Asystole of the cardiac ventricles is a complete stop of the heart and, accordingly, cessation of its activity. It consists of ventricular fibrillation, asystole and electromechanical dissociation. The clinical picture of this pathology is very vivid, moreover, extremely dangerous, regardless of age and gender.
Symptoms of this type of disease are called clinical death; at this moment, loss of consciousness occurs, in which there is no pulse in the large arteries. Breathing becomes noisy and rare, the skin acquires a pale bluish color. In addition, a person who has lost consciousness may experience a convulsion; a couple of minutes after fainting, the reaction of the pupils to light is lost, while they are in a dilated state.
It is important to know! In order to save a person during ventricular asystole, it is necessary to immediately perform resuscitation procedures. If the victim has the above symptoms, you need to give him artificial respiration and perform chest compressions, and, of course, take him to a medical facility as quickly as possible.
Causes of the disease
Asystole can be a consequence of both cardiac pathologies and lesions of an extracardiac nature.
The disease necessarily affects the functioning of the sinus node, which is responsible for the heart rate. The main causes of cardiac disease include:
- cardiogenic shock;
- cardiac ischemia in the acute or chronic stage;
- cardiac thrombosis;
- necrosis of a significant area of the myocardium;
- cardiac tamponade, which occurs when the membranes of large vessels rupture;
- impaired functioning of artificial valves;
- aortic stenosis;
- hypertrophic changes observed in the myocardium;
- inflammation of the inner or muscular layer of the heart, etc.
Causes of asystole not related to heart disease:
- significant blood loss, which reduces the volume of its circulation through the vessels;
- decreased oxygen content in the blood with an increase in the amount of carbon dioxide;
- thrombus formation in the pulmonary arteries, which leads to blockage of their large branches;
- chest injuries, in which there is an accumulation of air in the pleural cavity;
- hypothermia for a long time;
- electric shock;
- overdose of certain types of drugs;
- severe stress, during which large amounts of adrenaline are released;
- shock of various nature.
Algorithm for providing assistance
Treatment of cardiac asystole according to approved clinical protocols involves carrying out resuscitation measures in the presence of signs of circulatory arrest. At the pre-hospital stage (before the arrival of the ambulance, which must be called by witnesses), it is necessary:
straightening and clearing the airways (unfasten the narrow collar, remove foreign objects from the oral cavity).- mouth-to-mouth breathing;
- indirect cardiac massage (at least 100 compressions per minute) - this method of artificial contraction of the myocardium contributes to minimal hemodynamic recovery. The effectiveness of the event is ensured by the activation of the nervous system and sinus node.
Emergency doctors use intravenous injections of adrenaline, which helps activate the autonomic nervous system and start cardiac activity.
In a hospital setting, the patient is treated for the resulting consequences of resuscitation (“post-resuscitation illness”) and the primary cause of circulatory arrest, which implies:
- adequate ventilation (using a machine or oxygen therapy);
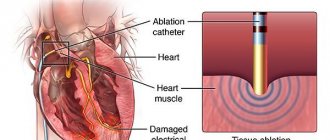
- surgical interventions for injuries;
- correction of metabolic processes;
- use of antidotes;
- administration of intravenous glucose solution;
- replacement therapy with blood products after significant loss and hypovolemia.
There are no traditional methods for treating or preventing asystole; cardiac arrest is one of the signs of death, which requires emergency resuscitation.
How does cardiac asystole appear on an ECG?
Cardiac asystole on the ECG is detected in the form of an almost straight line reflecting its electrical activity.
Characteristic signs of this condition also include abnormal atrial rhythm and the inability to count the frequency of their contractions when there are no ventricular contractions. In some cases, when the atria continue to contract for some time after the ventricles have stopped, atrial P waves can be detected on the cardiogram.
An auxiliary element for diagnosing asystole can be the arrhythmia preceding this condition. So, if it manifests itself in the form of early polytopic ventricular extrasystoles and ventricular tachycardia, then they will be followed by ventricular fibrillation and flutter, and increasing blockade usually indicates the approach of asystole.
| Passive | |
| Atrioventricular replacement nodal systole | Single nodal contractions after a long diastolic pause |
| Escape atrioventricular nodal rhythm | Frequency 40-60 per minute |
| Active | |
| Nodal (atrioventricular) extrasystole | Single premature nodal contractions |
| Non-paroxysmal nodal (atrioventricular) tachycardia | Frequency 60-150 per minute |
| Paroxysmal nodal (atrioventricular) tachycardia | Frequency 150-220 per minute |
ATRIOVENTRICULAR NODUAL RHYTHM
With atrioventricular rhythm, the heart contracts for a long period of time under the influence of passively activated impulses from the atrioventricular system with a frequency of 40-60 per minute. Impulses emanating from the atrioventricular system propagate upward, retrograde to the atria, and downward to the ventricles. Atrioventricular rhythm is defined as the presence of six or more successive escape nodal contractions.
