Humane cartridges
The story began with the fact that on June 18 (5), 1904, he boarded the Trans-Siberian Express with an unfamiliar girl, and they emerged from the carriage as husband and wife. Such cases occur from time to time on the longest road in Russia. Here's one of the first.
Korotkov was born into a middle-class merchant family. His parents paid for his studies at the university and supported him while he operated free of charge in the clinics of Bobrov and Fedorov, gaining valuable experience. Merchants, whose heirs left business for various professions, usually had an agreement with their children: “Son, study as much as you see fit. But if you start a family, you will provide for it yourself.”
And then the time suddenly came, and when Korotkov went to war.
He was preparing a dissertation on traumatic aneurysm. When an artery is damaged, blood flows out, pushing the tissue apart so that a pulsating lake of blood is formed. A rupture of the aneurysm wall leads to fatal internal bleeding.
In battles with the Japanese, such injuries often occurred. Russian doctors called the cartridges of the enemy Arisaka 6.5 mm rifle “humane.” The reason for humanism was the frailty of the Japanese infantryman, who could not withstand the strong recoil from a large-caliber bullet. Thin Japanese bullets in a durable cupronickel shell deformed little when hit. On average, the wounds they inflicted healed faster. But the small-caliber bullet tumbled in the soft tissues, bruising blood vessels and causing aneurysms.
Korotkov had already seen such wounds in Blagoveshchensk, when Chinese bandits obtained Japanese weapons during the Boxer Rebellion of 1900. At the first news of the war with Japan, he volunteered for the sanitary detachment of the St. George community of sisters of mercy of the Red Cross. He approached the matter thoroughly. I took with me all the literature on aneurysms, starting with the works of Pirogov, and new instruments from the Military Medical Academy.
Modern ABPM systems
Modern 24-hour blood pressure monitoring systems:
real opportunities in clinical practice.
Akselrod A.S., Head of the Department of Functional Diagnostics
Clinics of Cardiology MMA named after. THEM. Sechenov
Today, 24-hour blood pressure recorders (monitors) are becoming increasingly common in functional diagnostic departments of cardiology hospitals and clinics. However, this study is less in demand than Holter ECG monitoring. This situation is due to the fact that often practicing doctors consider it unnecessary to use an expensive monitor for a patient who can independently measure blood pressure throughout the day with the required frequency. At the same time, the doctor forgets that keeping a BP diary while the patient is awake does not allow monitoring nighttime BP values. In addition, automatic blood pressure monitors allow you to obtain an objective picture of blood pressure dynamics during the day, excluding aggravation on the part of the patient and underdiagnosis on the part of the doctor.
Main characteristics of blood pressure recorders (monitors)
Modern blood pressure recorders are small in size and weight (200-300g). Of course, any manufacturer strives for a progressive reduction in the size and weight of the monitor in each subsequent generation.
To carry the recorder, special reusable (or disposable) bags with adjustable straps are used. Unlike a 24-hour ECG recorder, it is impossible to make a 24-hour blood pressure monitor practically invisible to others due to the shoulder cuff and the sound of the compressor operating during the next measurement.
The frequency of blood pressure measurements during monitoring may vary. One of the most common is a program with the following frequency: during the day - once every 20 minutes, at night - once every 30 minutes. However, there may be a need for more frequent (once every 15 minutes) or, on the contrary, less frequent (once every 30 or 40 minutes) measurements. Most modern recorders have the ability to save several standard measurement programs with different frequencies of measurements at different periods of the day.
Blood pressure is recorded over a 24-hour period, hence the name of the study “24-hour blood pressure monitoring” (ABPM). During this time interval, you can see the change in periods of sleep and wakefulness and, therefore, have the most complete understanding of the dynamics of blood pressure in the patient. With a shorter registration period, distortion of the indicators will inevitably occur (primarily the average blood pressure values during the day and night hours).
Figure 1 shows a 24-hour blood pressure recorder BR-102 plus from Schiller AG, Switzerland.
Rice.
