute obstruction of a vein as a result of hypercoagulation, which is the leading mechanism. But after 5–10 days, the resulting thrombus causes reactive inflammation of the tissues surrounding the vein with the development of phlebitis, that is, phlebothrombrosis transforms into thrombophlebitis
.
The term “varicothrombophlebitis” clearly indicates, in fact, the initial cause of thrombosis that occurs against the background of varicose veins that the patient already had.
The pathology of the venous system listed above in the overwhelming majority of clinical cases occurs in the large saphenous vein system and much less often in the small saphenous vein system.
Thrombophlebitis of the veins in the upper extremities is extremely rare, and the main provoking factors for their occurrence are multiple punctures for administering medications or prolonged placement of a catheter in a superficial vein.
Particular attention should be paid to patients with spontaneously occurring thrombi on the upper and lower extremities, not associated with iatrogenic effects. In such cases, the phenomenon of thrombophlebitis can be suspected as a manifestation of a paraneoplastic reaction caused by the presence of an oncological pathology in the patient, requiring an in-depth multifaceted examination.
Thrombosis in the superficial venous system is provoked by the same factors that cause thrombosis of the deep venous system of the lower extremities. These include: age over 40 years, the presence of varicose veins, cancer, severe disorders of the cardiovascular system (cardiac decompensation, occlusion of the main arteries), physical inactivity after major operations, hemiparesis, hemiplegia, obesity, dehydration, common infections and sepsis, pregnancy and childbirth, taking oral contraceptives, limb trauma and surgical interventions in the area of venous trunks.
Thrombophlebitis can develop in any part of the superficial venous system
, with the most common localization on the lower leg in the upper or middle third, as well as the lower third of the thigh. The overwhelming number of cases of thrombophlebitis (up to 95–97%) were noted in the basin of the great saphenous vein (Kabirov A.V. et al., Kletskin A.E. et al., 2003).
The further development of thrombophlebitis can actually occur in two ways:
1. Relatively favorable course of the disease
, against the background of the treatment, the process stabilizes, thrombus formation stops, inflammation subsides and the process of organizing a blood clot begins, followed by recanalization of the corresponding part of the venous system. But this cannot be considered a cure, because... Damage to the initially altered valve apparatus always occurs, which further aggravates the clinical picture of chronic venous insufficiency.
Clinical cases are also possible when a fibrotic thrombus tightly obliterates the vein and its recanalization becomes impossible.
2. The most unfavorable and dangerous option
in terms of the development of local complications - ascending thrombosis along the great saphenous vein to the fossa ovale or the transition of the thrombotic process through the communicating veins to the deep venous system of the leg and thigh.
The main danger of the course of the disease according to the second option is the threat of developing a complication such as pulmonary embolism (PE), the source of which can be a floating thrombus from the system of the small or great saphenous vein, as well as secondary thrombosis of the deep veins of the lower extremities.
It is quite difficult to judge the frequency of thrombophlebitis among the population, but if we take as a basis the fact that among patients hospitalized in surgical departments with this pathology, more than 50% had varicose veins, then taking into account the millions of patients with this pathology in the country, this figure looks very impressive and The problem is acquiring great medical and social significance.
The age of patients ranges from 17 to 86 years and even older, and the average age is 40–46 years, that is, the working population.
Considering the fact that with thrombophlebitis of the superficial veins, the patient’s general condition and well-being, as a rule, do not suffer and remain quite satisfactory, this creates for the patient and his relatives the illusion of relative well-being and the possibility of various methods of self-medication.
As a result, such behavior of the patient leads to late referral for qualified medical care, and often the surgeon is faced with complicated forms of this “simple” pathology, when high ascending thrombophlebitis or deep vein thrombosis of the limb occurs.
