Sudden cardiac arrest on the street: what to do before the ambulance arrives?
Resuscitation measures are carried out after establishing a state of clinical death, the main signs of which are: absent breathing and heartbeat, unconsciousness, dilated pupils, lack of response to external stimuli. To reliably determine the severity of the situation, it is necessary to determine the following indicators of the victim:
- check the pulse in the carotid arteries of the neck at the jaw angle - when the pressure drops to less than 60-50 mm Hg. Art. the pulse on the radial artery of the inner surface of the hand is not detected;
- examine the chest, check for spontaneous breathing movements;
- approach the victim’s face to check breathing, determine inhalation and exhalation (air movement assessment);
- pay attention to the color of the skin - cyanosis and severe pallor appear when breathing stops;
- check consciousness - lack of response to stimuli indicates coma.
Cardiopulmonary resuscitation according to the new standards is carried out only in two cases. You should start performing CPR only after determining your pulse and breathing.
If the pulse is clearly detected for 10-15 seconds and atonal breathing is disturbed with episodes of convulsive sighs, artificial respiration is required. To do this, you need to take 10-12 breaths “mouth to mouth” or “mouth to nose” over the course of a minute. While waiting for an ambulance, you need to measure your pulse every minute; if it is absent, CPR is indicated.
If spontaneous breathing and pulse fail, a set of resuscitation measures is indicated strictly according to the algorithm.
Consciousness testing is carried out according to the following principle:
- Address the victim loudly. Ask what happened and how he feels.
If there is no response, use painful stimuli. Pinch the top edge of the trapezius muscle or apply pressure at the base of the nose.- If there is no reaction (speech, twitching, attempts to defend yourself with your hand) - there is no consciousness, you can move on to the next stage.
Breath test:
- Tilt your head back (holding it by the back of your head and chin) and open your mouth. Inspect it for foreign bodies. If they are there, remove them.
- Bend towards your face and for 10 seconds. check your breathing. You should feel it with your cheek and hear and see the movements of your chest. Normally, 2-3 breaths are sufficient.
- If there is no breathing or only 1 breath is felt (which can be considered its absence), we can assume the cessation of a vital function.
In such a case, it is necessary to call an ambulance and begin performing resuscitation measures in case of cardiac and respiratory arrest.
Stages and stages of resuscitation
A set of emergency measures carried out to patients in a state of clinical death, aimed at restoring the body’s vital functions and preventing irreversible damage to its organs and systems, is called resuscitation. The person who revives the victim is called a resuscitator.
Returning a patient to a full life from a state of clinical death is possible only with a qualified and consistent implementation of a complex of resuscitation measures.
The first stage of resuscitation is the provision of first aid (basic life support) carried out by a resuscitator (not necessarily a medical worker, but every trained person who has basic resuscitation skills). After clinical death is declared (which should take no more than 7-8 seconds!), preparatory measures are immediately carried out: the victim is laid on his back, preferably with the upper part of his body lowered, on a solid base. A savior who is not involved in intensive care lifts the victim’s legs 50–60 cm upward to drain blood from them and increase blood supply to the cavities of the heart.
The first stage of resuscitation is to ensure airway patency. The resuscitator performs a “triple technique” (according to P. Safar):
a) opens the victim’s mouth and with a finger wrapped in a handkerchief (gauze cloth for clamps) frees him from foreign bodies and liquids (vomit, sputum, algae, inserted crevices, blood clots, etc.);
b) tilts the victim’s head as far back as possible, placing an improvised cushion under the neck (for example, the forearms). In this case, in most victims, the upper respiratory tract is freed from the tongue and its root, becoming open;
c) brings the lower jaw forward. The patency of the upper respiratory tract is restored in other cases.
The second stage of resuscitation is performing mouth-to-mouth artificial ventilation. Having covered the victim's mouth with a bandage (handkerchief), the resuscitator tightly covers his mouth with his lips and exhales. Mandatory condition: the victim's head is tilted back, his nostrils are pinched with the thumb and forefinger (so that the air does not return back), the exhalation volume for adults should be 800 - 1000 ml. When blowing air, the resuscitator, out of the corner of his eye, watches the movements of the victim’s chest, which should rise and fall. Having made 2 - 3 exhalations, the savior begins to carry out the next stage of resuscitation.