1. 24-hour blood pressure recorder BR -102 plus from S with Hiller AG , Switzerland.
Measurement methods for ABPM: advantages and disadvantages.
Systems for ABPM use the following options for measuring blood pressure:
oscillometric method;
· Korotkoff method (auscultatory or acoustic);
· combination of both methods.
The different physical principles underlying these methods may result in significant differences in blood pressure measurements. That is why the interpretation of the results obtained on blood pressure monitors with different measurement methods in the same patient over time is difficult and is not correct. The main differences between the methods are presented in Table 1.
Tab. 1. The main differences in methods for measuring blood pressure when performing ABPM.
| Method Differences | Auscultatory (Korotkoff method) | Oscillometric |
| General acceptance of the method | is the “gold standard” for blood pressure measurement | Instruments from different companies have measurement algorithms with some differences |
| Differences between the values of the blood pressure monitor and the values obtained by traditional measurements with a tonometer | no significant differences | may vary greatly |
| Number of successful measurements during active movement | up to 85-95% | no more than 15-25% |
| Study of the individual characteristics of the method | good | bad |
| Possibility of use in conditions of external noise | cannot be used | can be used if the noise is not accompanied by strong vibration |
| Possibility of use in persons with deaf tones | up to 5-10% of patients | in almost 100% of patients |
| Sensitivity to proper microphone placement and cuff movements | high | low, it is possible to measure blood pressure through thin tissue |
From the table presented, it is clear that the blood pressure recorders that have the greatest sensitivity and reproducibility are monitors with a combined method of blood pressure recording (i.e., using both the auscultatory Korotkoff method and the oscillometric method).
First of all, the need for a combined measurement method is dictated by the lifestyle characteristics of patients. Currently, ABPM is very often in demand by actively working people in the real conditions of their working hours. It is ambulatory monitoring in such patients that is most informative, therefore, successful measurement of blood pressure during heavy traffic and/or in a noisy room is absolutely necessary.
Software Features
After completing blood pressure measurements at a given frequency, the information obtained is transferred from the monitor to a personal computer with installed software. Regardless of the manufacturer, the stage of data transfer and analysis occurs in fundamentally the same way for all registrars. The duration of this period usually takes 1-3 minutes.
Depending on the software manufacturer, the “icons” and program options will be called and look, of course, differently.
However, almost all programs have the same principles.
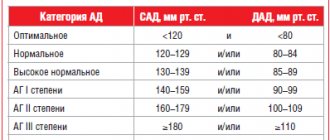
Boundaries of systolic and diastolic pressure
in different (daytime and nighttime) periods and the resulting dynamics of blood pressure and heart rate can be compared on the corresponding graphs (Figure 2). Such graphs are usually called trends.
Rice. 2. Boundaries, periods and trends in the dynamics of systolic (SBP, red), diastolic (DBP, green) and average (MAP, blue) pressure; trend of heart rate dynamics.
Moreover, most programs allow you to set and change the maximum permissible range (limits) of values for normal heart rate, as well as normal values of systolic (SBP), diastolic (DBP) and mean pressure (MAP) during the day and night. In addition, the software must have the ability to indicate (if necessary, correct) the beginning of the day and night periods. The need for such a feature is due to the fact that, for a number of reasons, the recorder can be installed for a certain period of time (for example, only for night measurements).
Histograms
the obtained blood pressure values are also very clear for assessing the predominance of absolute and/or relative blood pressure values (Figure 3). The colored vertical line on each histogram is the maximum permissible value of the corresponding indicator (SBP, DBP, MAP, HR). The location of most bar graphs to the right of the vertical indicates a tendency toward arterial hypertension, while to the left indicates a predominance of normal or low blood pressure values. It is the “attachment” of histograms to the vertical that indicates the degree of severity of the trend. If the bar graphs of SBP, DBP or MAP are not in contact with the vertical and the histogram is strongly shifted to the left or right of it, we can speak of a pronounced tendency towards arterial hypo- or hypertension, respectively.
