make an appointment with a doctor!
The umbilical cord is an organ that is quite simple in structure, but very important in significance. It plays a big role in ensuring the normal functioning of the baby during pregnancy. Accordingly, various anomalies and pathologies of its structure negatively affect the child’s condition and can lead to birth defects and even death. One of the problems that pregnant women face is a short umbilical cord in the fetus. This is a fairly serious pathology that can seriously complicate pregnancy and childbirth, up to its complete impossibility.
The umbilical cord and its role in childbirth
The umbilical cord is a hollow, flexible tube that connects the fetal abdominal wall to the placenta. Inside it lies:
- 1 vein, through which the baby receives blood enriched with oxygen and nutrients from the mother’s bloodstream;
- 2 arteries through which waste products of the fetus (urea, carbon dioxide, etc.) are discharged back;
- The vitelline duct connects the embryo's intestine to the yolk sac, which contains a supply of nutrients;
- The urachus is a duct that connects the fetal bladder to the placenta and serves to remove metabolic products.
The outer membrane (amnion) consists of strong connective tissue and protects blood vessels from damage. The space between it, the artery and veins is filled with Wharton's jelly - a jelly-like or mucous substance consisting of polysaccharides. It gives the umbilical cord elasticity and prevents it from twisting, thereby protecting the veins from the formation of kinks and mechanical damage.
Thus, the purpose of the umbilical cord is to provide nutrition, respiration and metabolism to the fetus during gestation. Since his own organs and systems are just being formed, their function is transferred to the mother’s body. During childbirth, the blood vessels in the umbilical cord, under the influence of the hormone oxytocin, “collapse,” gradually cutting off blood flow. This is how atrophy of the umbilical cord begins, which normally ends completely a few hours after the birth of the child. Under natural conditions, the umbilical cord dies and falls off on its own, but in the maternity hospital it is cut 1-3 minutes after birth. This allows you to minimize the risk of developing infection.
Take the first step
make an appointment with a doctor!
What is EAP, does such a diagnosis pose a danger to the fetus and the expectant mother?
Despite the fact that normally there should be 3 blood vessels in the umbilical cord, there are situations when a future woman in labor is diagnosed with a single artery in the umbilical cord. This syndrome in medicine is designated by the abbreviation “EAP” and is not a rare phenomenon. This pathology is detected in 0.5% of women carrying one child and 5% of patients diagnosed with multiple pregnancies.
Factors provoking the development of this anomaly:
- diabetes;
- multiple births;
- liver dysfunction;
- renal pathologies;
- disruptions in the functioning of the cardiovascular system;
- severe somatic and infectious pathologies of women in the first trimester of gestation;
- negative effects on the body of a future woman in labor of chemicals, medications, radiation;
- chromosomal disorders;
- bad habits during planning and bearing a child;
- living in unfavorable environmental conditions;
- harmful working conditions.
If a single vessel is formed, in the vast majority of situations this is not dangerous for the expectant mother and fetus. This means that one artery can cope even with high loads.
There may be cases when EAP is accompanied by other developmental abnormalities and genetic failures:
- chromosomal mutations;
- congenital cardiovascular diseases;
- diseases of the urinary system, abdominal and thoracic cavities.
When this phenomenon is detected, a comprehensive examination of the fetus is performed. This measure will eliminate the presence of concomitant diseases. The syndrome is not an indication for forced expulsion of the fetus from the uterine cavity. However, the combination of EAP with other abnormal phenomena serves as a reason for an induced abortion, because is fraught with the following consequences:
- freezing of the fetus;
- intrauterine development disorder;
- oxygen starvation of the child;
- protein-energy deficiency.
Short umbilical cord during pregnancy: causes and symptoms
Normally, the length of the umbilical cord in humans is 50-70 cm. This size reduces the likelihood of it twisting, which can cause hypoxia and nutritional deficiency in the fetus. However, quite often pregnant women experience disturbances in the length of the umbilical cord - in particular, its shortening. If the length of the organ is less than 50-40 cm, it is considered abnormally short. Depending on the causes of the pathology and the size of the umbilical cord, two types of anomalies are distinguished:
- Relatively short umbilical cord. It initially has a normal size, but during gestation it shortens due to twisting or entwining around the fetus, and the formation of varicose nodes on the organ. Most often this happens if the expectant mother eats poorly, drinks alcohol and drugs, smokes, experiences constant stress, or suffers from chronic systemic and gynecological diseases. This pathology poses a danger to the health and life of the child due to impaired blood circulation and accompanying hypoxia. However, a shortened umbilical cord can unravel on its own and therefore has a more favorable prognosis.
- Absolutely short umbilical cord. This is a genetic pathology associated with a violation of the mechanism of placenta formation. Factors contributing to this condition are hereditary diseases and chromosomal mutations. It occurs in most cases and also poses a great threat to the fetus. However, unlike the previous type of pathology, an absolutely short umbilical cord cannot be treated.