The third stage of resuscitation is closed cardiac massage. Being on the side of the victim, the resuscitator places one hand on the lower third of the sternum, strictly in the middle, so that the fingers are raised up and placed parallel to the ribs. He places the second hand on top and, pressing rhythmically, moves the sternum in the sagittal direction to a depth of 3 - 5 cm. The frequency of pressing is 60 per minute.
Mandatory condition: when pressing on the sternum, the fingers of the hand should be raised up to prevent fractures of the ribs, and the arms should be straightened at the elbow joints. Cardiac massage is thus carried out by the mass of the resuscitator’s torso. Subsequently, the rescuer alternately injects air and presses on the sternum in a ratio of 1: 4. If there are two resuscitators, each of them performs its own stage of resuscitation. If necessary, each time remove the lower jaw to ensure patency, breathe in the 2nd and 3rd stages in a ratio of 2: 10.
Signs of effective resuscitation measures :
- constriction of the pupils,
- normalization of skin color,
- feeling under the fingers of arterial pulsation, synchronous with the massage;
- Sometimes blood pressure is determined.
In some cases, cardiac activity may be restored. The first stage of resuscitation should be carried out continuously until the arrival of a specialized medical team.
The second stage of cardiopulmonary resuscitation is the provision of specialized medical care (further life support). It is carried out by professional doctors using monitoring, diagnostic, therapeutic equipment and medications. Under the control of a laryngoscope, a portable or electric suction is used to better clean the airways and intubate the trachea.
The resuscitation team provides more effective artificial ventilation of the lungs - with a manual portable or stationary ventilator through a mask, air duct or endotracheal tube with an air-oxygen mixture. If you have a special massager, you can perform closed cardiac massage using hardware.
At this stage, the following stages of resuscitation are carried out alternately. The first stage is drug therapy. For all types of circulatory arrest, solutions of adrenaline hydrochloride (1 ml of 0.1% solution) and atropine sulfate (3 ml of 0.1% solution) are used. The second stage is assessing the type of circulatory arrest. For adequate drug therapy, it is necessary to diagnose the functional state of the victim’s heart. To do this, the patient is connected to an electrocardiograph (cardioscope) in the second lead and the curve is recorded.
There are the following types of circulatory arrest : asystole, fibrillation, “ineffective heart”.
- During asystole, the electrocardiograph records a straight line.
- Ventricular fibrillation is manifested by frequent chaotic contraction of individual myocardial fibers (uneven “teeth” of high, medium and variable amplitude).
- “Ineffective heart” - registration of the ventricular complex on the ECG in patients with absent pumping function of the heart.
Ventricular fibrillation and an “ineffective heart” without appropriate correction, as the energy resources of the myocardium decrease, quickly turn into asystole. In the presence of high-wave fibrillation, you can use a 2% lidocaine solution (0.5 mg per 1 kg of body weight, repeatedly).
In case of an “ineffective heart” caused by a sharp decrease in the volume of circulating blood, to ensure its pumping function, hemodynamic media (refortan, stabizol, polyglucin, rheopolyglucin), crystalloids, and glucocorticoids are infused intravenously or intraarterially; in case of massive blood loss - canned blood and its components.
In case of cardiac arrest caused by hyperkalemia or hypocalcemia (acute and chronic renal failure, hemolysis of red blood cells, massive tissue destruction, hypoparathyroidism), calcium chloride should be used (5 - 10 ml of 10% solution, intravenously). Medicinal media are administered intravenously, into the lumen of the trachea, through a cannulated artery, intracardiacly.
Medians administered intravenously, with effective cardiac massage, enter the coronary vessels, exerting their influence on the heart. If it is impossible to provide venous access, the intratracheal method is used, which is no less effective. In this case, with a needle for intramuscular injections, the cricothyroid ligament or the space between the tracheal rings is pierced and solutions of adrenaline, atropine or lidocaine are injected (2-3 ml of 0.1% solution of adrenaline hydrochloride, 1 ml of 0.1% solution of atropine sulfate, 2 ml of 2% lidocaine solution - diluting them in 10 ml of sodium chloride solution). These medications can also be given through an endotracheal tube. During ventilation of the lungs at this time, medicinal media penetrate through the alveoli, and after 30-40 seconds enter the lumen of the coronary vessels.
According to some researchers, using distilled water as a solvent can achieve effective absorption of the solution from the alveoli into the blood due to the difference in osmotic pressure. Due to the large number of complications, intracardiac administration of drugs is used less and less (the technique is described below).