Clinical picture
The clinical picture of the disease is quite typical in the form of local pain in the projection of the saphenous veins at the level of the leg and thigh
with the involvement of the tissues surrounding the vein in the process, up to the development of sharp hyperemia of this zone, the presence of compactions not only of the vein, but also of the subcutaneous tissue. The longer the zone of thrombosis, the more pronounced the pain in the limb, which forces the patient to limit its movement. Hyperthermic reactions in the form of chills and an increase in temperature to 38–39°C are possible.
Quite often, even a banal acute respiratory disease becomes a provoking moment for the occurrence of thrombophlebitis, especially in patients with varicose veins of the lower extremities.
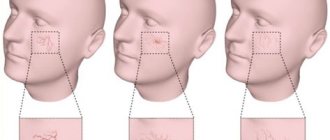
The examination is always carried out from both sides - from the foot to the groin area. Attention is drawn to the presence or absence of pathology of the venous system, the nature of changes in skin color, local hyperemia and hyperthermia, and swelling of the limb. Severe hyperemia is typical for the first days of the disease; it gradually decreases by the end of the first week.
When thrombophlebitis is localized in the small saphenous vein, local manifestations are less pronounced than when the trunk of the great saphenous vein is affected, which is due to the peculiarities of the anatomy. The superficial layer of the shin's own fascia, covering the vein, prevents the transition of the inflammatory process to the surrounding tissues. The most important point is to find out the timing of the onset of the first symptoms of the disease, the speed of their increase, and whether the patient has attempted to influence the process with medication.
So, according to A.S. Kotelnikova et al. (2003), the growth of a blood clot in the great saphenous vein system is up to 15 cm per day. It is important to remember that in almost a third of patients with ascending thrombosis of the great saphenous vein, its true upper limit is located 15–20 cm above the level determined by clinical signs (V.S. Savelyev, 2001), that is, this fact should every surgeon should take into account when advising a patient with thrombophlebitis of a vein at the hip level, so that there is no undue delay in the operation aimed at preventing pulmonary embolism.
It should also be considered inappropriate to administer local anesthetics and anti-inflammatory drugs to the area of the thrombosed vein on the thigh, since, while relieving pain, this does not prevent the growth of the thrombus in the proximal direction. Clinically, this situation becomes difficult to control, and duplex scanning can really only be used in very large medical institutions.
Differential diagnosis
should be carried out with erysipelas, lymphangitis, dermatitis of various etiologies, erythema nodosum.
Instrumental and laboratory diagnostics
For a very long time, the diagnosis of thrombophlebitis of the superficial veins was made by a doctor based only on the clinical symptoms of the disease, since there were virtually no non-invasive methods for characterizing venous blood flow. The introduction of ultrasound diagnostic methods into practice has opened a new stage in the study of this common pathology. But the clinician must know that among ultrasound methods for diagnosing venous thrombosis, the decisive role is given to duplex scanning, since only with its help can one determine a clear boundary of thrombosis, the degree of organization of the thrombus, the patency of the deep veins, the condition of the communicants and the valve apparatus of the venous system. Unfortunately, the high cost of this equipment still sharply limits its practical use in outpatient and inpatient settings.
This study is indicated primarily for patients with suspected embologenic thrombosis, that is, when there is a transition of a thrombus from the superficial to the deep venous system through the sapheno-femoral or sapheno-popliteal anastomosis.
The study can be carried out in several projections, which significantly increases its diagnostic value.
Phlebographic examination
The indications for it have been sharply narrowed. The need to perform it arises only in the event of a thrombus spreading from the great saphenous vein to the common femoral and iliac vein. Moreover, this study is carried out only in cases where the results of duplex scanning are doubtful and their interpretation is difficult.
Laboratory diagnostic methods
In a routine clinical blood test, attention is paid to the level of leukocytosis and the level of ESR.
It is advisable to study C-reactive protein, coagulogram, thrombelastogram, prothrombin index level and other indicators characterizing the state of the coagulation system. But the scope of these studies is sometimes limited by the capabilities of the laboratory service of a medical institution.