The danger of this pathological condition is that outwardly it does not show itself in any way. The expectant mother does not experience any inconvenience or pain; her life is not in danger. Very often, a woman finds out that she has an abnormally short umbilical cord during childbirth. Typical signs of this pathology:
- Increased labor time. For patients giving birth for the first time, they can last up to 20 hours, for those who have previously given birth again - up to 15 hours.
- Early delivery of the placenta. Normally, she is born within 20-50 minutes after the fetus leaves the woman’s birth canal. If the umbilical cord is too short, the child “pulls” it along with him, which is often accompanied by its separation and bleeding.
- Fetal hypoxia. This symptom is not direct evidence of an abnormally short length of the umbilical cord, since this condition is also observed in some other intrauterine pathologies. However, in combination with the above symptoms, fetal hypoxia may indicate a violation of the development or structure of the umbilical cord.
- Fetal hyperactivity. With acute hypoxia, the child begins to make vigorous movements. His heartbeat first increases to 160 beats per minute, then becomes slow (no more than 120 heartbeats). In addition, in the amniotic fluid, as a result of increased activity of the fetal intestine, meconium may appear - primary feces, consisting of bile, mucus, prenatal hair, and amniotic fluid digested by it.
Thus, the presence of a short umbilical cord in a fetus can be judged either by the fact of birth, or by using modern diagnostic tools that make it possible to track the condition of the baby during the prenatal period.
Take the first step
make an appointment with a doctor!
Umbilical cord diseases
There is a connection between the fetal place and the fetus through the umbilical cord or umbilical cord (funiculus umbilicalis), which normally consists of three vessels: one vein , through which blood saturated with oxygen and nutrients enters the fetus, and two arteries , through which venous blood returns from fetus to placenta.
In the early stages of embryonic development, the umbilical cord has two veins, but at 4 weeks of pregnancy the right umbilical vein becomes blocked and disappears by 7 weeks of pregnancy. In very rare cases, the left umbilical vein becomes obstructed, and the right one supplies the fetus with the necessary blood, while the development of the fetus is not impaired.
About 80% of the blood from the umbilical vein enters the fetal systemic circulation through a special ductus venosus, which drains into the inferior vena cava. The remaining 20% of the blood enters the portal (hepatic) circulation of the fetus.
The volume of blood flow in the umbilical cord increases with the duration of pregnancy - from 35 ml/min at 20 weeks to 240 ml/min at 40 weeks.
Types of pathological conditions of the umbilical cord
All disorders and pathological conditions of the umbilical cord can be divided into the following:
- pathological set of umbilical cord vessels
- short and long umbilical cord
- pathological torsion of the umbilical cord
- compression and blockage of the umbilical cord
- disruption of blood flow in the umbilical cord
- umbilical cord nodes
- umbilical cord hernia
- pathological attachment of the umbilical cord
- umbilical cord entanglement
- umbilical cord tumors
- damage (trauma) to the umbilical cord
- prolapse of the umbilical cord
Any deviation in the structure of the umbilical cord found on an ultrasound requires a detailed examination of the structure of all fetal organs, as it may be associated with other fetal malformations.
Single umbilical artery
In 1% of all pregnancies, instead of two arteries, the umbilical cord contains one, which in 75% of cases is an isolated deviation that does not affect the development of the fetus and ends in the birth of a healthy child. However, in 25% of cases, a single umbilical artery is associated with other abnormalities in fetal development, in particular the presence of defects of the heart, kidneys, intestines and skeletal system. Also, this type of umbilical cord pathology is more common with trimosomy 18 (Edwards syndrome).
If a single umbilical artery is detected, it is recommended to perform fetal karyotyping through chorionic villus sampling or amniotic fluid sampling, detailed anatomical ultrasound, and echocardiography. In the absence of other abnormalities in the development of the fetus, the prognosis and outcome of pregnancy are positive, as in cases of a healthy pregnancy.
Short or long umbilical cord
The normal size of the umbilical cord at the time of birth is 55-61 cm, although it may be slightly smaller or larger. Determining the true length of the fetal umbilical cord using ultrasound is not always possible due to the compact position of the fetus and its constant movements.
Leonardo da Vinci, who was not only a famous artist and mathematician, but also an excellent anatomist, argued that the length of the umbilical cord usually corresponds to the length of the fetus, and he was right. At 8 weeks of pregnancy, the umbilical cord is 0.5 cm long, at 20 weeks it is about 16-18 cm. The growth rate of the umbilical cord slows down after 28 weeks of pregnancy.
One of the first signs of a long umbilical cord is the presence of umbilical cord entanglements or umbilical cord knots. The average length of the umbilical cord when such abnormalities are detected is from 75 to 95 cm.