The intra-arterial method of infusion in patients with a significant loss of circulating blood volume (for example, with hemorrhagic shock and an “ineffective heart”) also deserves attention Infusion of blood and other agents into a catheterized artery (eg, radial) is often effective in filling the coronary arteries with blood, ensuring efficient cardiac function and restoring hemodynamics.
The third stage is electrical defibrillation of the heart. It is used in patients with ventricular fibrillation (the method is described below). In an operating room, it is sometimes more effective to perform open cardiac massage. Indications: cardiac arrest during surgery on the organs of the chest and upper abdomen; cardiac tamponade; bilateral pneumothorax; multiple fenestrated rib fractures; congenital and acquired deformities of the chest, which make it impossible to conduct effective closed massage. Open massage is carried out through transthoracic or subdiaphragmatic access, without opening or with opening of the cardiac membrane.
A prerequisite for this is that the fingers of one or both hands, when squeezing the ventricles, should be placed along the vascular bundle so as not to pinch it. The third stage of cardiopulmonary resuscitation.
Stages of cardiopulmonary resuscitation according to new standards
It is extremely important to follow the correct procedure for resuscitation measures. According to the latest medical protocols, to save the victim it is necessary to adhere to the following algorithm:
- A - ensure airway patency for oxygenation, eliminate blockage of the lumen of the pharynx and trachea;
- B - perform breathing using the “mouth to mouth” or “mouth to nose” method;
- C - restore blood circulation using indirect massage.
Technique and procedure for performing indirect cardiac massage and artificial ventilation of the lungs
- It is important to maintain safety; before starting CPR, the person must be placed on a rigid, stable and solid surface or floor.
- After this, tilt your head to the side, open your mouth slightly and make sure that the airway is not blocked. If obstruction is detected, clear the airways using improvised means (handkerchief or napkin).
- For effective artificial respiration, perform the Safar maneuver - tilt your head back, push your jaw forward and upward, and open your mouth in one movement.
- If there are signs of a spinal fracture in the neck area, just move your jaw.
- The resuscitation complex begins with 30 compressions of the sternum, which are performed by one person rhythmically without breaks.
- To do this, you need to place your right hand with your palm resting on the lower part of the sternum in the center, place your left hand on top of your right hand and interlace your fingers.
To perform a heart massage, your arms should be straight, not bent at the elbow joints.- Perform 100-120 compressions per minute with rhythmic compression of the sternum 5-6 cm deep, until the chest is completely expanded after compression.
- After 30 compressions, exhale 2 times into the victim’s mouth or nose for 1 second.
- When breathing using the mouth-to-mouth method, you must close your nostrils with your fingers before exhaling.
- During two exhalations, you should look at the chest: straightening and lifting indicate correct execution.
- If the chest does not rise or fall, it is necessary to check whether the airways are passable, and you may need to repeat Safar.
- During CPR, be sure to check your pulse every 2 minutes. Resuscitate without stopping for up to 30-40 minutes.
Criteria for the effectiveness of activities
With timely assistance, the chance of saving a person increases. To do this, it is important to strictly follow the rules of cardiopulmonary resuscitation. The effective implementation of the CPR complex is indicated by:
- the appearance of a pulse in the carotid arteries - to make sure that the pulse is maintained, cardiac massage can be stopped for 3-5 seconds;
- return of the pupillary reaction to a light stimulus - narrowing indicates an enrichment of oxygenated blood in the brain;
- the appearance of spontaneous breathing with full, steady inhalation and exhalation, without episodes of convulsive inhalations followed by cessation (apnea);
- disappearance of blueness of the skin of the face, lips, hands;
After the heartbeat and breathing are restored, the resuscitation complex is stopped, but the victim must remain in the field of view of the resuscitator until the doctor arrives
Common mistakes in providing assistance
It should be remembered that incorrectly provided first aid often causes more harm than its absence. The following erroneous recommendations and myths are often found on the Internet (the rule of four “NOT”):
- Do not check your breath with a mirror or feather - you waste time looking for it, the humidity outside may interfere with your breathing, and when using a feather, the wind can interfere with the reliability of the result. In such a situation, you will mistakenly consider the dead person to be alive.
Do not check the pupillary reflex - you need to be able to do this correctly and not with the help of a regular flashlight. If a person is alive, too bright light in certain diseases can damage the retina. Finally, there are neurological disorders in which this reflex will not work in a person with preserved vital functions.- You shouldn't do a precordial blow. This requires appropriate practice, moreover, this method has not been proven in terms of effectiveness, and in some cases it can cause even greater harm.