Treatment
One of the important points that determine the outcome of the disease and even the fate of the patient is the choice of tactics for the optimal treatment option for the patient.
If thrombophlebitis is localized at the level of the lower leg, the patient can undergo treatment on an outpatient basis, under the constant supervision of a surgeon. In these conditions, it is necessary to explain to the patient and his relatives that if signs of thrombosis spreading to the hip level appear, the patient may need to be hospitalized in a surgical hospital. Delay in hospitalization is fraught with the development of complications, including the occurrence of pulmonary embolism.
In cases where thrombophlebitis at the level of the leg, treated for 10–14 days, does not respond to regression, the question of hospitalization and more intensive treatment of the disease should also be raised.
One of the main issues in the treatment of patients with thrombophlebitis of the superficial veins is the discussion of the need for the patient to comply with strict bed rest
.
It is now a recognized fact that strict bed rest is indicated only for patients who already had clinical signs of pulmonary embolism or there are clear clinical data and the results of instrumental studies indicate the embologenic nature of thrombosis.
The patient's physical activity should be limited only to severe physical activity (running, lifting weights, performing any work that requires significant muscle tension in the limbs and abdominals).
General principles of treatment of superficial vein thrombophlebitis
These principles are truly general for both conservative and surgical treatment of this pathology. The main objectives of treatment
these patients are:
- Act as quickly as possible on the source of thrombosis and inflammation to prevent its further spread.
- Try to prevent the transition of the thrombotic process to the deep venous system, which significantly increases the risk of developing pulmonary embolism.
- Treatment should be a reliable method of preventing recurrent thrombosis of the venous system.
- The treatment method should not be strictly fixed, since it is determined primarily by the nature of the changes occurring in the limb in one direction or another. That is, it is quite logical to switch or complement one treatment method with another.
Of course, conservative treatment
indicated for the absolute majority of patients with “low” superficial thrombophlebitis of the saphenous veins.
Once again, it should be emphasized that reasonable physical activity of the patient improves the function of the muscle pump, which is the main determinant in ensuring venous outflow in the inferior vena cava system.
The use of external compression (elastic bandage, stockings, tights) in the acute phase of inflammation can cause some discomfort, so this issue should be resolved strictly individually.
The issue of using antibiotics in this category of patients is quite controversial. The doctor must remember the possible complications of this therapy (allergic reactions, intolerance, provocation of blood hypercoagulation). Also, the question of the advisability of using anticoagulants (especially direct action) in this group of patients is far from clear.
The doctor must remember that the use of heparin after 3-5 days can cause thrombocytopenia in the patient, and a decrease in the platelet count by more than 30% requires discontinuation of heparin therapy. That is, difficulties arise in controlling hemostasis, especially in an outpatient setting. Therefore, it is more appropriate to use low molecular weight heparins (dalteparin, nadroparin, enoxaparin), since they extremely rarely cause the development of thrombocytopenia and do not require such careful monitoring of the coagulation system. The positive thing is that these drugs can be administered to the patient once a day. A course of treatment requires 10 injections, and then the patient is transferred to indirect anticoagulants.
In recent years, ointment forms of heparin (Lioton-gel, Hepatrombin) have appeared for the treatment of these patients. Their main advantage is fairly high doses of heparin, which are delivered directly to the site of thrombosis and inflammation.
Of particular note is the targeted effect on the zone of thrombophlebitic changes of the drug Gepatrombin
(“Hemofarm” – Yugoslavia), produced in the form of ointment and gel.
Unlike Lyoton, it contains 2 times less heparin, but additional components - allantoin and dexpanthenol, which are part of the ointment and gel "Gepatrombin", as well as pine essential oils, which are part of the gel, have a pronounced anti-inflammatory effect, reduce skin itching and local pain in the area of thrombophlebitis. That is, they help relieve the main symptoms of thrombophlebitis. The drug Gepatrombin has a strong antithrombotic effect.
