Mitral valve plastic surgery is performed for pathologies of this part of the heart that cannot be cured with conservative methods. Reconstruction of the valve allows you to restore all its functions, prevent heart failure, and save the patient’s life. During the operation, plastic structures are used to completely rehabilitate the heart and avoid repeated problems with the valve. The procedure has its own characteristics, preparation and recovery rules.
Causes of development of mitral valve defects
The disease may be based on fundamentally different defects in the valve structures. To choose effective treatment tactics, it is important to accurately determine the form of the defect and the cause of its development.
- Valve leaflet defects often occur with infective endocarditis and myocarditis, and rheumatic heart disease. Perforated, loosely closing leaflets are not able to hold blood in the left ventricle during heart contractions. The blood is pumped back into the left atrium and then into the lungs.
- Fusion of valve leaflets . The most common cause of mitral stenosis is rheumatism (acute rheumatic fever); less commonly, this defect develops after infective endocarditis or heart injury. The calcified valves, welded together, impede the normal flow of oxygen-enriched blood into the left ventricle and further to the tissues and organs.
- Rupture of the chordae tendineae most often occurs in systemic connective tissue diseases and acute endocarditis. The valve leaflets move (prolapse) into the atrium, reducing the efficiency of the heart.
- Rupture or sclerosis of the papillary muscles is an acute, life-threatening condition that develops with infarction of the papillary muscles against the background of coronary heart disease (CHD) or heart tumors. When the papillary muscles are damaged, the valve leaflets lose their fixation point, and the valve completely stops functioning.
Contraindications for surgery
{banner_banstat1}
Heart valve replacement surgery is contraindicated for the following diseases and conditions:
- Acute myocardial infarction,
- Acute cerebrovascular accidents (stroke),
- Acute infectious diseases, fever,
- Exacerbations and worsening of chronic diseases (diabetes mellitus, bronchial asthma),
- Extremely severe heart failure with an ejection fraction of less than 20% with mitral stenosis, in which case the attending physician should decide whether a heart transplant is necessary.
Approaches to the treatment of mitral valve defects
The first step in treating clinically significant mitral valve disease is drug therapy. It includes drugs that slow down the heart and reduce the force of its contractions (beta blockers), antiplatelet agents and anticoagulants, antibacterial and anti-inflammatory drugs for infectious etiologies of the defect. Drug therapy improves the patient’s condition to a certain extent, but only high-quality surgical correction of the mitral valve can radically eliminate the cause of the disease.
Depending on the form of the defect, cardiac surgeons use one of the following procedures:
- Annuloplasty is the replacement or reconstruction of the support ring that surrounds the mitral valve and securely fixes it between the left atrium and the ventricle.
- Chordplasty – restoration of the integrity of damaged tendinous chords or their lengthening.
- Commissurotomy is the surgical separation of fused valve leaflets.
- Valve leaflet plastic surgery – correction of the shape, size or anatomical position of the valve leaflets.
- Prosthetics is the complete replacement of a damaged mitral valve with a biological or mechanical prosthesis.
According to the results of multicenter clinical studies and practical experience of leading cardiac surgery centers, preference is given to robotic surgery using the daVinci system and catheter surgical techniques.
daVinci Robotic Surgery - a combination of surgeon experience and robotic precision
Robotic surgery using the daVinci system allows you to successfully perform both reconstructive surgeries and complete mitral valve replacement. Such interventions combine the advantages of minimally invasive surgery and high precision of manipulation due to computer control of endoscopic instruments.
Patients receive a number of important benefits when using the daVinci robot:
- Shorter hospitalization period (up to 7 days).
- Short stay in the intensive care unit.
- Low risk of bleeding, no need for transfusion of blood and its components.
- Low risk of reactive postoperative pericarditis and pleurisy.
- Rapid restoration of physical activity (the next day after surgery, the patient can move around the clinic).
- Invisible postoperative scars measuring 1-2 cm, the chest is not opened.
The daVinci robot has over 20 years of experience. During this time, the system has undergone a number of modifications to improve the functional and aesthetic results of treatment. Modern cardiac surgery centers use the latest modification of the robot – da Vinci Xi®. To date, it is the only robotic device approved by the FDA for mitral valve surgery.
Relative limitations to the use of the daVinci system include the high cost of the equipment and the small number of qualified cardiac surgeons who are fluent in the technique of working with it. Also, endoscopic interventions are not performed in patients with pulmonary hypertension, aortic stenosis or insufficiency, severe liver dysfunction.