- Do not perform mechanical ventilation without protection (without a film valve) on strangers - there is a high risk of transmission of infection. If the chest does not rise during artificial ventilation, it should be assumed that air is passing into the stomach, or the airways are blocked. In the first case, limit yourself to NMS; in the second, clean your mouth or use the Heimlich maneuver.
Basics of cardiopulmonary resuscitation. Asphyxia, drowning, electrical trauma.
BASICS OF CARDIOPULMONARY RESUSCITATION
Cardiopulmonary resuscitation (CPR) is a set of emergency measures aimed at restoring the body’s vital functions and bringing it out of a state of clinical death.
Having discovered a victim while extinguishing a fire or eliminating an emergency, a firefighter or rescuer must first of all diagnose the person being rescued.
Determine whether the victim is unconscious:
- lies motionless;
- does not answer questions;
- does not respond to surrounding impulses (call, touch).
Next, it is necessary to take measures to assess the situation and ensure safe conditions for providing first aid:
- identify threatening factors for your own life and health and/or threatening factors for the life and health of the victim (exposed wires, spilled flammable or explosive liquids, parts of building structures threatening to fall, unbreathable atmosphere, unstable emergency vehicle, etc.);
- eliminate threats to life and health;
- stop the effect of damaging factors on the victim (move the victim to a safe place);
- Determine the presence of breathing using hearing, vision and touch: look for chest movements, listen to breathing sounds from the victim’s mouth, feel the exhaled air on your cheek for no more than 10 seconds;
- Determine the presence of blood circulation - checking the pulse in the main arteries for no more than 10 seconds.
Identify signs of biological death:
- clouding and drying of the cornea;
- the presence of a symptom of “cat’s eyes” - when the eye is compressed, the pupil is deformed and resembles a cat’s eye;
- coldness of the body and the appearance of cadaveric spots (blue-violet spots appear on the skin; when the corpse is positioned on the back, they appear in the area of the lumbar shoulder blades, buttocks, and when positioned on the stomach - on the face, neck, chest, abdomen);
- rigor mortis occurs 2 to 4 hours after death.
| Attention!!! | ||
| Determine the presence of a pulse in the carotid artery. (There is a pulse - the victim is alive.) | Listen to breathing, determine the presence or absence of chest movements. (There is movement of the chest - the victim is alive.) | Determine the reaction of the pupils to light by lifting the upper eyelid of both eyes. (The pupils narrow in the light - the victim is alive.) |
CARRYING OUT CARDIOPULMONARY RESUSCITATION
Measures to restore airway patency:
- place the victim on his back, without raising his head, on a flat, hard surface;
- throw back your head with a lift of the chin - one hand is placed on the forehead and gently tilts the head back, the fingertips of the other hand are placed under the chin or neck and gently pull up;
- push the lower jaw forward and upward - four fingers are placed behind the angle of the lower jaw and pressure is applied upward and forward, using the thumbs, the mouth is opened slightly by moving the chin slightly;
- It is strictly forbidden to throw back your head if you suspect a cervical spine injury.
| Attention!!! | |
| Ensure patency of the upper respiratory tract. Using gauze (handkerchief), remove mucus, blood, and other foreign objects from the mouth using a circular motion of your fingers. | Tilt the victim's head back. (Lift your chin while holding the cervical spine.) Do not perform if a fracture of the cervical spine is suspected! |
| Pinch the victim's nose with your thumb and forefinger. Using a device for artificial ventilation of the lungs of the “mouth-device-mouth” type, seal the oral cavity, make two maximum, smooth exhalations into his mouth. Allow two to three seconds for each passive exhalation of the victim. Check whether the victim’s chest rises when inhaling and falls when exhaling. |
Measures to carry out cardiopulmonary resuscitation until signs of life appear (in the absence of adequate breathing and pulse):
- perform indirect cardiac massage;
- perform artificial respiration “Mouth to mouth” or artificial respiration “Mouth to mouth”, “Mouth to nose” using an artificial respiration device;
- alternate a series of massage pushes with artificial breaths in the ratio of 30 pushes: 2 breaths .
It is necessary to continue chest compressions and artificial ventilation until the ambulance arrives or until the victim shows signs of life.
Giving the victim an optimal body position: when signs of life appear and there is no consciousness, transfer the victim to a lateral stable position.
Next, monitor the victim’s condition (consciousness, breathing, blood circulation).