Rice. 3. Histograms of absolute values of SBP, DBP, MAP and HR for the day, night and day.
Some manufacturers, instead of bar charts, present pie charts that show the distribution of low, normal, moderately and significantly increased values in absolute values and/or % of the total number of measurements.
Measurement data
must be submitted to a doctor for editing, as they are primary material. With a combined method of measuring blood pressure, the program must provide the doctor with information about the method for obtaining each measurement. By comparing the measurement time and the patient’s activity according to the diary, the doctor can also assess the adequacy of the obtained BP values with actual physical activity.
Based on all the information, the doctor is able to assess the likelihood of an artifact and exclude questionable results from the analysis.
Fig.4 Measurement data
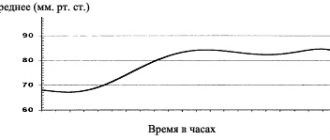
Averaging data
Most manufacturing companies provide an additional trend (Figure 5). These data are of great importance for patients with rare moderate or significant elevations in blood pressure. By analyzing the dynamics of average values for each hour, the doctor can more reliably assess the dynamics of blood pressure during the day. Therefore, in controversial cases, it is the dynamics of average values that makes it possible to compare the results of several successive ABPM against the background of antihypertensive therapy and evaluate its effectiveness.
Fig.5. Averaging data
A pivot table (report) is very convenient.
with summary information in the form of absolute values and various trends. Based on such a summary table, it is convenient for the doctor to formulate a conclusion (Figure 6) and select fragments for a general printout (Figure 7).
Fig.6. Formulating a conclusion based on the summary table.
The choice of samples for printing can be made at the discretion of the physician. Of course, the printout that is handed to the patient cannot contain only a title page with a conclusion. At the same time, you should not select all software capabilities for printing in a patient with a normal blood pressure profile.
Fig.7. Formation of samples for printing
Main indicators of the daily blood pressure profile.
At present, a unified scheme for analyzing ABPM data has not yet been developed, and therefore there are differences in the set of parameters in the software of different manufacturers.
Among the indicators of the daily blood pressure profile, standard ones
and
additional
indicators.
To standard indicators
ABPM include:
· average values of systolic, diastolic, average, pulse blood pressure and heart rate for 24 hours, day, night;
· hourly average values of blood pressure and heart rate;
· maximum and minimum values of blood pressure and heart rate for different periods of the day;
daily index (DI, degree of blood pressure reduction at night);
· variability of systolic, diastolic, mean and pulse blood pressure and heart rate;
· indicators of “pressure load”: measurement index, hypertension time index (TI), hypertension area index (AI).
To additional indicators
ABPM include:
· hypotension indices (IIH, area of hypotension);
· characteristics of blood pressure dynamics in the morning (magnitude and speed of the morning rise in blood pressure, morning index).
Of course, not all of the above indicators should be automatically determined by the software. In most cases, the most informative in practical work (selection of antihypertensive therapy) are all average values (including hourly values), all maximum and minimum values of blood pressure and heart rate, daily index and measurement index. The remaining indicators can be calculated by a doctor if necessary and, of course, are of great interest for research work.
Of course, today there are still a large number of blood pressure recorders from various manufacturers. Having decided on the characteristics of “his” patient flow (elderly sedentary patients in a hospital or young active patients in an outpatient setting), the doctor selects equipment for ABPM. The only advice we allow ourselves to give is this: the high degree of freedom of the software determines the ability to work with a wide variety of patients. The greater the possibilities available in the presented program, the higher the likelihood of success of the medical analysis, comfort for the patient and the lower the risk of medical error.
Moscow, 07/16/2009
Elena the beautiful
All this flew out of his head when, while boarding the train, among his nurses he saw Elena Alekseevna. Korotkov was handsome, sang well, and charmed girls, drawing their portraits with pencils or paints. Painting is an excellent reason to spend several hours with a lady in a confidential conversation. During such activities, Korotkov forgot that he had not notified the head of the academy about his departure. Only on the Chinese border, from the Manchuria station, did he send a telegram to St. Petersburg with a request to postpone the defense of his dissertation until his return from the war.