Mechanism
Atrioventricular rhythm is the result of a passive replacement mechanism. It occurs when impulses from the sinoauricular node or other atrial ectopic impulses do not reach the atrioventricular system at a certain time. The automaticity of the atrioventricular system is included as a physiological mechanism for creating ventricular contractions in cases where other supraventricular impulses do not reach the atrioventricular system.
Atrioventricular rhythm begins:
1. With slow sinus impulses - sinus bradycardia and (or) sinus arrhythmia
2. When sinus impulses do not reach the atrioventricular node due to:
a) sinus node failure
b) sinoauricular blockade
c) atrioventricular block II or III degree 3. When ectopic atrial impulses during fibrillation, atrial flutter or tachycardia do not reach the atrioventricular node due to:
a) high degree or complete atrioventricular block
b) prolonged blockade at the exit (“exit block”) near the ectopic focus in the atrium
Most often, atrioventricular rhythm is observed with sinus bradycardia with sinus arrhythmia and with partial or complete atrioventricular block.
Hemodynamics.
Hemodynamic changes depend on the cardiac arrhythmia causing the atrioventricular rhythm, the ventricular rate and the underlying cardiac disease. When junctional rhythm occurs with sinus bradycardia, intermittent sinus node block, or short-term sinoauricular block, there is usually no hemodynamic disturbance. On the contrary, nodal rhythm during atrioventricular block, especially in the presence of atrial fibrillation, is accompanied by significant hemodynamic disturbances. The slower the ventricular contraction rate during junctional rhythm as a result of complete atrioventricular block, the more pronounced the hemodynamic disturbances. With a junctional rhythm with simultaneous contraction of the atria and ventricles, the value of atrial systole during filling of the ventricles disappears and the stroke volume decreases.
Etiology
The etiology of atrioventricular rhythm coincides with the etiology of the underlying arrhythmia that causes its appearance: sinus bradycardia, sinoauricular block, sinus node failure, atrioventricular block with or without atrial fibrillation.
There are three main etiological possibilities:
Vagotonia in healthy people, especially after irritation of the vagus nerve by pressing on the carotid sinus or eyeballs, with deep breathing
Drug effects and metabolic disorders - intoxication with digitalis drugs, strophanthin, quinidine, procainamide, morphine, reserpine, guanethidine, hyperkalemia, acidosis, hypoxia
Organic heart diseases - acute myocardial infarction, especially with its posterior-inferior localization and (or) atrial infarction, coronary disease with atherosclerotic myocardiosclerosis, hypertension, rheumatic heart defects, rheumatic carditis, myocarditis and cardiomyopathies, heart failure of various etiologies, shock, damage during heart surgery, after electrodefibrillation
In healthy people, we are most often talking about sinus bradycardia with the occurrence of single replacement systoles or short periods of replacement nodal rhythm. Elderly people with coronary artery disease most often have high-grade atrioventricular block with prolonged periods of junctional rhythm, or complete atrioventricular block with a constant junctional rhythm. In patients with atrial fibrillation, poisoning with digitalis drugs often causes high-grade atrioventricular block with the appearance of long periods of escape junctional rhythm. Junctional rhythm is often detected during the bradycardial phase of brady-tachycardial syndrome. In every case of unclear origin of the junctional rhythm, one should think about hyperkalemia and acidosis.
Clinical picture.
Healthy people with sinus bradycardia and a short junctional rhythm do not complain. Patients with prolonged junctional rhythm often have subjective symptoms, which depend on the severity of the underlying disease and the degree of decrease in cardiac activity. With a junctional rhythm with a fresh myocardial infarction and (or) heart failure and (or) intoxication with digitalis drugs, the general condition of the patient is serious. Fainting, attacks of Morgagni-Edams-Stokes syndrome, angina pectoris and heart failure refractory to drug therapy are often observed.
There are three main physical signs,
the presence of which in combination suggests that there is atrioventricular rhythm:
Bradycardia with regular rhythm (rate between 40 and 60 per minute)
Increased first heart sound
Increased pulsation of the neck veins engorged with blood
The intensified first sound in the upper node rhythm is due to the fact that the ventricular systole that occurs immediately after the atrial systole finds the valve flaps between the atria and ventricles wide open, as a result of which they slam shut with considerable force. Increased pulsations of the jugular veins are caused by the fact that contractions of the atria occur when the tricuspid valve is closed due to simultaneous or almost simultaneous contraction of the atria and ventricles, and blood from the right atrium returns in the opposite direction to the jugular veins. Pulsations of the neck veins coincide with systole. They are synchronous with the first heart sound and the pulse on the radial artery. A venogram of the neck veins helps make the diagnosis. It establishes a high amplitude of the atrial wave “a”, coinciding with the QRS complex on the ECG.
