Pregnancy often involves many health risks for the mother and her unborn baby. One of the serious complications is Rh conflict and blood group conflict (ABO conflict). Such conditions can lead to slower fetal development and the appearance of hemolytic disease in the newborn.
Appointment with an obstetrician-gynecologist (doctor of the highest category) RUB 2,500.
Appointment with a hemostasiologist RUB 2,600.
All prices Make an appointment
The presence of such a problem can only be detected using certain tests. Self-diagnosis and treatment of the disorder is impossible. That is why you will definitely need the help of an experienced specialist.
You can seek help from our International Hemostasis Clinic in Moscow - we employ experienced gynecologists, candidates and doctors of medical sciences. We offer a competent approach to diagnosing possible pathologies and their treatment.
What is blood type conflict?
Blood type incompatibility or AB0 conflict occurs if mother and baby have different blood groups.
This can cause serious complications in the process of bearing a child, slowing down the formation of fetal organs and the appearance of hemolytic disease of the newborn. Incompatibility can only be detected after testing for group antibodies (hemolysins). From a school biology course, everyone knows that, despite the outward appearance, the blood of all people is different. It's all about the red blood cells, or more precisely, the antigens A and B located on their cell membrane. The blood plasma, in which the red blood cells are located, also contains α and β antibodies. There are four combinations of antibodies and antigens, each of which determines a person's blood type:
- a combination of α and β antibodies, without antigens – blood group 0 (I);
- combination of antigen A and antibody β – blood group A (II);
- combination of antigen B and antibody α – blood group B (III);
- a combination of antigens A and B, without antibodies - blood group AB (IV).
Only such combinations are possible, since antibodies and antigens of the same name (for example A and α) cannot be in human blood - when they come into contact with each other, they cause the death of red blood cells.
There is a persistent misconception that a child will necessarily inherit the blood type of one of the parents. In fact, a baby’s blood type can be absolutely anything. Even with extensive knowledge about the composition and characteristics of blood, one can only make assumptions as to whether the baby belongs to any group.
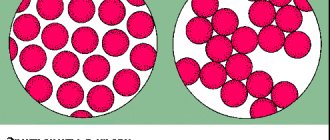
During a normal pregnancy, the likelihood of an AB0 conflict is minimal. Nature itself took care of this: due to the special structure of the placenta, the blood of the mother and fetus are reliably separated by the placental barrier. But even with a slight placental abruption, which at first glance does not pose a danger to the child, blood cells can mix, which leads to the appearance in the mother’s body of antibodies to the cells of the developing fetus. This is the conflict.
Rh factor inheritance
The birth of a child with a negative Rh factor in a family with Rh positive parents causes deep bewilderment at best, and mistrust at worst. Reproaches and doubts about the fidelity of the spouse. Oddly enough, there is nothing exceptional in this situation. There is a simple explanation for such a sensitive problem.
Rh factor
is a lipoprotein located on the membranes of red blood cells in 85% of people (they are considered Rh positive). If it is absent, they speak of Rh-negative blood. These indicators are denoted by the Latin letters Rh with a plus or minus sign, respectively. To study Rhesus, as a rule, one pair of genes is considered.
- A positive Rh factor is designated DD or Dd and is a dominant trait, while a negative Rh factor is dd, a recessive trait. In the union of people with heterozygous presence of Rh (Dd), their children will have positive Rh in 75% of cases and negative in the remaining 25%.
Parents: Dd x Dd. Children: DD, Dd, dd. Heterozygosity occurs as a result of the birth of an Rh-conflict child from an Rh-negative mother or can persist in genes for many generations.
In what cases does incompatibility occur?
An immunological conflict in the AB0 system can theoretically arise if the mother and baby have different blood groups, namely:
- the mother has group I or III, the child has group II;
- for the mother I or II, for the baby - III;
- the mother has group I, II or III, the child has group IV.
The most dangerous combination is group I in the mother and group II or III in the child. This situation will most likely lead to conflict and the development of hemolytic disease in the baby.
Group immunological conflict is possible in married couples with the following combinations of blood groups:
- woman with I, man with II, III or IV;
- woman with II, man with III or IV;
- woman with III, man with II or IV.
It is important to note that women with group I, regardless of the Rh factor, find it most difficult to achieve compatibility. The only optimal option is if the man and the fetus also have group I. If a man has a different group, the risk of developing an immunological conflict increases.
Women at risk include:
- received blood transfusions;
- have had several abortions or miscarriages;
- already having children with hemolytic disease or mental retardation.
Compatibility tests when planning pregnancy
It should be noted that the Rh factor does not affect the course of the first pregnancy, but it must be determined in order to protect the woman and give her a chance to give birth to a second and subsequent children.