Due to the increase in life expectancy of the population and the improvement in the quality of medical care, an increasing number of people are reaching old age, and therefore the issues of providing them with effective medical care are becoming increasingly relevant. The leading place among diseases in elderly and senile people is occupied by diseases of the cardiovascular system [1, 3, 4, 16]. The main manifestations of physiological aging are associated with a limitation of the functional reserve of vital organs and systems, a decrease in the regenerative and adaptive capabilities of the body. In the elderly, concomitant diseases are much more common, affecting both the natural development of diseases of the cardiovascular system and the course of the postoperative period. Thus, back in the 70-80s of the 20th century, there was a tendency to abandon active surgical tactics in elderly patients in most clinics around the world; they tried to resort to it only in extreme cases [2, 3]. E. Nowicki et al. [15], having studied data from the England Cardiovascular Disease Registry for the period from 1990 to 1999, provide information that the average age of patients undergoing cardiac surgery increased from 64.7 years in 1990 to 67.0 years in 1999 d. At the same time, the most striking changes were observed in the group of patients over 80 years of age who underwent surgery on the mitral valve. Surgeries on 80-year-olds were performed extremely rarely in 1990, but by 1999 this group accounted for 12.4% of all patients with such interventions [15]. Progress in the field of anesthesiology, perfusionology, the development of more effective methods of protecting the myocardium and improved intraoperative monitoring make it possible to achieve results comparable to those in younger patients. Despite the increase in the number of heart surgeries in elderly and senile people, this cohort of patients remains a high-risk group in cardiac surgery. Most studies performed in recent years indicate a fairly large number of postoperative complications.
The purpose of the study was to evaluate the immediate results of mitral valve replacement in patients over 65 years of age.
Material and methods
For the period from 2000 to 2013, in the department of surgery of acquired heart defects of the Russian Scientific Center for Surgery named after. acad. B.V. Petrovsky Russian Academy of Medical Sciences, mitral valve replacement (MVR) was performed in 107 elderly patients (34 men, 73 women), which amounted to 8.9% of the total number of those operated on for mitral disease. The age of the patients ranged from 65 to 75 years (average 68.0±2.8 years). The duration of the medical history of the underlying disease ranged from 1 year to 65 years, on average 22.8±17.7 years. The duration of the medical history in patients with rheumatic defects was significantly longer than in patients with degenerative defects, exceeding the latter by 3.7 times.
69 (64.5%) patients had heart failure of functional class III and IV according to the NYHA classification. In the etiology of defects, the leading position was occupied by degenerative lesions - 65 (60.7%). Defects of rheumatic etiology were identified in 30 (28.1%) patients, ischemic mitral regurgitation - in 12 (11.2%). The absolute majority of patients had a concomitant pathology: one concomitant disease - in 99 (92.5%) patients, 2 or more diseases at the same time - in 71 (66.4%), 3 or more - in 34 (31.8%). The structure of concomitant pathology is presented in Table. 1
.
As part of the preoperative examination, all patients underwent a general clinical examination according to a standard protocol, which was supplemented by the use of instrumental methods, including selective coronary angiography. Transesophageal echocardiography was used intraoperatively to evaluate the results of surgical intervention.
All patients underwent MVP. The heart was accessed from a complete longitudinal median sternotomy. The heart-lung machine was connected according to the aorta-vena cava scheme. The main stage was carried out under conditions of pharmacocold cardioplegia and systemic hypothermia with cooling to 30-32 °C. Isolated MVP was performed in 57 (53.3%) cases, MVP in combination with tricuspid valve repair according to De Vega - in 38 (35.5%). Coronary artery bypass grafting was additionally performed in 12 (11.2%) patients, thrombectomy from the left atrium (see figure on color insert)
— 18 (16,8%).
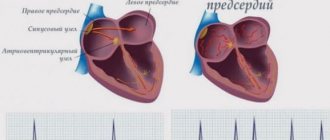
noted in 36 (33.6%) patients. The duration of artificial circulation was on average 97.2±31.2 minutes (from 50 to 236 minutes), aortic cross-clamping - 71.2±18.0 minutes (from 39 to 115 minutes).
results
The mortality rate was 2.8% (3 patients died). The causes of death were in 1 case - spontaneous rupture of the posterior wall of the left ventricle, in 2 cases - multiple organ failure due to complex rhythm disturbances resistant to drug therapy. Non-fatal complications were noted in most patients. Among the complications, the leading positions were occupied by cardiovascular failure, which necessitated the need for cardiotonic support for more than 72 hours - in 32 (29.9%) patients, disturbances of heart rhythm and conduction, which required temporary cardiac pacing for 1-7 days - in 27 ( 25.2%). In 6 cases, permanent pacemakers were implanted, 2 of them due to Frederick's syndrome identified in the preoperative period; in 3 cases the indication was postoperative complete transverse block with a heart rate <35 per minute, in 1 case it was a bradysystolic form of atrial fibrillation. Neurological disorders in the form of acute psychosis and postoperative delirium were noted in 12 (11.2%) patients. The structure of postoperative complications is presented in table. 2
.