It is very rare to find all three signs. Therefore, it is impossible to detect atrioventricular rhythm without an electrocardiogram. Usually the only physical sign that raises suspicion of the presence of atrioventricular rhythm is bradycardia with a contraction rate of 40-60 beats per minute with a regular rhythm,
Electrocardiogram
There are two main types of atrioventricular rhythm:
A. Nodal rhythm with retrograde wave P'
B. Junctional rhythm with atrioventricular dissociation without retrograde wave P'
Junctional rhythm with retrograde P' wave
(Isolated or “pure” form of atrioventricular rhythm)
This form of atrioventricular rhythm is relatively rare. It occurs with prolonged sinus node failure or sinoauricular block until impulses other than retrograde nodal impulses reach the atria and activate the atria. The P' wave is negative in leads 2, 3 and aVF and positive in lead aVR. Its electrical axis (ap) is between -60 and -90°. Wave P'
positive in the I, aVL and left precordial leads
of the nodes
-Ve- The position of the P' wave in relation to the ventricular complex depends on the location of the ectopic focus in the atrioventricular system and (or) on the state of anterograde and retrograde atrioventricular conduction. The P' wave may be before, on, or behind the QRS complex. The P'-R interval is shortened <0.12 seconds, and the R-P' interval is within 0.10 and 0.20 seconds, provided that there is no slow atrioventricular conduction in the retrograde or anterograde way. The AV rate is most often between 40 and 60 beats per minute and rarely between 30 and 40 per minute. In most cases, the atrioventricular rhythm is correct and rarely fluctuates above 0.04 seconds. With atrioventricular rhythm, the excitation of the ventricles occurs in a normal way and therefore the ventricular complexes have a normal shape and width, or there is a slight deformation of them. The ventricular complexes are widened and split when the junctional rhythm is combined with a previous bundle branch block or aberrant ventricular conduction. Such deformed QRS complexes are difficult to distinguish from idioventricular rhythm complexes.
Atrioventricular rhythm with a negative P' wave before the ventricular complex ("upper" nodal rhythm)
There is a failure of the sinoauricular node or prolonged sinoauricular block. Excitation originates in the atrioventricular system. The atria are activated “retrogradely and before the ventricles. The P' wave appears very close to the ventricular complex (P'-R interval less than 0.12 seconds). It is negative in leads II, III, aVF and positive in leads aVR, I and aVL. In V1 and V2 the P' wave is two-phase with the first negative phase. The rhythm is correct with a frequency of 52 beats per minute. The width and shape of the ventricular complex are normal
The atrioventricular ri is hidden in the QRS complex. Its presence can be proven using esophageal and intracardiac leads. The rhythm is correct, its frequency is 48 per minute. The shape and width of the ventricular complex are normal
Atrioventricular rhythm with a negative P' wave located after the ventricular complex (“lower” nodal rhythm)
There is sinus node failure or prolonged sinoauricular block. Excitation originates in the atrioventricular system. Excitation of the ventricles occurs before the atria. P' waves are located directly behind the ventricular complex and superimpose on the beginning of the ST interval. They are negative in leads II, III and aVF and positive in leads aVR, I and aVL. The rhythm is correct, its frequency is 56 v. minute. The shape and width of the ventricular complex are normal
Junctional rhythm with atrioventricular dissociation without retrograde P' wave
This form of atrioventricular rhythm is much more common and will be discussed in detail in the chapter on atrioventricular dissociation. Junctional rhythm with atrioventricular dissociation without retrograde excitation of the atria appears in three conditions:
1. When the atria are excited by a sinus impulse just before the atrioventricular impulse reaches the atria. The atria have a sinus rhythm, and the ventricles have a nodal rhythm. Sinus atrial and nodal ventricular rhythms are independent of each other.
2. When there is complete atrioventricular block with retrograde blocking of nodal impulses. In this case, sinus rhythm of the atria and nodal rhythm of the ventricles, which are independent of each other, are also observed.
3. When there is atrial fibrillation or flutter in combination with high-grade or complete atrioventricular block. In this case, the ectopic atrial rhythm is independent of the nodal rhythm. This condition is characteristic of intoxication with digitalis preparations.