Upon arrival, transfer the victim to the emergency medical team.
TECHNIQUE FOR CARDIOPULMONARY RESUSCITATION
Indications for cardiopulmonary resuscitation:
- presence of signs of clinical death (lack of breathing, carotid pulse, consciousness);
- agonal breathing (rare weak sighs or rare noisy labored breathing), manifests itself in the first few minutes after loss of consciousness during sudden cardiac arrest in adults.
IMPORTANT!:
- do not wait for adults to completely stop breathing; if there is any doubt, begin CPR;
- if there is any doubt about the presence of a pulse and there are no other signs of life (response to a call, spontaneous breathing, coughing or movement), begin cardiopulmonary resuscitation.
Method of performing indirect cardiac massage:
- the victim must lie on a flat, hard surface;
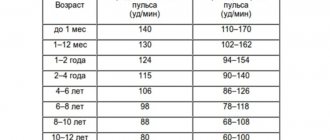
- hand placement point: for adults - in the center of the chest, 2 transverse processes above the base of the xiphoid sternum, for children under 1 year - 1 finger below the nipple line;
- press on the point with the heel of your palm, place your other hand on top, fingers of your palms pointing upward; for children under 1 year - two fingers;
- straighten your elbows, hang over the victim, apply pressure strictly vertically;
- perform 30 strong and fast rhythmic thrusts with a depth of pressure of 5-6 cm; for children under 1 year - by 3-4 cm or 1/3 of the diameter of the chest and with a frequency of compressions on the chest of 100 per minute;
- ensure that the chest is straightened after each compression to fill the heart with blood, ensuring that the duration of chest compression and decompression is approximately the same;
- Constantly adjust the pressure point;
- perform alternately if resuscitation is provided by 2 firefighters or rescuers (every 2 minutes or every 5 cycles of cardiopulmonary resuscitation, the firefighter or rescuer performing chest compressions must be changed; the change of firefighters / rescuers should not take more than 5 seconds).
Method of performing artificial lung ventilation:
- Use the index finger and thumb of one hand to pinch the victim’s nose, and support his chin with the fingers of the other hand;
- take a (shallow) breath, tightly wrapping your lips around the patient’s mouth (“kiss of life”), and exhale;
- keeping your head thrown back and your jaw extended, remove your lips so that air can passively escape from the victim’s respiratory tract;
- perform a second exhalation and return to chest compressions;
- carry out air injection for 1 s, observing the visible excursion of the chest. The exhalation should not be too large or sharp. The volume of blown air should be 500 - 600 ml;
- avoid exceeding the frequency, force or volume of air injections, but at the same time strive to perform artificial respiration as quickly as possible in order to minimize pauses in chest compressions;
- use barrier devices (face mask, respiratory protection devices for the resuscitator, air duct) that reduce the risk of disease transmission during mouth-to-mouth artificial respiration;
- in the first minutes, use protective devices that are at hand and allow you to avoid direct contact, for example a gauze mask;
- use a breathing bag (it is preferable for 2 people to work with the breathing bag: one presses the face mask and holds the patient’s airways open - throwing back the head, extending the jaw, the other compresses the bag, ventilating the patient’s lungs, thus achieving better sealing);
- For children under 1 year of age, artificial ventilation should be performed “mouth to nose and mouth.”
Criteria for stopping cardiopulmonary resuscitation:
- the appearance of independent pulse and breathing;
- transfer of the victim to an emergency medical team;
- a doctor's declaration of biological death;
- if resuscitation measures are ineffective within 30 minutes. (the skin does not turn pink, the pupil does not react to light, there is no pulsation of the carotid arteries in time with massage shocks).
Criteria for not performing cardiopulmonary resuscitation:
- the onset of clinical death due to incurable consequences of acute injury incompatible with life (by doctor’s decision);
- It is reliably known that death occurred more than 30 minutes. back (exception - drowning in cold water);
- presence of reliable signs of biological death.