Therefore, future parents need to find out the compatibility of their Rhesus in advance. To check blood compatibility, both spouses must undergo tests at the planning stage.
Women who are Rh negative and planning a pregnancy with a Rh positive man should have a blood test done to check for antibodies. You can donate blood for antibodies even if you are already pregnant. In the latter case, this should be done as early as possible in order to prevent miscarriage and fetal diseases.
Possible complications
Possible complications during pregnancy and after the birth of a child:
- development of hemolytic disease of the fetus with edema, jaundice of the skin, anemia, increased size of the liver and spleen;
- fetal hypoxia;
- thickening of the umbilical cord and placenta;
- disorders of the cardiovascular system in a child;
- delayed physical and mental development.
Without a doubt, blood type conflict is a rather dangerous phenomenon. But here it should be noted that Rh conflict can have more serious consequences for the child.
Rhesus conflict during pregnancy
In accordance with the definition, Rh immunization (Rh sensitization/Rh conflict) is the appearance of Rh antibodies in a pregnant woman in response to fetal erythrocyte antigens entering the bloodstream, i.e., to paraphrase more simply, this is the incompatibility of a mother with a Rh-negative blood group with a child who has Rh positive blood group (and not with my husband, as many people think).
Rh antigen is a protein found in the membrane of most people's red blood cells/erythrocytes. The blood of such people is Rh positive, and the blood of those who do not have this protein is called Rh negative. About 1/3 of the population is Rh negative.
Rh-positive parents may well have a Rh-negative child. In this case, a very peaceful, conflict-free relationship develops between the “positive” mother and her “negative” child: such a combination poses no threat to either the woman or the fetus.
If the mother and father of the child have a Rh negative blood group, the child also has a negative Rh factor.
But if the mother has Rh-negative blood and the father has positive blood, a Rh-positive fetus occurs in 60% of pregnant women, but incompatibility develops in only 1.5% of these pregnancies.
As a rule, with a second pregnancy the likelihood of incompatibility is higher than with the first.
The mechanism of development of Rh conflict
If Rh-positive red blood cells meet Rh-negative ones, they stick together - agglutination. To prevent this from happening, the immune system of a Rh-negative mother produces special proteins - antibodies, which combine with the Rh protein in the membrane of the fetal red blood cells (antigens), preventing them from sticking to the mother's own red blood cells. Antibodies are called immunoglobulins and come in two types: IgM and IgG.
Contact of fetal red blood cells with antibodies occurs in the space between the wall of the uterus and the placenta. When fetal Rh-positive red blood cells first encounter the immune system of the Rh-negative mother, IgM is produced, the size of which is too large to penetrate the placental barrier. That is why, as a rule, during the first pregnancy of an Rh-negative mother with an Rh-positive fetus, conflict arises relatively rarely. Incompatibility develops when fetal antigens (Rh positive red blood cells) re-enter the bloodstream of the Rh-negative mother, whose immune system in this case massively produces IgG, which, being smaller in size, penetrate the placenta and cause hemolysis, i.e. destruction of fetal red blood cells. This is how hemolytic disease of the fetus/newborn develops.
Complications of Rhesus conflict
As a result of the destruction of red blood cells, toxic damage occurs to almost all organs and systems of the fetus as a result of the breakdown of hemoglobin, a substance contained in red blood cells and responsible for oxygen transport. This occurs due to the breakdown product - bilirubin. First of all, the central nervous system of the fetus, liver, kidneys and heart are affected; fluid accumulates in its cavities and tissues, which interferes with the normal functioning of organs and systems, including intrauterine death in severe cases. It is in connection with this “rejection” of the fetus that Rh-negative mothers often develop the threat of miscarriage, and the risk of intrauterine fetal death increases.
Risk factors for Rhesus conflict
Divided into: 1. Pregnancy-related: - any type of termination of pregnancy: miscarriage, instrumental and medical abortions; - ectopic pregnancy; - childbirth, namely, in the third period, when the placenta separates from the wall of the uterus; - complication of pregnancy or childbirth - premature placental abruption, which is accompanied by bleeding from the vessels of the placenta; - any invasive research methods: (amniocentesis, cordocentesis - puncture of the amniotic sac or umbilical cord). 2. Unrelated to pregnancy: - immunization during blood transfusion; - using one needle for intravenous drug use.
Symptoms of Rh conflict
The patient has no clinical manifestations, her condition does not suffer.