Atrioventricular rhythm with complete atrioventricular block
Due to the retrograde blocking of nodal impulses, there are no retrograde P' waves.
The atria contract under the influence of sinus impulses. P' waves are positive
Heart rate less than 40 beats per minute.
Ventricular complexes are unchanged. They do not depend on ventricular contractions occurring under the influence of nodal impulses. The nodal rhythm is correct, its frequency is 38 per minute
The shape and width of the ventricular complexes are normal
Differential diagnosis.
Without an electrocardiogram, it is usually impossible to distinguish atrioventricular rhythm from sinus bradycardia. It should be borne in mind that the atrioventricular rhythm may increase slightly after physical exertion, emotions, or the use of atropine, but usually to a much lower extent than that inherent in sinus bradycardia. Junctional rhythm with preceding bundle branch block or aberrant conduction is difficult to distinguish from idioventricular rhythm. Typically, the frequency of the atrioventricular rhythm is higher (40-60 per minute) than the idioventricular rhythm (30-40 per minute). Aberrant QRS complexes often resemble normal ventricular complexes and in most cases have the form of right bundle branch block. The ventricular rate during atrial fibrillation can be less than 60 per minute without the presence of a replacement junctional rhythm. In such cases, the activity of the ventricles is very irregular and slow (bradyarrhythmia with atrial fibrillation). In atrioventricular dissociation, when there is sinus rhythm for the atria and nodal rhythm for the ventricles, sinus waves P may fall close to the QRS complex, and then the rhythm will look like ordinary sinus bradycardia. To identify the nodal rhythm in such cases, short (less than 0.12 seconds) P-R intervals are important.
In contrast to the nodal rhythm, with the left atrium rhythm there is a positive P' wave in lead V1, which has the shape of a “dome and spear”, and a negative P' wave in leads I and (or) V6.
Junctional tachycardia with varying degrees of exit block resembles atrioventricular escape rhythm. Long R-R intervals in junctional tachycardia with outlet block are usually multiples of short R-R intervals.
Treatment of junctional rhythm depends on the cardiac arrhythmia causing it. When there is a short junctional rhythm with sinus bradycardia, there is usually no need for treatment. On the contrary, a junctional rhythm with complete atrioventricular block with hemodynamic disturbances and significant symptoms usually necessitates the use of an artificial pacemaker (electrical stimulator). The main drugs for atrioventricular rhythm are atropine, isoprenaline and orciprenaline (alupent) in doses used for sinus bradycardia. If the occurrence of atrioventricular rhythm coincides with treatment with digitalis, quinidine, reserpine, guanethidine, these medications should be discontinued. Antiarrhythmic drugs - quinidine, procainamide, ajmaline and beta blockers are contraindicated. Treatment of junctional rhythm with hyperkalemia and (or) acidosis should be carried out by prescribing 1-3 ampoules of sodium bicarbonate (one ampoule contains 44.6 mEq) and 25% glucose 250 ml with 20 IU insulin, for drip intravenous infusion for 30 minutes and then 1000 ml of 10% glucose intravenously by drip over 6-8 hours.
The prognosis for atrioventricular rhythm depends on the cardiac arrhythmia that caused the rhythm, the presence or absence of heart disease, and the ventricular rate. The prognosis is very good in healthy individuals with sinus bradycardia and short periods of atrioventricular rhythm. The prognosis is serious when the junctional rhythm is the result of complete atrioventricular block, with heart disease and heart failure. Junctional rhythm in atrial fibrillation with intoxication with digitalis preparations causes a serious prognosis. The lower the junctional rate, the greater the likelihood of Morgagni-Edams-Stokes syndrome and drug-resistant heart failure.
RHYTHM FROM THE CORONARY SINUS (SINUS VENOSUS CORONARIUS)
This rhythm is a type of atrioventricular rhythm. Impulses with it arise in the pacemaker cells located low in the right atrium, near the mouth of the venous coronary sinus.
The rhythm from the coronary venous sinus, as well as the rhythm from the atrioventricular node, is characterized by bradycardia with a frequency of 40-60 per minute and retrograde activation of the atria. Impulses emanating from the coronary venous sinus, in contrast to the nodal sinus, travel along the entire length of the atrioventricular system and then reach the ventricles. As a result, the P'-R interval during coronary rhythm has a normal duration and is above 0.12 seconds.
In such cases, there is a prolonged failure of the snoauricular node or sinoauricular block with a replacement rhythm from the venous coronary sinus.
The main sign by which the rhythm from the venous coronary sinus differs from the “upper” nodal rhythm is the absence of a shortened P'-R interval.