It is used topically by applying a layer of ointment to the affected areas 1-3 times a day. If there is an ulcerative surface, the ointment is applied in the form of a ring up to 4 cm wide around the perimeter of the ulcer. The good tolerability of the drug and the versatility of its effect on the pathological focus puts this medicine at the forefront in the treatment of patients with thrombophlebitis both on an outpatient basis and during treatment in hospitals. Hepatrombin can be used in a complex of conservative treatment or as a means aimed at relieving inflammation of the venous nodes after the Troyanov-Trendelenburg operation, as a method of preparation for the second stage of the operation.
The complex of conservative treatment of patients should include non-steroidal anti-inflammatory drugs
, which also have an analgesic effect. But the clinician must remember to exercise extreme caution when prescribing these drugs to patients with diseases of the gastrointestinal tract (gastritis, peptic ulcer) and kidneys.
Phlebotonics, already well known to doctors and patients, have proven themselves well in the treatment of this pathology.
(rutoside, troxerutin, diosmin, gingko biloba and others) and
disaggregants
(acetylsalicylic acid, pentoxifylline). In severe cases with extensive phlebitis, intravenous transfusions of rheopolyglucin 400–800 ml IV for 3 to 7 days are indicated, taking into account the cardiac status of the patient due to the danger of hypervolemia and the threat of developing pulmonary edema.
Systemic enzyme therapy has limited use in practice due to the high cost of the drug and a very long course of treatment (from 3 to 6 months).
Surgery
The main indication for surgical treatment of thrombophlebitis, as previously indicated, is the growth of a blood clot along the great saphenous vein above the middle third of the thigh or the presence of a blood clot in the lumen of the common femoral or external iliac vein, which is confirmed by phlebography or duplex scanning. Fortunately, the latter complication does not occur so often, in only 5% of patients with ascending thrombophlebitis (I.I. Zatevakhin et al., 2003). Although individual reports indicate a significant frequency of this complication, reaching even 17% in this group of patients (N.G. Khorev et al., 2003).
Methods of anesthesia - different options are possible: local, conduction, epidural anesthesia, intravenous, intubation anesthesia.
The position of the patient on the operating table is of certain importance - the foot end of the table should be lowered.
The generally accepted operation for ascending thrombophlebitis of the great saphenous vein is the Troyanov–Trendelenburg operation.
.
The surgical approach used by most surgeons is quite typical - an oblique incision below the inguinal fold according to Chervyakov or the inguinal fold itself. But at the same time, it is important to take into account the main clinical point: if there are instrumental data or clinical signs of a thrombus moving into the lumen of the common femoral vein, then it is more advisable to use a vertical incision that provides control over the thrombosed great saphenous vein and the trunk of the common femoral vein, when it is sometimes necessary to clamp it moment of thrombectomy.
Some technical features of the operation:
1. Mandatory isolation, intersection and ligation of the trunk of the great saphenous vein in the area of its mouth.
2. When opening the lumen of the great saphenous vein and detecting a thrombus in it that extends beyond the level of the ostial valve, the patient must hold his breath at the height of inspiration during surgery under local anesthesia (or this is done by an anesthesiologist for other types of anesthesia).
3. If the thrombus “does not form on its own,” then a balloon catheter is carefully inserted through the saphenofemoral anastomosis at the height of inspiration and thrombectomy is performed. Retrograde blood flow from the iliac vein and antegrade blood flow from the superficial femoral vein are checked.
4. The stump of the great saphenous vein must be sutured and ligated; it must be short, since a stump that is too long is an “incubator” for the occurrence of thrombosis, which creates a threat of the development of pulmonary embolism.
In order to discuss options for this routine operation, it should be noted that during the Troyanov-Trendelenburg operation, some surgeons suggest performing thrombectomy from the great saphenous vein and then injecting a sclerosant into it. The expediency of such manipulation is questionable.