A short umbilical cord limits fetal movements and is often a secondary sign of fetal pathology (against the background of existing abnormalities in fetal development). The umbilical cord is considered short if its size is less than 32-40 cm at 38-40 weeks. This type of umbilical cord deviation is observed in 2% of births and placental examinations.
Most often, a short umbilical cord is accompanied by lesions of the fetal nervous system, skeletal dysplasia and other developmental defects, as well as inhibited mental development of children. The shorter the umbilical cord, the greater the risk of serious developmental defects in the fetus. When the umbilical cord length is less than 15 cm, malformations of the anterior wall of the abdomen, spine, and limbs are often found.
Natural childbirth with a short umbilical cord is impossible if the fetus is born with a head, and may be accompanied by placental abruption during childbirth, severe bleeding and other negative consequences of such childbirth complications.
Genetic factors (heredity) can play a role in the occurrence of a long umbilical cord, since it has been noted that such an umbilical cord can be observed in the same woman during subsequent pregnancies. The evidence that the longer the umbilical cord, the more active the fetus and the more active the child in the future, is contradictory and not confirmed by clinical studies.
While diagnosing a short umbilical cord is not usually difficult, there is no consensus among physicians regarding the diagnosis of a long umbilical cord. The standard minimum permissible maximum size of the umbilical cord has not yet been adopted - it fluctuates around 70-90 cm.
Measuring the length of the umbilical cord after a normal birth is not usually done, so most cases of long umbilical cord remain undiagnosed. After a pathological birth or the birth of children with developmental defects, the placenta is usually examined and attention is rarely paid to the size of the umbilical cord, except in cases where there is pathological torsion of the umbilical cord, umbilical cord nodes, or a single umbilical artery.
A long umbilical cord is often accompanied by intrauterine fetal hypoxia, fetal growth retardation, intrauterine fetal death, a large number of brain development abnormalities, neurological disorders, neurological development disorders in children and blood clotting disorders in newborns.
Pathological torsion of the umbilical cord
Normally, the umbilical cord vessels are evenly twisted counterclockwise to the left (like a serpentine) with a certain frequency of torsion from left to right (7: 1.4). The average number of twists of the umbilical arteries and veins along the entire length of the umbilical cord is 40. The umbilical cord twist index is the number of twists per 1 cm, which is normally 0.2.
Umbilical cord torsion appears early in pregnancy and can be detected on ultrasound at 9 weeks. The cause and mechanism of twisting is unknown, but it is thought to be related to the turning and movement of the fetus. The torsion index can characterize low or high fetal motility.
Also, twisting of the umbilical cord may be due to different growth rates of the umbilical cord vessels.
Changes in the direction of torsion do not affect the development of the fetus, but are more often accompanied by placenta previa and bleeding during pregnancy.
Absence of torsion or low torsion index is associated with chromosomal abnormalities, fetal malformations, fetal distress, and increased fetal and neonatal mortality. Increased twisting or pathological torsion of the umbilical cord is often accompanied by premature birth, death of the fetus and newborn due to asphyxia, as it can lead to disruption of blood flow in the umbilical cord, which in turn can result in thrombosis, rupture, dilation (coarctation) of the umbilical cord vessels. Pathological umbilical cord torsion is more often observed with long umbilical cords.
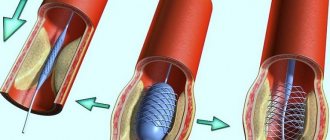
Compression and blockage of the umbilical cord
The umbilical cord is located outside the fetal body in the uterine cavity and is surrounded by amniotic fluid, and also has a specific structure: the vessels of the umbilical cord are covered with a membrane and have a layer of gelatinous mass, somewhat reminiscent of jelly ( Wharton's jelly ), a derivative of connective tissue. This not only improves the strength of the umbilical cord, making it hard to the touch (like rubber), but also protects it from being completely crushed. The fetus often compresses the umbilical cord, but due to the constant movement and turns, such compression is very short-lived. If the umbilical cord has pathological changes, any compression can lead to serious negative consequences, primarily blockage of the lumen of blood vessels and disruption of blood flow in the umbilical cord.
All causes of umbilical cord compression can be divided into external (fetus, large uterine tumor) and internal (structural abnormalities of the umbilical cord, nodes, torsion, hernia, umbilical cord tumors, etc.). If compression develops gradually and does not completely block the lumen of the vessels, a state of chronic obstruction (blockage) of blood flow occurs. The fetus may develop normally, but most often there is a delay in fetal growth.