The rhythm is correct, the frequency is 56 beats per minute. Wave P' is negative in leads II, III and aVF and positive in leads aVR, I and aVL
It should be emphasized that it is impossible to distinguish the rhythm generated by the coronary venous sinus from the upper nodal rhythm when, with the latter, there is slow conduction by the anterograde route and the P'-R interval is more than 0.12 seconds. The P'-R interval with a rhythm from the venous coronary sinus and with a nodal rhythm can be more than 0.20 seconds when there is significant atrioventricular block.
Clinical significance, treatment and prognosis
the rhythm from the venous coronary sinus is the same as with the nodal rhythm.
WANDERING RHYTHM
Synonyms: sliding rhythm, migrating rhythm, pacemaker migration, Wandering pacemaker, wandernder Schrittmacher. There are several variants of the wandering rhythm.
Wandering rhythm in the sinus node
The P wave is positive and has sinus origin. Its shape changes with different heart contractions. The P-R interval remains relatively constant. Severe sinus arrhythmia is always present. In essence, the migration of impulse formation between separate groups of cells in the sinoauricular node is a variant of sinus arrhythmia.
Wandering rhythm in the atria
Wave P is positive. Its shape and size change with different heart contractions. Along with this, the duration of the P-R interval also changes. Rhythm migration in the atria often has an active impulse generation mechanism and causes the so-called chaotic atrial tachycardia (see page 97).
Wandering rhythm between the sinus and atrioventricular nodes
This is the most common variant of the wandering rhythm. With it, the heart contracts under the influence of excitation impulses from the center, periodically changing its location, gradually moving from the sinus node to the atrial muscles, the region of the coronary sinus, less often reaching the atrioventricular node, and again returning back to the sinus node. A wandering rhythm is rare and usually its migration is fleeting. The clinical significance of this rhythm is the same as that of sinus arrhythmia.
Mechanism.
Rhythm migration is the result of periodic changes in the intensity of vagal impulses that affect the function of the sinus node. Increased tone of the vagus nerve depresses the sinus node and the center of excitation moves down to the atrioventricular node. With decreased tone of the vagus nerve, the sinus node is activated again and the center of excitation returns to its old place.
In fact, the question concerns the replacement rhythm due to temporary, transient depression of sinus function and activation of lower autonomous centers, most often in the atrial muscles.
Etiology
Vagotonia in healthy people - most often
Intoxication with digitalis or quinidine preparations, infectious diseases
Organic heart diseases - rheumatic heart disease, heart valve defects, coronary disease
Heart surgery
Clinical picture.
When the pacemaker migrates, there are no clinical signs at all. Mild arrhythmia is often detected - a gradual decrease in heart rate when the center of excitation moves to the atria and atrioventricular node and an increase in heart rate when the pacemaker returns to the sinus node.
Clinically, wandering rhythm cannot be distinguished from sinus arrhythmia without an electrocardiogram.
Electrocardiographic criteria
rhythm migration between the sinoauricular and atrioventricular nodes:
1. Change in the shape and size of the P wave, which gradually decreases, becomes deformed, becomes nzoelectric and at the end negative, after which it gradually becomes positive
2. The P-R interval gradually shortens and then the sheaf lengthens. Shortening can reach 0.12 seconds or less if the center of excitation moves to the atrioventricular node
3. Ventricular complexes remain unchanged. A slight arrhythmia may be observed - a decrease in heart rate when the center of excitation moves downward, and an acceleration when it returns to the sinus node
Diagnosis
is possible only on the basis of electrocardiographic studies. Rhythm migration should be distinguished from sinus arrhythmia with a change in the P wave configuration in connection with breathing, from some cases of frequent atrial extrasystoles, and from some forms of atrioventricular dissociation and sinoauricular block.
Treatment
not necessary. If digitalis and quinndine preparations are considered to be the cause of rhythm migration, their use should be temporarily discontinued. The administration of atropine is necessary only for severe vagotoia.
IDIOVENTRICULAR RHYTHM
Synonyms:
intrinsic ventricular rhythm, ventricular automatism, intraventricular rhythm.
With idioventricular rhythm, ventricular contraction impulses constantly arise in the center located in the ventricles themselves. Most often, this center is located in the upper part of the interventricular septum, in one of the two legs and their branches of the bundle of His (“bundle branch rhythm”) and less often in the fibers of the Purknier network. Idioventricular rhythm is defined as the presence of six or more successive replacement idioventricular contractions.
Mechanism.
The idioventricular rhythm is of a replacement nature. It occurs only in the absence of impulses from the sinus and (or) atrioventricular node. A significant decrease or absence of impulses simultaneously from the sinoauricular and atrioventricular nodes allows the third-order center localized below, located in the ventricles, to replace the first- and second-order centers.