| Attention!!! | |
| Determine the location of the xiphoid process, as shown in the figure. | Determine the point of compression two transverse fingers above the xiphoid process, strictly in the center of the vertical axis. |
| Place the heel of your palm on the compression point. | Apply compressions strictly vertically along the line connecting the sternum to the spine. Perform compressions smoothly, without sudden movements, using the weight of the upper half of your body. |
| - For infants, massage is performed using the palmar surfaces of the second and third fingers; - for teenagers - with the palm of one hand; - in adults, the emphasis is placed on the base of the palms, the thumb is directed towards the head (legs) of the victim. The fingers are raised and do not touch the chest. |
| Alternate two “breaths” of artificial pulmonary ventilation (ALV) with 30 pressures, regardless of the number of people performing resuscitation. | Monitor the pulse in the carotid artery, the reaction of the pupils to light (determining the effectiveness of resuscitation measures). |
ERRORS WHEN CARRYING OUT CARDIOPULMONARY RESUSCITATION
Errors during artificial ventilation (artificial respiration):
- complete patency of the airways is not ensured;
- tightness is not ensured when air is blown using the “mouth to mouth” or “mouth to nose” method;
- air enters the stomach, which leads to its distension, followed by vomiting (regurgitation);
- the sequence of air injection and pressure on the chest during external cardiac massage is disrupted (inspiration during pressure).
Mistakes when performing external cardiac massage:
- the victim is laid on a springy surface;
- the position of the hands of the person providing assistance differs from the “standard” one;
- when performing a cardiac massage, the arms are bent at the elbow joints or lifted from the victim’s sternum;
- Very sharp pressure is applied to the sternum, which can lead to fractures of the ribs or sternum with damage to the lungs and heart. If excessive pressure is placed on the xiphoid process of the sternum, ruptures of the stomach and liver are possible;
- the required frequency of pressure on the sternum is not provided (60 pressures per 1 minute is the minimum, 80-100 are optimal values) or rhythm (long breaks are allowed);
- there is no control over the effectiveness of the massage (checking the pulse every 2-3 minutes) and the ratio of the frequency of pressure on the sternum and air blowing (30:2).
Features of resuscitation in children:
- when performing artificial respiration on a child, it is necessary to blow air into the victim’s respiratory tract simultaneously through the mouth and nose, tightly covering them with the lips;
- exhale into the child’s airways less sharply than for an adult;
- Unlike adults, in whom artificial respiration is carried out at a frequency of 12 blows per 1 minute, when providing assistance to children under 2-3 years of age, 20 blows per 1 minute are performed, and at an older age - 15 blows per 1 minute;
- external cardiac massage should be carried out not with two, but with one hand, in infants (up to 1 year) - with the tips of two fingers, index and middle, with a frequency of 100-120 pressures per 1 minute. The point of application of pressure is 1 finger below the line connecting the nipples.
PROCEDURE FOR PROVIDING FIRST AID TO VICTIMS DURING OBTURATION OF THE UPPER RESPIRATORY TRACT BY A FOREIGN BODY (ASSHYXIA)
Asphyxia is oxygen starvation of the body and excess carbon dioxide in the blood and tissues, for example, when the airways are compressed from the outside (suffocation), their lumen is closed by edema, or pressure drops in the artificial atmosphere (or respiratory system).
The first step is to quickly diagnose the victim. Examination of the victim to determine the degree of airway obstruction:
- partial obstruction : paroxysmal cough, noisy breathing, hoarseness of voice (up to complete disappearance), signs of respiratory failure (bloating of the wings of the nose, retraction of intercostal spaces, bluish skin and visible mucous membranes), restless behavior of the victim;
- complete obstruction : cannot speak, breathe or cough, motor agitation, rapid onset of loss of consciousness, bluish face.
First aid for asphyxia
It is necessary to take measures to restore airway patency:
When providing assistance to a conscious victim:
- tilt the victim forward;
- apply 5 sharp blows with the heel of your palm between the shoulder blades;
- if the obstruction is not eliminated, perform five subdiaphragmatic thrusts (Heimlich maneuver);
- alternate five blows to the back with five subdiaphragmatic thrusts until the obstruction is eliminated.
Method of performing subdiaphragmatic thrusts (Heimlich maneuver):
- stand behind the victim, grab him around the waist, bend him slightly forward;
- clench one hand into a fist, place it below the sternum and above the victim’s navel;
- grab the clenched fist with your other hand;
- pull sharply and forcefully upward.
The mechanism for performing subdiaphragmatic thrusts (Heimlich maneuver) in a pregnant woman, an obese victim, victims with an abdominal wound:
- place your hands at the base of the sternum (directly above the attachment of the lower ribs);
- perform the technique with a quick push, pressing hard on the chest.