The second stage of the operation - removal of thrombosed varicose nodes and trunks is carried out according to individual indications in a period of 5-6 days to 2-3 months as local inflammation is relieved, in order to avoid suppuration of wounds in the postoperative period, especially with trophic skin disorders.
When performing the second stage of the operation, the surgeon must ligate the perforating veins after preliminary thrombectomy, which improves the healing process.
All conglomerates of varicose nodes must be removed to avoid the further development of severe trophic disorders.
A very wide range of general surgeons and angiosurgeons are involved in the surgical treatment of this group of patients.
The apparent simplicity of treatment sometimes leads to tactical and technical errors. Therefore, this topic is almost constantly present at scientific conferences. Literature:
1. Zatevakhin I.I. with co-authors. “Angiology and Vascular Surgery” No. 3 (supplement) 2003, pp. 111–113.
2. Kabirov A.V. with co-authors. “Angiology and Vascular Surgery” No. 3 supplement 2003, pp. 127–128.
3. Kletskin A.E. with co-authors. “Angiology and Vascular Surgery” No. 3 (supplement) 2003, pp. 161–162.
4. Kotelnikov A.S. with co-authors. “Angiology and Vascular Surgery” No. 3 (supplement) 2003, pp. 168–169.
5. Revskoy A.K. “Acute thrombophlebitis of the lower extremities” M. Medicine 1976
6. Savelyev V.S. "Phlebology" 2001
7. Khorev N.G. “Angiology and Vascular Surgery” No. 3 (supplement) 2003, pp. 332–334.
Treatment Options
The doctor prescribes treatment based on the form and stage of phlebitis. It may have the following character:
- Medication. These can be drugs aimed at relieving inflammation, venoprotectors, anticoagulants, antibiotics. Topical medications may also be prescribed.
- Physiotherapeutic. For phlebitis of the lower extremities, a course of physiotherapeutic procedures may be prescribed to eliminate the signs of the disease remaining after the main treatment.
- Surgical. If complications develop and the disease does not respond to other treatment methods, the doctor performs surgery.
After eliminating the acute attack, the patient is recommended to use compression stockings.
Treatment of phlebitis
The first step to recovery is diagnosing the disease. Diagnosis is carried out by a phlebologist during a personal conversation with the patient and examination of the affected veins. Then the doctor prescribes a set of examinations to recognize the type of phlebitis and formulate a treatment strategy suitable for the patient.
A set of examinations may consist of different procedures. And it is compiled depending on the condition of the patient’s blood vessels and his overall health. For example, general and biochemical blood tests, blood coagulogram, ultrasound of blood vessels, MRI of the affected limb.
The second step of treatment depends on the form of the disease. Treatment of phlebitis of the superficial veins is carried out on an outpatient basis. Severe stages requiring surgery are treated with hospitalization. In this case, the patient spends 24 hours in the Vascular Center: 2 hours before the operation to prepare, during the operation and time for observation after the operation.
Complex forms are treated surgically. The following types of surgical intervention are used:
- crossectomy - ligation and removal of a vein;
- thrombus extraction - removal of blood clots;
- thrombolysis therapy - restoration of blood flow in the vessel due to the dissolution of the blood clot;
- installation of a vena cava filter - a device for catching blood clots.
Mild forms are treated with medication. The patient is prescribed:
- antibacterial drugs (for infectious phlebitis);
- anti-inflammatory drugs;
- ointments, gels with heparin;
- drugs to improve blood microcirculation:
- disaggregant - prevent the formation of blood clots;
- antihistamines, if the patient is allergic to drugs;
- glucocorticosteroids - prevent joint destruction.
The complex of drugs depends on the form of the disease. Treatment is also accompanied by wearing compression hosiery and mechanotherapy (the use of special devices and simulators to increase the functionality of the patient’s limbs).