The most common cause of idioventricular rhythm is high-grade or complete atrioventricular block. Less commonly, such a rhythm is observed with sinus node failure or sinoauricular block, when the atrioventricular system cannot create replacement impulses. Idioventricular rhythm can occur in the presence of ectopic atrial rhythm - fibrillation, atrial flutter, atrial tachycardia, when atrial impulses do not reach the ventricles due to the presence of a high degree or complete atrioventricular block. Often, idioventricular rhythm occurs without excitation of the atria (atrial asystole) as a terminal condition in severe heart disease.
Etiology.
Idioventricular rhythm is almost always caused by advanced cardiac disease. Its etiology coincides with the etiology of complete atrioventricular block, sinus node failure and sinoauricular block.
Hemodynamics.
Ohm depends on the nature and severity of the underlying heart disease and the ventricular rate.
Significant hemodynamic disturbances occur with a very slow
ventricular rate. Significant hemodynamic disturbances occur with a strong decrease in ventricular contractions and advanced cardiac disease.
Clinical picture.
Idioventricular rhythm can be suspected in the presence of bradycardia less than 40 beats per minute of the correct rhythm, which is not affected by physical effort and the use of atropine or is only slightly affected. In most cases, there is advanced cardiac disease, attacks of Morgagni-Edams-Stokes syndrome, or heart failure refractory to drug treatment. With idioventricular rhythm, there is a pronounced tendency to the occurrence of ventricular tachycardia, ventricular flutter and fibrillation, ventricular asystole and sudden death. Idioventricular rhythm, especially in the absence of atrial activity (atrial asystole), is most often the terminal arrhythmia of a dying heart.
Electrocardiographic criteria for idioventricular rhythm
1. Widened and severely deformed ventricular complexes, as with ventricular extrasystoles and ventricular tachycardia. The width of the QRS complex is almost always greater than 0.12 seconds. Very dilated and highly deformed ventricular complexes are characteristic of terminal idioventricular rhythm. Sometimes two or more different QRS shapes can be observed, as an expression of two or more foci of impulse generation.
2. The rate is usually 30-40 per minute, but can be less than 30 or sometimes slightly more than 40 per minute. Terminal Idioventricular rhythm is very slow and unstable.
3. The rhythm is most often correct, but it can also be incorrect. The abnormal rhythm is due to the presence of several ectopic foci in the ventricles or the presence of one focus of excitation with varying degrees of impulse formation or exit block ("exit block")
4. Almost always, the atrial rhythm does not depend on the ventricular rhythm, i.e. There is complete atrioventricular dissociation. The atrial rhythm can be sinus or ectopic—atrial fibrillation, atrial flutter. In some cases, atrial asystole is observed due to the absence of sinus impulses, or when the atria lose their ability to be activated. It is extremely rare that a retrograde negative P wave may appear immediately after widened QRS complexes. Typically, ventricular impulses are not conducted retrogradely through the atrioventricular node.
Idioventricular rhythm with complete atrioventricular block
The atria contract under the influence of sinus impulses, regardless of the ventricular rhythm. The ventricular complexes are dilated and deformed. The ventricular rhythm is correct and its frequency is 30 beats per minute
Differential diagnosis.
All types of bradycardia should be kept in mind. It is most difficult to differentiate from junctional rhythm, in which there are dilated and distorted ventricular complexes due to the presence of a previous bundle branch block or aberrant ventricular conduction. The presence of a junctional rhythm is indicated by a higher ventricular rate (40-60 per minute) and, possibly, a more minor deformation of the QRS complex.
Treatment.
In case of idioventricular rhythm, antiarrhythmic drugs such as procainamide, quinidine, ajmaline are contraindicated, as they can cause depression of the last third-order center and ventricular asystole. Treatment is the same as for sinoauricular and atrioventricular blockade. In many cases it is necessary to use an artificial electrical stimulator.
The prognosis depends on the nature and severity of the underlying heart disease and the degree of slowing of cardiac activity.
JUMPING ABBREVIATIONS
Synonyms:
Replacement systoles, escape systoles, Ersatzsystolen, echappements ventriculaires, individual automatic contractions of the ventricles.
Jumping contractions are time-delayed single contractions of the heart that appear with decreased sinus node function and are caused by impulses emanating from the atrioventricular node, and much less often by impulses from the ventricles. They differ from the replacement atrioventricular and idioventricular rhythm only in that in this case there is no long period of contractions, but only single contractions.
Mechanism.