The length of hospital stay after surgery averaged 14.4±3.5 days. In all cases where tricuspid valve repair was performed according to De Vega, its function, according to intraoperative transesophageal echocardiography, was found to be satisfactory. Regurgitation on the tricuspid valve did not exceed grade I.
Discussion
Global trends indicate an increase in the number of operations on the mitral valve in elderly and senile patients. This is due to an increase in the life expectancy of the population and, as a consequence, an increase in the population of people over 65 years of age, and an improvement in the material and technical support of medical institutions. In addition, many research works are devoted to the age characteristics of this group of patients. In the literature, studies in groups of patients over 70 and 80 years of age are increasingly found. However, surgery in this group is associated with a high risk of fatal and non-lethal complications [1, 3, 7]. Thus, according to a study by C. Akins et al. [5], mortality after mitral valve replacement was 12%. G. Ailawadi et al. [6] in a study of 117 patients over 75 years of age noted a mortality rate of 23.4%. However, according to many authors, mortality in isolated MVP ranged from 1.5 to 6.5% [8, 12]; short hospital stays and a low incidence of neurological complications have been reported [6, 10]. In studies of long-term survival, many authors have concluded that plastic surgery is more effective than prosthetics. V. Thourani et al. [17] in a study of 1250 patients over 65 years of age obtained a 10-year survival rate of 46% with mitral valve replacement versus 62% after mitral valve repair. A. Gogbashian et al. [11] in a study involving 292 patients over 70 years of age obtained a 5-year survival rate of 63% after prosthetics and 81% after plastic correction of the defect.
Our study did not include patients who underwent plastic surgery on the mitral valve, since the number of such patients was insufficient to conduct a comparative analysis. According to the literature, age itself is not a risk factor. Among the risk factors, the most frequently identified are a decrease in the left ventricular ejection fraction (less than 40%), the emergency nature of the intervention, renal failure, and a high functional class according to the NYHA classification, but their statistical significance has not been confirmed [7, 14, 17]. According to J. Nloga et al. [14], in a study of 129 patients over 80 years of age, the only statistically significant risk factor was the degenerative etiology of mitral valve disease (odds ratio 0.3 with a 95% confidence interval of 0.0 to 1.6; p
=0.01). In addition to the high incidence of complications, performing the surgical stage in this group of patients is associated with a number of technical difficulties. Thus, a decrease in the elastic properties of the vascular wall in combination with fibrosis and calcification increases the risk of developing spontaneous ruptures of the structures of the heart and great vessels. The risk of thromboembolism from atheromatous and calcium masses increases during aortic cannulation and after tissue decalcification. Severe calcification of the annulus fibrosus limits the surgeon's ability to perform decalcification; In elderly patients, in most cases, techniques are used to strengthen the surgical suture both when implanting a prosthesis and when sealing the cavities of the heart and great vessels. Left atrial thrombosis in the group of elderly patients with mitral valve disease is a common complication of the underlying disease. In our study, left atrial thrombosis was detected in 18 (16.8%) patients. According to the literature, factors contributing to thrombus formation in the left atrium include the predominance of stenosis in the pathophysiology of the defect in combination with atrial fibrillation. In our study, among 40 patients with group I and II mitral valve disease in combination with a permanent form of atrial fibrillation, left atrial thrombosis was detected in 18 (45%). Of these, 7 (6.5%) had a history of acute cerebrovascular accident of varying severity.
The need to perform thrombectomy, ligation and suturing of the left atrial appendage in order to prevent thrombosis increases the duration of artificial circulation. Severe osteoporosis of the sternum and the formation of fractures during retraction are another distinctive feature when performing surgical procedures in this group of patients. In the elderly, there is often a need for resternorrhaphy and reosteosynthesis of the sternum. In our study, sternal reosteosynthesis using the Robichek method was used in 8 (7.5%) patients. Involutive changes in the hemostasis system, increased permeability of the vascular wall, and a reduction in the cell population of the platelet link lead to more massive blood loss, a high rate of discharge through drains, and the formation of hematomas, including in the pericardial area. The combination of these factors increases the overall duration of surgical intervention and, of course, influences the course of the postoperative period and the development of complications.