From that day on, Elena Alekseevna was with him inseparably. Near Liaoyang, they jumped together on the move from one carriage with the wounded to another, because the design of such carriages did not provide for transitions. In Harbin we got wet together for a whole month under a yellow downpour. And they operated together, transferring from the Red Cross infirmary to the consolidated military hospital No. 1 with a loss of pay. There, along the entire front, wounded with suspected aneurysm were collected for Korotkov.
Riva-Rocci pear
In those days, this bloody tumor - some the size of a nut, some the size of a fist - was not always able to be distinguished from an abscess. Following a recommendation read from Pirogov, Korotkov began to listen to aneurysms with a phonendoscope: even if the pulsation in them is imperceptible, the flow of blood inside creates some noise. Korotkov personally operated on 35 of these wounded: he ligated the arteries above and below the site of injury, usually removing the aneurysm sac.
Not all patients tolerated the operation well. For most, blood circulation was restored instantly: blood flowed through the collaterals that surround the artery, like lateral branches - a large river. Such bypasses help out with an aneurysm. But just as not all rivers have second channels, so collaterals are not developed everywhere in the human body. How can their presence be determined before surgery? How to predict whether the ligation of the artery will end successfully, or whether the lack of blood supply will cause gangrene, so is it better to amputate immediately?
Korotkov began to measure blood pressure below the wound - if the collaterals allow enough blood to pass through, it should reach a value that is sufficient to supply the limb. It was interesting, by the way, what value it was: no one knew it. A tonometer was used, which was invented by the Italian pulmonologist Scipione Riva-Rocci in 1896. Riva-Rocci made a cuff from a piece of bicycle tire that tightly enclosed the limb. They used a blower to pump air into the tire, squeezing the artery. Then the air was slowly released through the tap, and the pressure in the tire, at which blood began to pass under the cuff and the pulse was felt, was considered equal to the maximum (that is, upper, systolic) blood pressure. They didn’t know how to measure lower pressure at all.
Korotkov extended the Riva-Rocci cuff so that it could also cover the thigh - when wounded in the leg. He thought that the pressure necessary for normalization should reach at least 75 millimeters of mercury versus 120 in a healthy limb. It turned out that blood supply is restored even at 30, and in the fingers – at only a few millimeters. This was established on December 24, 1904, by experience on a patient whose gangrene had lost all fingers except the little finger. And this meant that the pressure was not zero, even if the pulse was not noticeable.
Revolution of Nikolai Korotkov. How was the method of measuring blood pressure invented?
Failed merchant
Any invention has its own author, its own history, sometimes not a simple one. But how quickly a person gets used to the fruits of any discovery and, having started using them at the everyday level, simply takes them for granted. No longer remembering the name of the discoverer.
Russian doctor Nikolai Korotkov. I wonder which of today's medical students will quickly, offhand, remember what he is famous for? However, in case of a hitch, you can ask a leading question: who came up with the method for measuring blood pressure?
A MERCHANT'S SON, NIKOLAI KOROTKOV REFUSED TO FOLLOW IN THE FOOTSTEPS OF HIS FATHER, ALREADY IN HIS YOUTH HE FIRST DECIDED TO DEVOTE HIMSELF TO MEDICINE
Yes, the history of the tonometer is closely connected with this person. The merchant's son, Nikolai Korotkov, refused to follow in his father's footsteps, having firmly decided in his youth to devote himself to medicine. After studying for three semesters at the medical faculty of Kharkov University, where he easily entered, Nikolai transferred to Moscow University - here, he believes, there are more opportunities for gaining knowledge.
In 1898, Korotkov was awarded the diploma of “doctor with honors” and, at the same time, he successfully passed the test for the title of district doctor. After an internship at a surgical clinic, as a volunteer, as part of one of the Red Cross units, he went to China, where at that time Russian troops took part in hostilities. For his services he was awarded the Order of St. Anne, third degree.