Acute obstruction occurs more often closer to childbirth or during childbirth, especially with the presenting part - the nascent head or body of the fetus. It is observed in the presence of another pathology of the umbilical cord (true umbilical cord nodes). Acute compression of the umbilical cord can result in the formation of umbilical cord thrombosis and rupture. Compression of the umbilical cord during childbirth can lead to fetal hypoxia and asphyxia of the newborn, which will result in brain damage due to oxygen deprivation. Such children suffer from neurological diseases of varying degrees. The risk of fetal death during childbirth also increases.
Since the umbilical vein carries “fresh” blood from the placenta to the fetus, its compression is characterized by more serious complications than compression of the umbilical arteries. There is blood stagnation in the placenta, and anemia and hypoxia in the fetus.
Diagnosing umbilical cord compression using ultrasound is not easy, but studying the blood flow in the fetal vessels and its biophysical profile allows us to suspect fetal hypoxia and conduct a more thorough search for the cause of such disorders. Treatment of such a pathology will depend on the condition of the fetus, the duration of pregnancy and may involve more frequent monitoring of fetal development or urgent delivery.
Umbilical cord blood flow disturbance
Almost all pathological conditions of the umbilical cord can lead to disruption of blood flow in the umbilical vessels. Often, compression of blood vessels leads to the formation of a blood clot. Umbilical cord thrombosis is often detected after childbirth, especially pathological ones, when examining the placenta and umbilical cord. Often the presence of blood clots is accompanied by areas of umbilical cord calcification, which is associated with a number of infections (for example, syphilis).
Thrombosis of the umbilical cord vessels can also be due to a violation of the properties of the blood in a number of fetal cogulopathies, when the central nervous system of the fetus is damaged, when the processes of regulation of blood flow from the vessels of the fetus and the umbilical cord are disrupted.
Diagnosis of thrombosis of the umbilical vessels using ultrasound is difficult and cannot always be done before the birth of the child.
Umbilical cord knots
There are false and true umbilical cord nodes. False nodes are thickenings of the umbilical cord associated with the formation of a loop or expansion of the umbilical vein without blocking its lumen, therefore most doctors do not call them nodes. Sometimes this is a local varicose vein of the umbilical vein, but externally it may look like a real node. False nodes have no clinical significance and are completely safe for the fetus.
True umbilical cord nodes are found in 0.4-3% of births. They are accompanied by a high risk of morbidity in newborns (up to 11% of cases). True nodes may be tight, causing damage to the Wharton's jelly and umbilical cord vessels. At the site of the node, varicose veins of the umbilical vein may be observed, as well as the formation of blood clots not only in the umbilical cord, but also in the placental vessels. Most often, true nodes are observed with a long umbilical cord and its excessive twisting, polyhydramnios, and multiple pregnancies. Women with gestational diabetes are more likely to have true nodes. A connection has also been noted between the formation of true nodes and amniocentesis, which is explained by greater fetal mobility and uterine contractions during the procedure.
Diagnosing true nodes using ultrasound is difficult and most often they are discovered after childbirth. Doppler ultrasound can help study blood flow in the umbilical cord.
In most cases, true umbilical cord nodes do not complicate the course of pregnancy and their presence does not affect the growth and development of the fetus, as well as the outcome of pregnancy. If the node is tight and its diameter and the lumen of the umbilical cord are less than 1.5 cm, disturbances in blood flow in the great vessels of the fetus, fetal hypoxia and very rarely other complications in fetal development may be observed.
Since true nodes are often accompanied by polyhydramnios, the frequency of surgical interventions (cesarean sections) in such cases is higher.
Data on increased rates of stillbirth or neonatal mortality are conflicting and require clinical trials.
Umbilical cord hernia
The two most common abdominal wall defects are umbilical cord hernia and omphalocele. With an omphalocele , the umbilical ring is expanded and the internal organs of the fetus (intestines, spleen, liver, gall bladder), covered with amniotic membranes, can come out through it. In such cases, the attachment of the umbilical cord is not normal, but occurs outside the hernial sac.
Unlike omphalocele, with an umbilical cord hernia , its attachment is normal - in the area of the umbilical ring, while the skin and muscles that form and cover the ring are not damaged. In other words, it is an enlarged umbilical ring that resembles an adult umbilical hernia. While omphalocele is accompanied by a number of serious complications of pregnancy and often occurs with chromosomal abnormalities of the fetus, umbilical cord hernia is a very rare occurrence and most often occurs without harm to the fetus and newborn. In some cases, intestinal damage may occur. Diagnosis of an umbilical cord hernia is often accompanied by the fact that an omphalocele is mistakenly diagnosed and the woman is often offered to terminate the pregnancy. Therefore, it is important to carry out karyotyping of the fetus (in case of hernias, the child’s chromosome set is normal), as well as MRI for a detailed study of the structure of the umbilical ring and the relationship of organs at the site of the hernia. The prognosis for umbilical cord hernia is positive.