Thus, performing surgical procedures in elderly and senile patients is associated not only with a high risk of developing lethal and non-lethal complications, but also with great technical difficulties. The results of recent studies of the natural history of mitral disease have shifted tactics in relation to elderly and senile patients from conservative tactics to the concept of early surgical intervention (before the development of signs of left ventricular dysfunction) [11, 16]. The concept of early surgical intervention is associated with long-term survival, a reduced risk of the need for re-intervention, and a reduction in the number of annual hospitalizations [9, 10, 12]. At the same time, life expectancy is comparable to the life expectancy of the population as a whole, and the quality of life of patients improves. We have demonstrated low mortality in patients with mitral valve replacement in this group. At the present stage, surgical treatment of mitral valve defects in patients over 65 years of age can achieve satisfactory results comparable to the results of surgical treatment of younger patients.
NeoChord – plastic surgery of chordae tendineae on a beating heart
The development of the NeoChord DS1000 system was the result of numerous clinical studies that demonstrated the superiority repair over complete replacement . NeoChord DS1000 has been successfully used for repair of chordae tendineae in patients with severe mitral regurgitation due to mitral valve prolapse.
The procedure is performed under general anesthesia, through a mini-thoracotomy access (incision length no more than 5-6 cm). In this case, the patient is not connected to a heart-lung machine; the heart maintains its natural rhythm.
Under strict visual guidance using 2D or 3D transesophageal echocardiography, the NeoChord DS1000 system is inserted into the left ventricle. The cardiac surgeon replaces the damaged chord with an artificial one and controls its tension. At the same time, the movement of the valve leaflets is reflected on the echocardiograph monitor in real time - this allows you to immediately evaluate the result of the operation and, if necessary, correct the position or tension of the chord.
To date, the NeoChord procedure has been successfully performed on more than 1,000 patients in Europe and the USA. The results of long-term postoperative follow-up confirm the safety of the technique and its effectiveness in the correction of mitral valve prolapse.
Indications and contraindications
Indications for the procedure are heart failure in combination with impaired valve function. Signs of such a problem are:
- swelling of the limbs. Most often the legs swell, but in some cases the same phenomenon occurs in the thighs, genitals, and abdomen;
- difficulty breathing. As a rule, this is shortness of breath, sometimes there may be a lack of air, pain when breathing in the chest area;
- pressing and throbbing pain in the chest;
- blue lips, gray skin color, “bruises” under the eyes;
- worsening of symptoms with physical activity.
Such signs indicate a developing disease; in the first stages, the problem may not manifest itself at all. Based on the patient’s complaints, the doctor prescribes several types of diagnostics, then clarifies the diagnosis. If a serious disorder in the mitral valve is confirmed, the type of surgical intervention is discussed.
Reconstruction of the heart is a difficult task, so it is carried out only if other methods do not help the patient. To prescribe plastic surgery, the attending doctor prescribes a series of examinations to the patient to ensure the need for such manipulations. For mild forms of the disease, drug treatment is most often used. Also, other types of therapy are sought if the patient has severe kidney and liver diseases, acute infections, pneumonia, gastric ulcers, diabetes mellitus, poor blood clotting, and sepsis.
Mitral repair is prohibited for people who have just suffered a stroke or extensive myocardial infarction.
If mitral repair is necessary, doctors weigh all the risks. Even against the background of some contraindications, surgery can be performed if it is intended to save the patient. Before prescribing this procedure, they must undergo training.
MitraClip – gentle one-stage reconstruction of the mitral valve leaflets
MitraClip technology is also used as part of the “Respect when you can, resect when you should” approach to cardiac surgery, which demonstrates the benefit of reconstructing a patient's native mitral valve over replacing it with an artificial prosthesis.
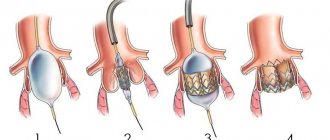
The MitraClip system allows you to firmly connect deformed or damaged valve leaflets using a microsurgical clamp made from an alloy of durable and metabolically inert metals - cobalt and chromium. During the procedure, the MitraClip is inserted into the femoral vein and moved into the left atrium under echocardiography guidance. This method of inserting a catheter into the heart does not require opening the chest and significantly reduces operational risks.
MitraClip securely fixes the valve leaflets in the required position, restoring normal blood flow from the left atrium to the ventricle. Using intraoperative echocardiography, the cardiac surgeon immediately assesses the quality of the reconstructed valve and, if necessary, installs an additional clamp.
Thanks to the successful results of clinical studies (European COAPT and EVEREST II studies), the MitraClip technique has been included in updated medical guidelines for the surgical treatment of mitral regurgitation. The MitraClip system is recommended for use in older patients with high surgical risks - such an operation is easier to tolerate compared to classic open cardiac surgery, but cannot fully replace complex reconstruction of the mitral valve.