Normally, impulses from the sinus node inhibit the activity of lower-level autonomous centers. For jump-off contractions to occur, the function of the sinus node must be suppressed - sinus bradycardia, or the conduction of sinus impulses must be temporarily interrupted - sinoauricular block, partial atrioventricular block. Only then, after a longer diastolic pause, impulses emanating from lower-lying autonomous centers, although their excitability is not changed, can cause a contraction of the heart. Most often, jumping contractions appear with severe sinus bradycardia and sinus arrhythmia during periods of significantly slow cardiac activity.
Jumping contractions also appear in pauses of sinus node failure, sinoauricular and partial atrioventricular block, and very often after longer extrasystolic pauses or immediately after the cessation of ectopic paroxysmal tachycardia.
Etiology
jumping contractions coincides with the ethnology of the main rhythm disturbance that created the conditions for their occurrence.
Clinical picture.
During auscultation, arrhythmia is detected, but, unlike extrasystoles, the pause before the jumping contraction is long, i.e., a delayed contraction of the heart has occurred. The first tone of the jumping contraction may be enhanced due to prolonged filling of the ventricles and due to the fact that most often jumping contractions are of nodal origin.
When examining the pulse, single, longer diastolic pauses are detected, which to a certain extent violate its correctness. These two auscultatory symptoms of a jumping contraction are not always well expressed. There may be no increase in the first sound, and the increase in the diastolic pause before the jump-out contraction may not be as obvious, especially in the presence of sinus arrhythmia. This makes clinical detection of these symptoms impossible. Jumping contractions have little clinical significance.
Diagnosis
jumping contractions are usually electrocardiographic.
Electrocardiogram.
According to the place of their occurrence, jump-out contractions are most often nodal and very rarely ventricular. Jumping contractions appear late and the interval between the last contraction emanating from the sinus node and the jumping contraction is always greater than the longest sinus cycle; the QRS complex is not preceded by a sinus wave P or, if present, is not associated with the ventricular complex, and the P-R interval is shorter than normal.
Nodal pop-up systoles
1. The R-R interval before the jumping contraction is always longer than one whole normal interval, and not shortened as with extrasystoles
2. R-R interval after a pop-up contraction of normal length. and not elongated as with extrasystoles, and in all cases shorter than the interval preceding the jumping contraction
3. Jumping contractions, as a rule, come from the atrioventricular node, which is why the ventricular complexes are identical in shape to the others and can be recognized by the position of the negative P wave or its absence, according to three variants of the nodal rhythm
Ventricular jump contractions
Very rarely, jumping contractions come from an autonomous center located in the ventricles, and then the ventricular complex is deformed and expanded
Differential diagnosis.
The distinction between nodal and ventricular jump-out contractions from nodal and, accordingly, ventricular extrasystoles is made on the basis of a longer diastolic pause before jump-out contractions and the absence of an extended pause after them. With extrasystoles, the ratios are completely opposite - a short diastolic pause before the extrasystoles and an extended one after them.
Jumping contractions indicate inhibition of sinus node function or blockade of sinus impulses and therefore, unlike extrasystoles, antiarrhythmic drugs (quinidine, procainamide, ajmaline) are contraindicated in their treatment.
From the point of view of clinical practice, jumping contractions signal the possibility of a transition from sinus rhythm to one of the types of atrioventricular rhythm. Jumping contractions also occur in individuals with a healthy heart and increased vagus nerve tone. In the latter case, after administration of atropine, sinus rhythm is restored.
Ratios of the length of diastolic pauses before and after extrasystole and jump-out contraction
ACTIVE ECTOPIC RHYTHM DISORDERS
In contrast to passive replacement rhythms, in which the primary cause is damage or functional inhibition of the sinus node, active ectopic rhythms arise in an ectopic focus with pathologically increased excitability, which leads to overcoming and suppressing the function of the sinus node. When the ectopic focus is located in autonomous centers of the second order, the ventricular complex on the electrocardiogram is not changed, and when the focus is in third-order centers, it is deformed.
The following active rhythm disturbances are distinguished:
Extrasystole
Atrial, nodal and ventricular tachycardias -
paroxysmal and non-paroxysmal
Atrial flutter and fibrillation
Ventricular flutter and fibrillation
Parasystoles
The frequency of impulses emanating from an ectopic focus located in the atria, atrioventricular system or ventricles determines the type of arrhythmia.