Pathological attachment of the umbilical cord
Normally, the umbilical cord is attached to the center of the placenta on the side of its fetal surface. In 7% of cases, attachment occurs along the edge of the placenta and such attachment is called marginal or marginal . In 1% of cases, the attachment of the umbilical cord occurs outside the fetal part of the placenta to the fetal membranes and such attachment is called velamentous or velamentous . Very rarely, there is a divergence of the umbilical cord vessels in the area of attachment and such an attachment is called furcated . Most often, pathological attachment of the umbilical cord is observed during multiple pregnancies.
The peculiarity of velamentous attachment of the umbilical cord is that in the area of attachment and formation of placental vessels there is no protective jelly-like mass (Wharton's jelly), which can be accompanied by compression of the umbilical cord, the formation of blood clots, rupture of the membranes, and umbilical cord injury.
The farther the umbilical cord is attached from the edge of the placenta, the more such attachment is accompanied by a high risk of vascular damage and serious pregnancy complications.
With vasa previa, the umbilical cord is attached to the internal os of the cervix and can be damaged during natural childbirth.
Bleeding due to rupture of umbilical cord vessels occurs in 1 in 50 cases of velamentous umbilical cord attachment, but is associated with a high rate of fetal death (two to three quarters of cases). With pathological attachment of the umbilical cord, fetuses are more likely to experience hypoxia, increased heart rate, developmental delay, intrauterine death, and newborns are more often diagnosed with low weight, thrombocytopenia, and other abnormalities associated with hypoxia and anemia.
Pathological attachment of the umbilical cord can be diagnosed in the early stages of pregnancy, but most often during an ultrasound scan in the second trimester, when the placenta is formed. However, in most cases, pathological attachment of the umbilical cord is discovered after birth when examining the birthplace.
There is no treatment for this malformation of the umbilical cord, but in some cases treatment of the fetus can be carried out (intrauterine blood transfusion for anemia and fetal hypoxia).
Childbirth requires good doctor skills and constant monitoring of the condition of the fetus. The incidence of operative delivery in cases of pathological umbilical cord attachment is higher due to fetal distress and hypoxia.
Umbilical cord entanglement
Entanglement of the umbilical cord, especially the fetal neck, is a common phenomenon that is found during ultrasound, starting from 10 weeks of pregnancy. It occurs in 15-20% of all pregnancies. In addition to the neck, the umbilical cord can wrap around other parts of the body, especially the limbs. Most often, entanglement occurs when there is a long umbilical cord.
The cause of umbilical cord entanglement is unknown, but a combination of a long umbilical cord and fetal twisting may be key to understanding how this condition occurs. More often, entanglement is observed with polyhydramnios.
The entanglement around the neck can be in the form of a simple loop and a loop with a “lock” (tied), and there can also be several loops (8 umbilical cord loops around the fetal neck have been recorded). The tighter the loop and the more loops, the worse the prognosis for pregnancy outcome.
Being entangled in the umbilical cord can cause compression of the umbilical cord and impede blood flow. This in turn can lead to fetal hypoxia and, in some cases, to its death. But in most cases, umbilical cord entanglement, which was discovered in the second trimester, is not found on ultrasound closer to birth. If there is an umbilical cord around the neck, the growth, development and condition of the fetus remains normal until the end of pregnancy, because the vast majority of loops are loose (not tight).
The danger most often arises during childbirth, when the noose may become tightened due to the baby moving through the birth canal. With tight entanglement, children are born with signs of hypoxia, and the rate of stillbirths is slightly higher compared to normal births. There is also a relationship between tight umbilical cord wrapping and a higher incidence of cerebral palsy.
Caesarean section is indicated only in cases of tight entanglement of the umbilical cord and signs of fetal hypoxia. In all other cases, its implementation should be rational, since the level of complications after surgery significantly exceeds the risk of a negative outcome in the presence of umbilical cord entanglement.
Umbilical cord tumors
Of all the tumor-like formations of the umbilical cord, the most common are hemangiomas, hematomas, aneurysms, and others less frequently.
hemangiomas are the same derivatives of blood vessels as body hemangiomas, and often their presence on the umbilical cord can be associated with the presence of hemangiomas in the fetus. Most often they are observed at the site of attachment of the umbilical cord to the placenta, also in the presence of polyhydramnios and fetal hydrops.
Hemangiomas are benign formations. Small tumors do not affect the development of the fetus and usually do not pose a risk to pregnancy. Large hemangiomas have a high risk of damage and bleeding. The size of some hemangiomas may be larger than the size of the fetal head.
Management of women with umbilical cord hemangiomas requires frequent ultrasound and monitoring of tumor growth. There is no cure for hemangiomas. For large hemangiomas, a cesarean section is performed.
Hematomas , unlike hemangiomas, are accompanied by a high level of fetal death and serious neurological damage to newborns in 50% of cases), since the fetus develops severe anemia. Hematomas appear as a result of an internal tear in one of the umbilical vessels and blood accumulates under the umbilical cord membrane.