When providing assistance to an unconscious victim:
- place the victim on the floor in a supine position;
- clear the airways;
- place one hand with the heel of the palm between the navel and costal arches, place the second hand on top;
- using your body weight, press on the victim’s stomach in an upward direction towards the diaphragm; repeat several times until the airways are cleared;
- if there is no effect, follow the cardiopulmonary resuscitation algorithm.
| Attention!!! | |
| Place the baby on the forearm of your left hand, and clap the palm of your right hand 2-3 times between the shoulder blades. Turn the baby upside down and pick him up by the legs. | Grab the victim from behind with your hands and clasp them in a “lock” just above his navel, under the costal arch. Press sharply with force - with your hands folded into a “lock” - into the epigastric region. Repeat the series of pressures 3 times. For pregnant women, apply pressure to the lower parts of the chest. |
| If the victim is unconscious, sit on top of the hips and sharply press on the costal arches with both palms. Repeat the series of pressures 3 times. | Remove the foreign object with your fingers wrapped in a napkin or bandage. Before removing a foreign body from the mouth of a victim lying on his back, he must turn his head to the side. |
PROCEDURE FOR PROVIDING FIRST AID TO DROWNING VICTIMS
Drowning is a death or pathological condition resulting from immersion of the body in water or other liquids and bulk materials) and asphyxia.
All actions of a firefighter or rescuer always begin with the fastest but high-quality diagnosis of the victim.
Measures to examine the victim:
- determining the presence of breathing using hearing, vision and touch;
- determining the presence of blood circulation, checking the pulse in the main arteries.
Examination of the victim to determine the type of drowning:
True (blue) drowning caused by water entering the victim’s lungs:
- the victim's face and neck are blue-gray;
- copious pinkish foam is released from the mouth and nose;
- swollen neck vessels.
Spastic (pale) drowning - the access of air to the lungs is stopped due to spasm of the larynx:
- the skin of the victim is pale gray;
- little or no foaming from the mouth and nose.
Syncopal drowning . With this type of drowning, a reflex cessation of blood circulation occurs in victims caught in cold water:
- pale skin;
- independent breathing and blood circulation are absent.
First aid for drowning
Remove the victim to the shore or boat. Next, it is necessary to take measures to restore airway patency.
In case of true drowning:
- turn the drowned person over onto his stomach, create an angle between the chest and pelvis (bend him over the knee, place a support under his stomach, bend him over his arms or turn him face down, raise the pelvis 40 cm from the ground);
- induce a gag reflex by pressing your fingers on the root of the tongue;
- continue to perform this technique until the end of water discharge from the mouth;
- clean your mouth.
For spastic and syncope drowning:
- throw back your head with your chin up;
- extend the lower jaw;
- clean the oral cavity of foreign bodies.
| Attention!!! | |
| Make sure you are not in danger. Remove the victim from the water. (If you suspect a fracture of the spine, pull the victim out on a board or shield.) | Lay the victim on his stomach on your knee, let the water drain from the respiratory tract. Ensure patency of the upper respiratory tract. Clear the oral cavity of foreign objects (mucus, vomit, etc.). |
If there is no spontaneous breathing, immediately begin cardiopulmonary resuscitation measures:
- hand pressure on the victim’s sternum;
- mouth-to-mouth artificial respiration;
- mouth-to-nose artificial respiration;
- artificial respiration using an artificial respiration device.
Measures to maintain airway patency:
- giving a stable lateral position;
- insertion of an oropharyngeal airway.
Next, measures are taken to warm the victim, give the victim an optimal body position and monitor the victim’s condition (consciousness, breathing, blood circulation).
If pulmonary edema occurs (bubbling breathing, cough with foamy sputum):
- create an elevated torso position or a sitting position;
- lower your legs;
- apply venous tourniquets (tight bandaging) to the base of the thighs;
- inhale ethyl alcohol vapor.
Transfer the victim to the emergency medical team.
FIRST AID FOR ELECTRICAL INJURIES
Electric shock is one of the most dangerous domestic and industrial accidents and is always associated with high mortality. The effect of electric current on the human body leads to strong heating of tissues and the development of burns, as well as disruption of the functioning of internal organs.
First aid for an electric shock consists of stopping the effect of the electric current on the victim’s body, performing a closed heart massage and artificial respiration if the victim’s heart has stopped due to an electric shock, treating and applying a bandage to the burned areas.
Electrical injury usually occurs as a result of exposure of the tissues of the human body to high-power household electric current or a discharge of atmospheric electricity (lightning).