Complications
{banner_banstat7}
The most serious complications after the introduction of a prosthesis are thromboembolic ones. Prevention of their development is lifelong antithrombotic therapy with the help of anticoagulants and antiplatelet agents - drugs that “thin” the blood. Such drugs include:
- Subcutaneous injections of heparin in the early postoperative period,
- Continuous use of warfarin under monthly monitoring of INR (international associated ratio) - an important indicator of the blood clot-forming system; normally it should be within 2.5 - 3.5,
- Constant use of aspirin (thromboAss, acecardol, aspirin Cardio, etc.).
No less dangerous consequences are the development or recurrence of infective endocarditis, the prevention of which is the rational prescription of antibiotics in the postoperative period, as well as their further use during any operations and minimally invasive interventions (tooth extraction, gynecological and urological manipulations, etc.).
Clinics and treatment costs
For successful minimally invasive mitral valve reconstruction, two main points are important: the availability of equipment and sufficient experience of the surgeon. Among the multidisciplinary and cardiology clinics that accept patients from all over the world, it is worth noting the following:
- University Hospital Oldenburg, Department of Cardiac Surgery
- University Hospital Essen, Department of Cardiothoracic Surgery
- University Hospital Ulm, Department of Cardiothoracic Surgery
- University Clinic named after. Goethe Frankfurt am Main, Department of Cardiothoracic Surgery
- University Hospital Tübingen, Department of Adult and Pediatric Cardiothoracic Surgery
The estimated cost of treatment is:
- Diagnosis of mitral valve insufficiency or prolapse – from €467
- Treatment of mitral valve insufficiency or prolapse with minimally invasive reconstruction – from €10,025
- Treatment of mitral valve insufficiency or prolapse using minimally invasive prosthetics – from €10,082
- Treatment of mitral valve insufficiency or prolapse using the Mitralign system – from €29,066
- Treatment of mitral valve insufficiency or prolapse using the Carillon system – from €27,326
- Cardiac rehabilitation – from €566
The exact cost of treatment can be determined after an initial consultation, assessment of the patient’s condition and selection of surgical technique. The cost of treatment is also affected by the presence of concomitant diseases and the need for rehabilitation after completion of the main course of treatment.
Send a request for treatment
Cost of the operation
{banner_banstat6}
In most cases, surgery to replace heart valves is performed free of charge, thanks to quotas from the Russian healthcare system under the compulsory medical insurance system. However, if for some reason it is not possible to obtain a quota, there is always the option of carrying out the operation at your own expense.
The cost of the operation itself, the prosthesis and rehabilitation in the early postoperative period ranges from 90 to 300 thousand rubles
, and the price is higher, the more complex the operation is, for example, the simultaneous replacement of the aortic valve and pulmonary valve is higher than one of them.
Heart valve replacement surgeries are carried out in all major cities of Russia, and now such interventions are not rare or inaccessible to the population.
Competent choice of clinic and cardiac surgeon is the basis for successful treatment
One of the keys to successful mitral valve surgery is a thorough preoperative examination and selection of an appropriate surgical technique. This is possible in a specialized cardiac surgery center or a large multidisciplinary university-level clinic, where doctors are not limited in equipment for carrying out innovative interventions. Most often, clinics in European countries with developed healthcare systems have such capabilities.
If you have chosen a prestigious foreign clinic, then you should take into account the specifics of registering for treatment for foreign patients - the need to receive an invitation from the clinic, preparation and translation of medical documentation, waiting for hospitalization for several months, paying for medical services at a higher rate, and so on. . To go through all stages of the medical program more comfortably and safely, you can use the services of Booking Health.
Booking Health is the only certified medical tourism operator in the world (ISO 9001:2015 certificate), which has been organizing treatment for patients from 75 countries in leading clinics in the world for more than 10 years. Booking Health specialists will help you with such important points:
- Choosing the right clinic based on the annual qualification profile
- Direct communication directly with the attending physician
- Preliminary preparation of a treatment program without repeating previously conducted examinations
- Ensuring favorable prices for clinic services, without surcharges and coefficients for foreign patients (savings up to 50%)
- Make an appointment for the desired date
- Control of the medical program at all stages
- Assistance in purchasing and shipping medications
- Communication with the clinic after completion of treatment
- Control of invoices and return of unspent funds
- Organization of additional examinations
- Service of the highest level: booking hotels, plane tickets, transfers
Leave a request with medical and contact information on the official Booking Health portal, and a competent consulting doctor or medical coordinator will contact you on the same day.