Hematomas often occur with true umbilical cord nodes, as a result of trauma, with the membrane attachment of the umbilical cord.
This condition is diagnosed using ultrasound, but since the development of hematomas can be rapid, they are often discovered after childbirth. In most cases, the appearance of a hematoma, especially large ones, requires urgent delivery.
An aneurysm of the umbilical vessels has the same mechanism of occurrence as an aneurysm of the aorta or other vessels in humans - the elasticity of the vessel is impaired, the wall becomes thinner and its lumen expands. The most common aneurysm is the umbilical vein (which carries blood from the placenta to the fetus). Often, an aneurysm compresses adjacent vessels and can lead to thrombosis, rupture, and hematoma formation.
An aneurysm is combined with other pathologies of the umbilical cord - a single umbilical artery, pathological attachment of the umbilical cord, other abnormalities, and is associated with a high level of fetal hypoxia, its death, brain damage with the development of serious neurological diseases in the newborn, and therefore requires timely diagnosis, careful monitoring of the fetus and optimal delivery. Other types of tumors and tumor-like formations of the umbilical cord are very rare and are most often diagnosed after childbirth.
Umbilical cord injury
Invasive diagnostic tests and treatments that involve the insertion of instruments (fetoscope) and needles into the uterine cavity and gestational sac always carry the risk of damage to the umbilical cord and fetus, which can lead to hemorrhage, fetal death, and brain injury due to acute anemia and the development of neurological diseases in the child in the future.
Minor damage to the umbilical cord with a needle most often will not lead to a bad outcome, and in most cases of such injury, the fetal defenses try to “patch up” the damage site. Traces of such punctures of the umbilical cord and placenta in the form of scars and old hematomas (collections of blood) can be seen after childbirth. Also, amniotic fluid may have a wine color (usually a mixture of wine and water) due to the breakdown of red blood cells after bleeding.
Injury to the umbilical cord can also occur during childbirth, when medical staff tries to force the release of the placenta and strongly pulls on the umbilical cord. Usually, rupture of the umbilical cord in such cases is not dangerous for the newborn, since most often the umbilical cord is already tied.
Umbilical cord injury is also observed with pathological attachment of the umbilical cord due to the lack of a protective layer of jelly-like jelly. But in general, spontaneous umbilical cord injury is an extremely rare occurrence. Most often, umbilical cord damage is still associated with invasive procedures.
Umbilical cord prolapse
Prolapse or prolapse of the umbilical cord is characterized by the appearance of umbilical cord vessels in the birth canal in front of the adjacent part of the fetus and often occurs with premature rupture of the membranes, with artificial rupture of the membranes with forced loss of amniotic fluid, breech presentation, pathological attachment of the umbilical cord (vasa previa), with a long umbilical cord and less often in other cases.
Umbilical cord prolapse is always an emergency in obstetrics, because it is accompanied by a high risk of damage and acute massive bleeding, and therefore fetal death. Attempts to insert the umbilical cord into the uterine cavity, that is, to remove it from the birth canal, may result in damage to the umbilical cord. Therefore, an emergency caesarean section is most often performed.
Despite the different causes and mechanisms of development, various pathological conditions of the umbilical cord often occur in combination with each other, and therefore can complicate the outcome of pregnancy due to an increase in the total negative effect on the fetus and pregnancy as a whole. Fortunately, the incidence of such anomalies is very low and most often their presence is not accompanied by serious pregnancy complications.
Share link:
- Click to share on WhatsApp (Opens in new window)
- Click to share on Telegram (Opens in new window)
- Click here to share content on Facebook. (Opens in a new window)
- Click to share on Twitter (Opens in new window)
- Click to share on Skype (Opens in new window)
- Send this to a friend (Opens in new window)
- Click to print (Opens in new window)
By
Why is a short umbilical cord dangerous?
Both absolutely and relatively short umbilical cords are pathological anomalies that are potentially dangerous to the life and health of the child. The greatest damage is caused by chronic hypoxia, which develops due to insufficient oxygen supply to the tissues (including the brain). Its result is the death of the baby during pregnancy or childbirth, as well as congenital pathologies caused by the death of neurons in the brain or spinal cord. Also, a short umbilical cord during childbirth can cause the following complications:
- Slow movement of the child through the genital tract, which again causes hypoxia and too long compression of the skull bones, leading to death or developmental disorders;
- Placental abruption, which is accompanied by intrauterine bleeding, hemorrhagic shock due to large blood loss, disseminated intravascular coagulation syndrome, which simultaneously leads to the formation of blood clots and massive hemorrhages that threaten the life of both the fetus and the woman herself;
- Incorrect presentation of the fetus in the uterus, which can lead to various birth injuries - ruptures, sprains, etc.