Sources of electric shock are:
- faulty electrical equipment in enterprises and household electrical appliances,
- broken wires of high-voltage lines,
- failure to comply with safety regulations when working with electrical equipment.
The degree of influence of electric current on the human body is determined by the voltage and current strength, the way the current passes through the body, the general health of the victim and how timely first aid was provided.
Features of electric shock and electrical injury
Electric current, when passing through the human body, causes tissue heating and can lead to electrical burns to the skin and damage to underlying tissues and organs.
Electrical burns occur where electrical current enters and exits and are called “current marks.”
Electrical burns may seem minor in appearance, but in fact they are often deep with significant damage to muscles, bones and internal organs.
Electric current can disrupt the functioning of the heart, even causing it to stop.
A victim of an electric shock may stop breathing.
Signs and symptoms of electrical shock:
- Finding an exposed source of electric current near the victim;
- The victim is unconscious;
- Obvious burns on the surface of the skin;
- Breathing problems with possible respiratory arrest;
- The pulse is weak, arrhythmic or absent;
- The entrance and exit holes of the electrical charge are usually located on the hands or feet.
Due to the nature of electrical trauma, even with short-term exposure to electric current, the victim may experience respiratory and cardiac arrest. Therefore, sufficiently effective first aid for electric shocks at the scene of an accident is often a decisive factor in saving the victim.
First aid for electric shock:
Assess the situation. Do not touch the victim immediately. He may still be under electrical current. If you touch the victim, you can get hit. If possible, you need to turn off the power source (unscrew the plugs, turn off the switch). If this is not possible, then move the current source away from yourself and the victim with a dry, non-conducting object (branch, wooden stick, etc.).
If it is necessary to pull the victim away from the electrical wire, we must remember that the human body through which the current has passed conducts the current in the same way as the electrical wire. Therefore, you should not touch open parts of the victim’s body with your bare hands; you can only touch dry parts of his clothing, and it is better to wear rubber gloves or wrap your hands in dry silk cloth.
| Attention!!! | |
| Ensure your safety. Put on dry gloves (rubber, wool, leather, etc.) and rubber boots. If possible, turn off the power source. When approaching the victim on the ground, walk in small steps, no more than 10 cm. | Remove the wire from the victim with a dry, non-conductive object (stick, plastic). Drag the victim by his clothes at least 10 meters from the point where the wire touches the ground or from live equipment. |
After the electric current ceases, it is necessary to pay attention to the presence of signs of life (breathing and pulse in large vessels).
In the absence of signs of breathing and pulse, urgent resuscitation measures are necessary: closed heart massage and artificial ventilation (artificial respiration). Inspect exposed areas of the victim's body. Always look for two burns (where electrical current enters and exits). Place a sterile or clean cloth over the burned areas. Do not use a blanket or towel for this purpose - fibers from them may stick to the burned surface. To improve the functioning of the heart, blood flow to it should be increased. To do this, lay the victim so that his chest is slightly lower than his legs.
All victims of electric shock should be hospitalized as quickly as possible.
Medical products that may be needed when providing first aid to victims :
- Isothermal rescue blanket.
- Sterile wipe.
- Glasses or eye protection.
- Non-sterile medical examination gloves.
- Oropharyngeal airway.
- Transport shield.
- Soft frameless medical stretcher.
- Vacuum stretchers.
- Devices for respiratory protection of the resuscitator.
- Face mask
- Breathing bag
Emergency assistance from the medical team: what is the algorithm of action?
To provide emergency care in case of sudden cardiac arrest, a special cardiology team arrives on site, whose task is to carry out advanced resuscitation measures and immediately transport the patient to the hospital. It works according to a protocol that includes the following sequence of actions:
- Checking vital signs and making a diagnosis. For this purpose, a wider arsenal of equipment is used, including an electrocardiograph. It is necessary to exclude other causes of clinical death, such as bleeding or blockage.
Resumption of conductivity of the upper respiratory tract. To ensure maximum oxygen supply, they are intubated.- Resuscitation measures are carried out according to the same algorithm as indicated above, but for mechanical ventilation they use breathing masks, an Ambu bag or a ventilator.
- In the presence of atrial fibrillation or ventricular fibrillation on the ECG, the question of using defibrillation is raised.
- Drug support is provided by intravenous or intracardiac administration of drugs such as Adrenaline (1 ml 0.1% in 19 ml NaCl 0.9%) and Cordarone (in the presence of arrhythmias, 300 mg IV).