Read the material on the topic: The triumph of love and creation. How was the Red Cross created?
"Tuner" of the human body
Korotkov once again had the opportunity to play the role of a military surgeon: he also participated in the Russian-Japanese War. The doctor operated on the wounded a lot, including dealing with damage to large blood vessels. In those days, to save such soldiers, the limb was simply clamped, trying to prevent critical blood loss. After which the arm or leg had to be amputated to avoid the development of gangrene.
Korotkov persistently looked for ways to do without amputation. Of course, he knew one of the classical medical methods - auscultation, that is, listening to damaged vessels. And he listened and listened, like an experienced tuner listens to an out-of-tune piano. But he just had to hear that true, without falsehood, note.
About “upper” and “lower” blood pressure
Of course, it was not only the Russian surgeon Nikolai Korotkov who tried to solve this problem. The first prototype of a device for measuring blood pressure was proposed by the Turin physician Scipione Riva-Rocci back in 1896. It was then that a special compression cuff and a pressure gauge connected to it appeared.
However, the device was far from perfect. First of all, it was very bulky and inconvenient to use. But the main drawback of the device proposed by the Italian doctor was that it could only measure systolic blood pressure.
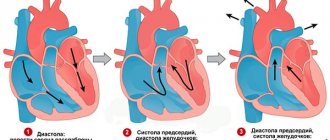
A little clarification. Today, when almost every family has blood pressure monitors, you often hear: “What is your upper pressure? What about the bottom?” What does this mean?
“Upper” - that same systolic - gives a characteristic of the work of the heart, shows the pressure at the moment of greatest contraction of the main organ of our body, when the heart “throws out” blood. The average norm for this indicator is 120-140 millimeters of mercury.
But there is another, no less important indicator - diastolic (“lower”) pressure; it gives the doctor an idea of the condition of the blood vessels. An indicator of 70-90 mmHg will appear. Art. - that means everything is close to normal. In addition, this parameter can be used to judge the condition of such an important organ as the kidneys.
Read the material on the topic: Hypertension? Looking for reasons
It was precisely this “lower” limit that the Italian therapist failed to reach. This discovery was to be made by the Russian innovator doctor.
The price of a word
Nikolai Korotkov’s passion for vascular surgery led to the fact that he decided to devote his doctoral dissertation to this topic. And then the unexpected happened.
November 1905, Imperial Military Medical Academy. Scientific and medical luminaries are once again discussing a long-standing problem: how to measure blood pressure. Korotkov gives his report. It is based on the result of his many listening to the damaged blood vessels of wounded soldiers.
THE KOROTKOV METHOD IS STILL THE ONLY NON-INVASIVE METHOD FOR MEASURING BLOOD PRESSURE
Nikolai Sergeevich offers his own, original, method, he calls it “a sound method for determining blood pressure in people.” And - here it is, triumph. The Korotkov method is still the only non-invasive (that is, without any punctures or “penetration” into the body) method of measuring blood pressure.
What is most surprising is that Korotkov’s historical report consisted of... only 281 words.
Remember this name
And finally, a few words about the personal qualities of this person. Neither the world-class discovery nor the defense of his doctorate had any impact on his character. Korotkov never looked for easy ways for himself. He treated workers at gold mines in distant Siberian Bodaibo, and healed both during the First World War and after it. For many years he worked for free, being an “unpaid assistant surgeon” at the Moscow Surgical Clinic. He did not leave medical practice even when he himself fell ill with pulmonary tuberculosis. Died at 46 years old.
Nikolai Sergeevich Korotkov. When you pick up a tonometer - and, alas, we often have to do this - remember this glorious name. Really, such a person deserves to be remembered.
Text: Igor Chichinov
Other materials on topics:
Selling everything means saving millions. How was insulin discovered?