Thus, the consequences that arise from a short umbilical cord concern not only the child himself, but also the mother. In severe cases, this pathology can lead to the loss of a newborn, infertility and death of the woman herself.
Take the first step
make an appointment with a doctor!
Umbilical cord research methods
Ultrasound will help detect abnormalities in the development of the umbilical cord - this is the main research method. Pregnant women are recommended to have an ultrasound scan during routine screening in each trimester.
Using ultrasound diagnostics, the doctor identifies:
- level of blood flow in the vessels;
- whether the fetus is wrapped in an umbilical cord (visible from the 15th week of pregnancy);
- fetal heart rate;
- how the cord is attached to the placenta;
- how the umbilical cord is attached to the abdominal wall of the unborn child;
- number of arteries and veins in the cord;
- are there any nodes?
- motor activity of the fetus.
Ultrasound allows the doctor to detect possible abnormalities in the development of the fetus, including those associated with umbilical cord abnormalities.
When there is reason to suspect umbilical cord abnormalities (slow or rapid heartbeat, signs of hypoxia), the doctor sends the patient for additional examinations, including:
- Dopplerometry is a type of ultrasound diagnostics that accurately determines the disturbance of blood flow in the vessels of the placenta and umbilical cord, as well as the degree of compression of the part of the baby’s body that is entwined with the umbilical cord;
- phonocardiography and auscultation - by listening to the sounds that arise during the work of internal organs, they reveal both defects in the work of the child’s heart and noise in the vessels of the umbilical cord, which is formed during entanglement;
Listening to the “inner world” of a pregnant woman using a phonendoscope will give the doctor additional information about possible disorders in the fetus - color mapping - allows you to see the umbilical vessels in detail;
- examination of the vagina - this is how prolapse of the umbilical cord is detected.
The method of treatment depends on what type of pathology the diagnosis reveals. If a loose umbilical cord entanglement or false knots on the cord are detected, the woman stays at home, but is regularly examined by a doctor. In more complex cases, the pregnant woman is placed in a hospital; when the fetus is diagnosed with severe hypoxia as a result of tight entanglement or the presence of true nodes on the umbilical cord, early delivery by cesarean is prescribed.
It happens that the unborn child is suspected of having chromosomal abnormalities; Then, to study the karyotype, umbilical cord blood is taken for analysis. The procedure is carried out under ultrasound control; the needle pierces the umbilical cord where it is attached to the placenta. Now in medical institutions they prefer to take a sample of amniotic fluid or the outer membrane of the fetus - chorionic villi - for analysis rather than blood.
Diagnosis of a short umbilical cord
As already mentioned, this pathology during pregnancy does not affect the condition of the woman herself, which significantly complicates its diagnosis. Often they find out about it only directly during childbirth, when complications begin. However, a short umbilical cord directly affects the condition of the fetus, and its changes can be recorded with modern diagnostic tools:
- Ultrasound. Ultrasound examination allows you to obtain a visual picture of the umbilical cord, from which you can judge the presence of knots and entanglements around the fetus. Unfortunately, this method does not accurately measure the length of the umbilical cord and, therefore, accurately diagnose the pathology.
- Ultrasound Doppler. Doppler ultrasound is a type of ultrasound, but it records the parameters of dynamic (moving) objects, while conventional ultrasound is used to study mainly static objects. This method is based on the fact that sound waves are reflected from moving objects with a change in frequency. Doppler ultrasound, in particular, allows one to determine the speed and direction of blood flow in the umbilical vessels. However, as in the previous case, these are only indirect signs that do not allow an accurate diagnosis to be made.
- CTG. One of the manifestations of a short umbilical cord in a child is hypoxia, which is accompanied by a reduction in his heart rate. To measure the fetal heart rate, cardiotocography is used, a type of Doppler ultrasound that records the heartbeat. In addition, this method also allows you to measure the frequency of uterine contractions. By synchronizing these two indicators, the doctor can judge the state of chronic fetal hypoxia and, therefore, the possible presence of a short umbilical cord.
- Gynecological examination. The standard of this procedure includes a visual examination of the cervix, which can be used to judge the position of the fetus, as well as an ultrasound scan, which monitors its heartbeat. Practice shows that gynecological examination quite often reveals indirect signs of a short umbilical cord.
The disadvantage of all of these methods for diagnosing a short umbilical cord is that they do not give an accurate result. However, by combining them with each other, the doctor can, with a fairly high degree of probability, make the correct diagnosis of a short umbilical cord.
Take the first step
make an appointment with a doctor!
What is the umbilical cord? What is its structure?