Scheme of active ectopic rhythm disturbances depending on the frequency of ectopic impulses
Ectopic focus in the atria
| Pulses per minute | Type of arrhythmia | ||
| Single or group 100-200 | Atrial extrasystoles Non-paroxysmal, chaotic atrial tachycardia | ||
| 140—220 | Paroxysmal atrial tachycardia | ||
| 220—350 | Atrial flutter | ||
| 350—650 or more | Atrial fibrillation | ||
Ectopic focus in the atrioventricular node
| Pulses per minute | Type of arrhythmia |
| Single or group | Nodal extrasystoles |
| 60—150 | Non-paroxysmal junctional tachycardia |
| 150—220 | Paroxysmal junctional tachycardia |
Ectopic focus in the ventricles
| Pulses per minute | Type of arrhythmia |
| Less than sinus node frequency - single or group | Ventricular extrasystoles Group (volley) extrasystoles |
| Several consecutive impulses from 55 to 100 | Slow ventricular tachycardia |
| from 100 to almost 220 | Ventricular paroxysmal tachycardia |
| from 150 to almost 300 | Ventricular flutter |
| from 150 to 500 | Ventricular fibrillation |
Causes of cardiac arrest
About 5% of severe cardiac pathologies lead to the patient developing cardiac asystole. The causes of this life-threatening condition most often lie in the occurrence of an acute form of myocardial infarction or pulmonary embolism.
Asystole can also be provoked by an overdose of cardiac glycosides, antiarrhythmic drugs or anesthesia, which affect the functioning of the said muscle. Cardiac arrest can also be caused by electrical trauma, intracardiac manipulation, or general severe metabolic disorders.
How is this disease diagnosed?
Considering the fact that in the event of cardiac arrest, resuscitation methods are necessary immediately, since a person’s life depends on it, diagnosis should also take only a few minutes. First you need to perform a physical examination, it is needed to determine the absence of breathing and pulse. The pulse is checked in the carotid artery, which is located in the neck. In addition, you need to pay attention to the reaction of the pupils to light, as well as changes in the skin.
After providing the victim with the necessary first aid, he needs to undergo EKN; it will help determine the activity of the organ and prescribe the correct method of further treatment.
Features of ventricular asystole
It should be mentioned that it is the asystole of the ventricles of the heart (complete stop of their contractions), in contrast to the atrial asystole compatible with life, that leads to the death of the patient.
- What is cardiac asystole, causes and first signs, emergency care and consequences
This pathology does not apply to those rhythm disturbances that are provoked by increased ectopic excitability. The causes of its occurrence are conduction disturbances with parallel inhibition of the ability of the ventricles to contract rhythmically.
Most often, this condition may be the result of ventricular flutter or fibrillation and occurs after them, and in some cases it is provoked by electromechanical dissociation or ventricular tachycardia.
Cardiac causes of asystole
This group of factors causes primary asystole, that is, associated with electrical instability of the myocardium itself, often against the background of ischemia (oxygen starvation of tissues).
Heart attack
General acute malnutrition of muscle structures. It occurs as a result of long-term coronary insufficiency, atherosclerosis, thromboembolism and other phenomena of this kind.
The development of cardiac asystole is a consequence of extensive damage, if the area reaches more than 25% or about a similar value. Possible delayed development. Thus, some patients suffer from cardiac arrest within a few days.
The most dangerous period is the first 72 hours. Further, the risks decrease, but remain throughout life, since a heart attack does not go away without a trace.
Cardiosclerosis, persistent heart failure, these are the reasons for the possible development of asystole. Lifelong maintenance treatment and constant monitoring of the condition are indicated.
- First aid for cardiac arrest - Emergency aid algorithm 2020
Decrease in the amount of blood circulating in the body
It has a dual nature. On the one hand, there is a possibility of classic bleeding, when liquid connective tissue leaves the closed system. Then the physical variety takes place.
On the other hand, everything can be more complicated. Against the background of pathologies of the mitral valve and aorta, incomplete ejection and movement in a large circle are possible. Hence the decrease in the amount of circulating blood against the background of a preserved nominal volume.
This is no less dangerous, rather the opposite: transfusion in such a situation is pointless, the problem is of an organic nature.
Cardiac tamponade
Accumulation of blood around. Liquids are also possible. The result of an injury, long-term swelling, and inflammatory process. Recovery is carried out surgically as a matter of urgency.
Pulmonary embolism
Refers to cardiac causes conditionally. The essence of the phenomenon is the blockage of a large vessel with a blood clot.
It can be either a result of the chest injury itself or a consequence of distant damage to anatomical structures (in a large circle the blood clot moves throughout the body and penetrates the pulmonary artery).
It is also possible that spontaneous rupture of small vessels may occur due to the use of anti-inflammatory drugs, corticosteroids, hematological conditions, or excessive thickening of fluid connective tissue.
Such problems are resolved before urgent processes arise. The chances of survival from thromboembolism are almost zero.
- Extrasystole of the heart causes and symptoms treatment