For the sake of the people. The tenacity of Dr. Ilizarov
Don't change yourself... The human feat of Vladimir Demikhov
Experiments on my wife
Having become accustomed to listening to blood vessels with a phonendoscope during examination, Korotkov also did this when measuring pressure. At the beginning of 1905, he discovered that when the cuff was loosened, at a certain moment, sounds similar to the muffled blows of a tambourine were heard. Apparently, a compressed vessel emits them as soon as the first drops of blood seep through it, when the pulse is still imperceptible. If you bleed the air further, the sounds increase and then disappear. Korotkov guessed that at this moment the pressure inside the cuff drops below the minimum (diastolic), so that the vessel is no longer compressed. The first experiments in measuring upper and lower pressure were carried out “on a healthy person,” as Korotkov wrote, without specifying that it was Elena Alekseevna.
By that time she was expecting a child. On April 14 (1), the Korotkovs resigned and left the war for St. Petersburg. Nikolai Sergeevich presented his observations at Fedorov’s clinic. The ability to predict collateral strength using a tonometer has greatly impressed surgeons.
But when on November 21 (8), Korotkov reported at a scientific meeting of therapists about a new, much more accurate, method of measuring pressure, he was badly bitten.
The main complaint was that the author of the method does not know the nature of his sounds. What if the heart produces them, and then in case of heart defects, for example, they are distorted? The idea of finding out the lower pressure seemed completely incredible. No one has ever done this before, even abroad.
Advantages of the Korotkoff method for blood pressure monitoring
Download Slideshow
Author: Tikhonenko V. M.
PDF file
For a hundred years now, the acoustic method of measuring blood pressure (BP), proposed by our compatriot N.S. Korotkov, has been the only officially approved method for non-invasive determination of blood pressure. The Korotkoff method, which we all constantly use in everyday practice, certainly does not need any protection. However, in recent years, opinions have increasingly begun to be expressed that when monitoring blood pressure, this method can be dispensed with. Almost half of the monitors produced for 24-hour blood pressure monitoring (ABPM) no longer use the acoustic method, making measurements using oscillometry. In this work, therefore, we tried to understand the advantages and limitations of both methods.
The most obvious advantage of the oscillometric method is the absence of a microphone - only the application of a cuff is sufficient for measurement, whereas to obtain a result using the Korotkoff method, the microphone must be correctly applied and not dislocated during the observation period. This is an important advantage when self-monitoring blood pressure by the patient, since the likelihood of the patient placing the microphone incorrectly is very high, which will lead to the impossibility of measuring or obtaining incorrect numbers. For example, if the microphone is not pressed against the artery by the cuff, the amplitude of the tones will be very low and the measurement will be unsuccessful. If the microphone is located under the upper part of the cuff, then a sharp increase in systolic blood pressure is possible due to the “tapping” of the pulse wave, even with the cuff compressed (Fig. 1).
With professional testing, such as blood pressure monitoring, when the installation is performed by specially trained medical personnel, the significance of this advantage is negated. An experienced nurse or doctor correctly positions the microphone, and the possibility of its dislocation relative to the artery is eliminated by a separate installation from the cuff - “gluing” it to the skin.
The next frequently mentioned “disadvantage” of the Korotkoff method is the widespread prevalence of individual tonal characteristics, which can result in incorrect blood pressure numbers. For example, with an “acoustic” failure, when the tones in the second phase are very low-amplitude and cannot be heard, systolic blood pressure may be underestimated. With the so-called “endless” Korotkoff sound, when sound phenomena in the vessel continue until very low pressure in the cuff, there is a high probability of underestimation of diastolic blood pressure (Fig. 2). In general, certain features of tones can be observed in 5-7% of patients, complicating the use of the method.
However, in our opinion, the fact that the individual characteristics of Korotkoff sounds are well known to doctors is more an advantage than a disadvantage of the method. Doctors are able to assess blood pressure in patients with special needs. For example, with an “endless” tone, an experienced doctor will usually determine diastolic blood pressure not by the fifth, but by the fourth phase of the tones - when they are sharply muffled. With oscillometry, special variants of pulsations also occur, but we do not know them well and do not know how to eliminate them. An example is the often observed “double-humped bell,” when the pulsation amplitude does not change monotonically, and an underestimation of systolic or overestimation of diastolic blood pressure is possible (Fig. 3). In our experience, certain features of the oscillogram are observed in every tenth patient, but, unfortunately, doctors do not know what can be done to avoid receiving incorrect blood pressure numbers in these cases.