Prevention
In order to prevent the development of phlebitis, it is recommended to adhere to the following recommendations and rules:
- exercise regularly and lead an active lifestyle;
- treat infections and inflammations correctly and promptly;
- Treat varicose veins promptly;
- it is advisable to avoid smoking;
- see your doctor regularly, especially if you are predisposed to venous diseases;
- eat properly and variedly so that the vascular system receives a sufficient amount of nutrients;
- control your weight;
- drink enough water per day;
- If you have to sit for a long time, do a warm-up every 2 hours.
The main causes of phlebitis
The development of the disease can be triggered by factors:
- phlebeurysm;
- infections, purulent wounds;
- burns, chemical burns, abscesses;
- damage to veins due to injuries, bruises;
- disruption of lymph flow in the tissues of the legs;
- malignant tumors, tuberculosis;
- prolonged immobility;
- complications after childbirth;
- insertion of a catheter into the vessels;
- mechanical damage to blood vessels (intravenous injection, infusion or blood sampling).
Causes of post-injection phlebitis
Sometimes phlebitis occurs after intravenous injections, insertion of a catheter independently and, at the same time, due to failure to maintain the proper level of hygiene. As a result, a spasm occurs, a narrowing of the vessel, and an infection causes inflammation of the vein (post-injection phlebitis).
The first symptoms of post-injection phlebitis appear 2-3 hours after the procedure: body temperature rises, the injection site hurts and thickens. Redness, bruising and swelling appear.
Thrombophlebitis treatment
I have accumulated vast experience in treating patients with acute thrombophlebitis at various stages of development of this formidable complication.
Thrombophlebitis laser treatment
Even in the most advanced cases, I try to use innovative techniques in the treatment of developed thrombophlebitis. Modern minimally invasive procedures of radiofrequency obliteration (RFO) and endovenous laser coagulation (EVLC) have proven themselves to be the best in the treatment of thrombophlebitis over recent years.
Video about how we remove blood clots from superficial veins in the legs without incisions in our center.
We successfully use these methods at the Moscow City Phlebological Center in the development of thrombophlebitis. Today, the world of modern phlebology is changing rapidly, new technologies are appearing, innovations are replacing each other.
Thrombophlebitis of the veins of the lower extremities. Causes and symptoms of thrombophlebitis
What are patients with varicose veins so afraid of when they come to see a phlebologist? Of course, the appearance of blood clots. Everyone knows that varicose veins themselves are not so terrible as their complications. One of the most common complications is thrombophlebitis (thrombosis) of the superficial veins of the lower extremities. Among phlebologists, it is also commonly called acute varicothrombophlebitis or ascending thrombophlebitis, thereby emphasizing the essence of the process that occurs in the lumen of varicose nodes of the superficial veins of the lower extremities.
Causes
For thrombophlebitis to occur, one or more of three factors must be present (the so-called Virchow triad):
- Damage to the vein wall (can be either mechanical, due to injury, or chemical - a burn from the administration of concentrated drugs, narcotic substances)
- Violation of the rheological properties of blood (increased coagulability, viscosity, etc.). This happens with dehydration, certain diseases, hormonal, and genetic disorders.
- Slowing of blood flow in the vein (when the vein is compressed, movement is limited (for example, when wearing a plaster cast)).
Under the influence of one or several factors, a blood clot forms in the lumen of the vessel and inflammation of its wall occurs. Example: with a serious leg injury, all three factors are present - mechanical damage (tears in the vein wall due to an impact), increased coagulability (due to blood loss), slowdown of blood flow (tissue swelling, plaster application).
Usually, with thrombophlebitis of the superficial veins, one vein is affected; inflammation can also spread to its tributaries. Migrating thrombophlebitis is known - with it, sequential inflammation of several veins occurs in different parts of the limbs. Such thrombophlebitis requires additional diagnostics to exclude oncological processes or genetic coagulation disorders.