Symptoms of hemolytic disease in the fetus during pregnancy can only be detected by ultrasound examination, they are: swelling, accumulation of fluid in the cavities (abdominal, thoracic, in the cavity of the pericardial sac); due to the accumulation of fluid in the abdominal cavity of the fetus, the size of the tummy increases, the fetus takes a certain position “Buddha pose” (when, unlike the norm, the limbs are removed from the enlarged tummy), an increase in the size of the liver and spleen, an increase in the size of the heart, a “double” contour appears heads (as a result of swelling of the soft tissues of the head). Also, swelling is determined and, accordingly, thickening of the placenta and an increase in the diameter of the umbilical cord vein. Depending on the predominance of one or another symptom, three forms of hemolytic disease of the fetus are distinguished: edematous, icteric and anemic.
Diagnosis of Rh conflict and pregnancy management tactics
The purpose of monitoring pregnant women during Rh immunization is: examination to identify sensitization, prophylaxis of Rh immunization, early diagnosis of hemolytic disease of the fetus and its correction, as well as determining the most optimal timing for delivery. When registering for pregnancy, it is necessary to determine the blood type of both the pregnant woman herself and the father of the child in a planned manner. If the mother has Rh-negative blood and the father has Rh-positive blood, pregnant women undergo a blood test for antibodies once a month, monitoring the dynamics of the antibody titer. In the presence of any antibody titer, the pregnancy is considered Rhesus sensitized. If antibodies are detected for the first time, their class is determined (IgM or IgG). Next, a blood test for antibodies is carried out monthly, observing the patient up to 20 weeks in the antenatal clinic, and after 20 weeks, they are sent to specialized centers to determine further management tactics, possibly carry out treatment and decide on the method and timing of delivery.
Starting from 18 weeks, the fetal condition is assessed using ultrasound.
Methods for assessing the condition of the fetus are divided into:
1. Non-invasive methods. — Ultrasound, which evaluates: the size of the fetal organs, the presence of free fluid in the cavities, the presence of swelling, the thickness of the placenta and the diameter of the umbilical cord vein. The first ultrasound is performed at 18-20 weeks, repeated at 24-26 weeks, 30-32 weeks, 34-36 and immediately before delivery. Depending on the severity of the fetal condition, this study may be performed more frequently, even daily (as, for example, after a blood transfusion to the fetus). - Doppler ultrasound, which evaluates the functional parameters of the heart, the speed of blood flow in the large vessels of the fetus and the umbilical cord, etc. — cardiotocography evaluates the reactivity of the fetal cardiovascular system, detects the presence or absence of hypoxia (lack of oxygen).
2. Invasive: - amniocentesis - puncture of the membranes for the purpose of collecting amniotic fluid to assess the severity of hemolysis by the content of bilirubin (a breakdown product of hemoglobin), which is one of the most accurate methods for assessing the severity of the fetal condition. Unfortunately, this method is fraught with many complications: infection, prenatal rupture of amniotic fluid, premature birth, bleeding, premature placental abruption. Indications for amniocentesis: antibody titer 1:16 or more, the patient has children who have suffered a severe form of hemolytic disease of the newborn. - cordocentesis - puncture of the umbilical cord to collect blood. The method allows you to accurately assess the severity of hemolysis and simultaneously perform an intrauterine blood transfusion to the fetus. In addition to those complications that are typical for amniocentesis, during cordocentesis it is also possible to develop an umbilical cord hematoma and bleeding from the puncture site. Indications for cordocentesis are the determination of signs of hemolytic disease of the fetus by ultrasound, antibody titer 1:32 or higher, the presence of children in the patient who have suffered severe a form of HDP in the past or those who died from it, a high level of bilirubin in the amniotic fluid obtained during amniocentesis.
Due to the possible risk, before performing either procedure, the patient must be informed by the doctor about the possibility of adverse consequences of the procedure and give her written consent to it.
Treatment of Rhesus conflict
In modern obstetrics, the only treatment method with proven effectiveness is intrauterine blood transfusion, which is performed for severe anemia (anemia) in the fetus. This type of treatment is carried out only in a hospital and can achieve a significant improvement in the condition of the fetus and reduce the risk of premature birth and the development of a severe form of the disease after birth.
Patients of a high risk group (whose antibody titer is detected in the early stages, those who have an antibody titer of 1:16 or higher, those whose previous pregnancy proceeded with Rhesus conflict) are observed in a antenatal clinic for up to 20 weeks, and then referred to specialized hospitals for the above treatment.
Various methods of purifying the mother's blood from antibodies (plasmapheresis, hemosorption), methods affecting the activity of the immune system (desensitizing therapy, immunoglobulin therapy, transplanting a skin flap from the child's father to the patient) are currently considered ineffective or even ineffective.
But, unfortunately, despite significant advances in the field of correcting the condition of the fetus, the most effective way is to stop the flow of maternal antibodies to it, which can only be achieved by delivery.