Another limitation of the Korotkoff method is sensitivity to noise in the surrounding space. When there is pronounced noise, such as happens, for example, in a metro train, Korotkoff sounds “drown” in it and reliable measurement of blood pressure is impossible (Fig. 4). This property limits the use of the method for examining, for example, pilots, but in clinical practice this drawback is not significant - usually no more than 1-2% of measurements are rejected based on the presence of noise on the microphone. In addition, the significance of external noise is reduced when differential microphones are used.
The most significant limitation of the acoustic method for blood pressure monitoring is the presence of patients with muffled tones, when the tones are not audible or there is no confidence that all phases of the tones are audible. In such patients, blood pressure is either not determined using the Korotkoff method, or errors are possible - underestimation of systolic and overestimation of diastolic blood pressure. The number of such patients in the population when listening while awake at rest ranges from 2 to 5%. When monitored, this percentage may increase to 5-10% due to a decrease in amplitude during sleep at night. A decrease in the sonority of tones during sleep is observed in all patients, and in some of them it may be critical in terms of the accuracy of blood pressure measurements. Oscillometry has clear advantages here - such low-amplitude pulsations, from which it is impossible to reliably determine blood pressure, occur with a frequency of no more than 0.1% only in cases of severe obesity.
On the other hand, the oscillometric method also has disadvantages. When measured at rest, according to most studies, its accuracy is slightly lower than that of Korotkov. For example, when assigning a class according to the BHS90 or BHS93 protocol, Korotkoff monitors usually correspond to class A/A, while oscillometric monitors are often classified as B/A. This is understandable, since the “reference” blood pressure is usually taken to be the pressure measured by two experts using the Korotkov method. This drawback is not so significant, since devices are being improved and the accuracy of measuring blood pressure at rest is constantly increasing.
Much more significant is the low noise immunity of blood pressure measurements using the oscillometric method during the patient’s physical activity. With minimal movements of the arm, which occur even during quiet walking, pronounced fluctuations in pressure in the cuff occur, which mask the pulsations of the artery and make it impossible to measure by oscillometry (Fig. 5). As a result, when using only the oscillometric method, complete immobility of the patient during the measurement is necessary - otherwise the measurement will be rejected. During the daytime, during patient activity, measurements rejected by pressure pulsations predominate, while measurements by Korotkoff sounds are possible in most of these cases.
Thus, according to our data, when examining 60 patients while climbing stairs, it was possible to correctly measure blood pressure using the Korotkov method in 85% of cases, while the oscillometric method was able to determine blood pressure in only 8.3% of patients (p<0.05). According to A.N. Rogoza (1996), it was possible to successfully measure blood pressure during bicycle ergometry in 93% of cases when using the Korotkov method and in only 18% when using oscillometry. Thus, the oscillometric method does not allow assessing blood pressure during the patient’s free behavior. When using only this method, the diagnostic value of ABPM is significantly reduced, since the doctor sees only changes in pressure at rest, which is enough to detect nocturnal hypertension or “white coat syndrome”, but is clearly not enough to characterize the entire daily blood pressure profile. The features of the oscillometric and Korotkoff methods of measuring blood pressure during monitoring are summarized in table. 1.
Having considered the advantages and limitations of both methods, we can conclude that for ABPM monitors should be used that provide measurement using two methods. In patients with sonorous Korotkoff sounds, they will allow you to measure blood pressure during the patient’s activity and obtain a minimum number of defective measurements carried out with high accuracy using the acoustic method. In cases of muffled tones or when measuring in conditions of pronounced external noise, the device will measure blood pressure using an alternative oscillometric method and blood pressure figures will nevertheless be obtained. In measurements where there is no pressure interference and there are sonorous tones, a combination of the two methods, if the results match, will give the doctor additional confidence in the accuracy of the measurement.