The umbilical cord (otherwise known as the umbilical cord) is a special formation that connects the fetus and the baby's place and allows for fetoplacental blood circulation. Outwardly, it resembles a spirally twisted bundle or cord and has a bluish-gray color. At the end of the third trimester, the umbilical cord reaches 50-60 cm in length, and its diameter at the umbilical ring is 1-2 cm. Although significant deviations from the average values in one direction or another can be observed. This is what the umbilical cord looks like. The photo demonstrates this.
One end of the umbilical cord is attached to the placenta, and the other to the baby in the area of the umbilical ring. It can be attached to the child's seat in different places, including in the center, on the side or on the edge. Rarely, the umbilical cord may attach to the membranes, some distance from the edge of the placenta. In this case, its vessels reach the child's place, passing between the membranes. Throughout its entire length, the umbilical cord has bends, depressions and bulges that arise due to its structural features. Normally, the umbilical cord has 3 vessels, two of them are umbilical arteries, and one is a thin-walled, wide-lumen umbilical vein. Nerve fibers are located along them. The nerves and vessels of the umbilical cord are surrounded by a special jelly-like connective tissue called Wharton's jelly. It performs a protective function, preventing compression of the arteries. The umbilical cord is covered on the outside with amnion, which, not reaching 0.5-1 cm from the navel, is transformed into the skin of the fetus.
Treatment of a short umbilical cord
There is currently no effective treatment for the pathology itself (both of its forms). If a short umbilical cord is suspected during pregnancy, the patient is hospitalized in a hospital for constant monitoring. Doctors use a wait-and-see approach, carefully monitoring the fetal heartbeat and mobility using ultrasound, ultrasound and CTG. The following are prescribed as maintenance therapy:
- Antispasmodics and mild sedatives that prevent vigorous fetal movements and umbilical cord twisting;
- Magnesium and iron preparations that improve oxygen supply to the blood and compensate for fetal hypoxia;
- Medicines that improve blood flow in the umbilical vessels.
Depending on the severity of the pathology, the predicted consequences of a short umbilical cord for the child and the woman herself, as well as the timing of detection, the following options are possible:
- Caesarean section - it is prescribed for a proven short umbilical cord and fetal hypoxia to prevent placental abruption and other complications during childbirth;
- Dissection of the perineum - this method is used to prevent fetal hypoxia in cases where a short umbilical cord is detected during natural birth.
A caesarean section can also be an emergency - for example, if bleeding, acute fetal hypoxia and other complications occur during natural childbirth with a short umbilical cord. In general, even with late detection of pathology, timely and correct use of CS allows to minimize the risks for both the woman and her child.
Take the first step
make an appointment with a doctor!
What to do if only 2 vessels are found in the umbilical cord?
There are situations when, instead of three arteries, the expectant mother has two blood vessels in the umbilical cord. This syndrome does not require specific treatment. The necessary measure in this situation is a full examination, including:
- detailed anatomical ultrasound examination;
- fetal karyotype analysis with sampling of chorionic villus or amniotic fluid;
- echocardiography.
If the antenatal development of the child does not have any abnormalities, the patient successfully carries the pregnancy to term under the constant supervision of the attending physician. A woman in such a situation is recommended to avoid stress, eat well, spend as much time in the fresh air as possible, and get enough sleep.
Prevention of a short umbilical cord
Since there is currently no effective treatment for this pathology, doctors recommend reducing the risk of its development even when planning pregnancy. If a woman cannot do anything about the hereditary physiological characteristics of her own body, then she is quite capable of the following actions:
- Avoid smoking, drinking alcohol and narcotic substances, which can cause disruption of the development of the placental apparatus;
- Prevent fetal hyperactivity by reducing the consumption of stimulating foods such as coffee, cocoa, chocolate, etc.;
- Be in the fresh air more often in order to maximally saturate your own blood with fresh oxygen, which will at least partially compensate for possible fetal hypoxia;
- Do not come into contact with toxic chemicals (varnishes, paints, industrial gases, etc.) during the period of preparation for pregnancy and gestation;
- Eliminate or minimize stressful situations - for example, changing jobs, leaving a dangerous urban area for a while, etc.;
- Make your diet more varied, rich in vitamins and other beneficial substances - especially iron and magnesium compounds, which will improve blood oxygen saturation;
- Avoid heavy physical activity and injuries, as they can lead to hyperdynamia of the fetus and the umbilical cord entwining around it.
Regularly scheduled medical examinations during pregnancy allow early diagnosis of possible pathology. If the expectant mother has relatives who were born with a short umbilical cord, or she herself had this anomaly, it is recommended to undergo examination by a geneticist.
If you suspect a short umbilical cord in the fetus, it is important to seek quality medical care. It can only be provided in licensed clinics staffed by qualified doctors. Also, the mother herself is required to completely trust the attending doctor and carefully follow his recommendations. You should not be afraid of such radical steps as a caesarean section - this is a long-established and simple operation that significantly reduces the likelihood of complications.