Experiment on a dog
Korotkov wanted to answer with an experiment, but the stress of a year and a half took its toll. He fell ill. The same VMA therapists diagnosed tuberculosis of both lungs and forbade me to get out of bed. Having suffered an exacerbation in the hospital, it was necessary to immediately change the climate. And yet, with the last of his strength, Korotkov carried out his experiment. The dog's femoral artery was isolated from the heart with a clamp. A tube was inserted into the artery, through which a salt solution was injected under pressure close to natural (from time to time Korotkov removed the clamp and allowed blood to flow so that the dog did not lose a limb). When manipulating the tonometer, the artery cut off from the heart with saline made the same sounds. Korotkov believed that the reason was the collapse and unsticking of the vessel.
This is what he said at the new meeting on December 26 (13). Deep doubts were again voiced until the chairman took the floor. It was Mikhail Vladimirovich Yanovsky, the chief therapist of the Military Medical Academy, and in fact of the entire army. He had not yet seen Korotkov, since he was absent from the previous meeting. (Then Sechenov died, and Yanovsky went to the funeral).
The chairman began by saying that this is not a collapse, because such a sound requires air, but there is none in the vessels. But the heart has nothing to do with it either. The reason is a sound wave, which is caused by obstructed blood flow, turbulent flow [which was later confirmed]. As for the rest, the speaker is right, Yanovsky summed up: “... I must say that in your observations you have discovered a certain talent and wit. You easily noticed a fact that many researchers missed when dealing with this issue.” From that day forward, therapists began listening for Korotkoff sounds when measuring blood pressure. First at the Military Medical Academy, a year later in Poland, two years later in Germany, and after 10 years in America.
Korotkoff sounds
The Korotkovs had a son. To feed his family and save himself from consumption, Nikolai Sergeevich hired himself as a doctor in the gold mines. The healing air of the pine forests stopped the apical process. The wife and son spent the summer and autumn with the doctor, leaving the harsh Siberian winter for European Russia. In 1911, when it was time for her son Seryozha to prepare for exams at the gymnasium, Elena Alekseevna left the boy with his father for the winter so that he could coach him in mathematics and Russian speech. Korotkov then worked at the Andreevskaya hospital of the Lenzoloto trust, and became an involuntary witness to the notorious Lena execution. On April 17 (4), 1912, 250 striking workers were shot on the street, and the same number were wounded in the Korotkov hospital. He didn't sleep a wink for several days and turned gray, even though he had just turned 38.
Then two commissions arrived from the capital, with whom the doctor had to explain himself. One is Senate, the other is public, led by the still unknown lawyer Alexander Kerensky. Thus began the political career of the future head of the Provisional Government. And there is some kind of secret connected with him, because of which Korotkov’s name was hushed up until Stalin’s death.
From the point of view of the Soviet government, the doctor’s biography is impeccable. He ended his relationship with Lenzolot and returned to St. Petersburg. After the revolution, he did not go to the whites or abroad. He treated wounded Red Army soldiers. Under war communism, I was malnourished like everyone else. Due to exhaustion, tuberculosis returned, and in 1920 Nikolai Sergeevich died of pulmonary hemorrhage.
His son became a doctor, but a strange thing: at the medical institute he was taught to measure blood pressure, without saying a word that his father was the first to do this. After the war, when Soviet propaganda trumpeted that everything in the world was invented by the Russians and in general “Russia is the birthplace of elephants,” no one mentioned a man whose discovery is called “Korotkoff sounds” all over the world (native speakers of English pronounce this surname with an emphasis on the second syllable). Only during the “thaw” did Fedorov’s students remember the Russian surgeon, without whom there would not have been a modern tonometer.
What’s the matter, they were embarrassed to say. For some unknown reason, Elena Alekseevna, who lived to see the blockade, did not save a single photograph of her beloved husband. And his son, Sergei Nikolaevich, first saw a photo of his father only in 1970.
Mikhail Shifrin
Mikhail Shifrin