Delivery in case of Rhesus conflict
Unfortunately, with Rh sensitization, it is often necessary to deliver early, because in late pregnancy there is an increase in the number of antibodies that reach the fetus. Depending on the condition of the fetus and the duration of pregnancy, the method of delivery is individual in each individual case. It is believed that a caesarean section is more gentle on the fetus, and therefore in severe cases it is resorted to. If the condition of the fetus is satisfactory, the gestation period is over 36 weeks, in a multiparous woman it is possible to conduct labor through the natural birth canal with careful monitoring of the condition of the fetus and prevention of intrauterine hypoxia. If his condition worsens during labor, the management plan may be revised in favor of a cesarean section.
Prognosis for Rhesus conflict
The prognosis depends on how early Rhesus immunization was diagnosed, on the magnitude of the antibody titer and the rate of its increase, as well as on the form of hemolytic disease of the fetus. The earlier antibodies are detected in the mother’s blood, for example, at 8-10 weeks, the more prognostically unfavorable it is. A rapid increase in antibody titer, a titer above 1:16, and its early detection (less than 20 weeks) is the basis for an unfavorable prognosis. In such cases, not only the risk of hemolytic disease of the fetus increases, but also the risk of miscarriage.
The most prognostically unfavorable form of hemolytic disease of the fetus is edematous. Such children often require treatment in a pediatric intensive care unit and replacement blood transfusion. The most prognostically favorable form is the anemic form (depending on the severity of anemia). In the icteric form, the determining criterion is the level of bilirubin. The higher it is, the higher the possibility of damage to the central nervous system of the fetus, which later manifests itself as dementia and hearing loss.
Prevention of Rhesus conflict
Currently, human anti-Rhesus immunoglobulin D is used to prevent Rh sensitization. This drug has proven effectiveness and exists under several trade names, such as: “HyperRow C/D” (USA), Rezonativ (France), anti-Rhesus Immunoglobulin D (Russia ).
Prevention should be carried out during pregnancy at 28 weeks in the absence of antibodies in the mother’s blood, since it is during this period that the risk of contact of maternal antibodies with fetal red blood cells sharply increases, and therefore the risk of hemolytic disease of the fetus increases. Due to the administration of the drug, an antibody titer may appear in the blood, therefore, after administration of the drug, antibody determination is no longer carried out. Next, prophylaxis should be repeated within 72 hours after birth if the patient is planning a subsequent pregnancy. If bleeding occurs during pregnancy, as well as during cordo- or amniocentesis, as well as in the postpartum period, the administration of immunoglobulin should be repeated, because Rh sensitization may occur during the next pregnancy in response to fetal blood entering the mother’s bloodstream (during bleeding from the blood vessels of the placenta).
Also, prophylaxis should be carried out by injection of the drug for any outcome of pregnancy: miscarriage, medical or instrumental abortion, ectopic pregnancy, hydatidiform mole within 72 hours after termination. Particular attention is paid to blood loss, when it occurs, the dose of the drug should be increased.
Prevention
Recommendations for preventing the development of blood group conflict:
- try to avoid abortions, as this increases the likelihood of complications during subsequent pregnancies;
- observe preventive measures against infection with infectious diseases (flu, hepatitis), which weaken the body of the expectant mother;
- undergo routine examinations during pregnancy in a timely manner;
- Be careful when carrying a baby so as not to provoke placental abruption.
Modern medicine has many means to prevent the development of blood group conflict. The specialists of the Mother and Child clinics will do everything possible to maintain the health of the expectant mother and baby.
Inheritance of traits
For centuries, parents have only wondered what their child would be like. Today there is an opportunity to look into beauty far away. Thanks to ultrasound, you can find out the gender and some features of the anatomy and physiology of the baby.
Genetics allows us to determine the likely color of eyes and hair, and even whether a child has an ear for music. All these characteristics are inherited according to Mendelian laws and are divided into dominant and recessive. Brown eye color, hair with small curls and even the ability to curl the tongue are signs of dominance. Most likely, the child will inherit them.
Unfortunately, dominant signs also include a tendency to early baldness and graying, myopia and gaps between the front teeth.
Gray and blue eyes, straight hair, fair skin, and a mediocre ear for music are considered recessive. These signs are less likely to occur.
Ways to deal with incompatibility
If immune infertility is diagnosed, lymphocytoimmunotherapy can be performed, which is combined with taking hormones. The main goal of treatment is to change the mother's immune response to the embryo.
When antisperm bodies are detected, therapy involves sexual activity using barrier contraception for the time prescribed by the doctor. In parallel, immunotherapy with allergens is prescribed.
In case of genetic incompatibility, the use of ART is indicated.
How to check the compatibility of a couple?
Previously, a postcoital test was widely used to assess compatibility, which made it possible to detect the “sticking together” of sperm. However, it is characterized by a high degree of subjectivity. Therefore, it is not currently recommended as a diagnostic test.
A couple's compatibility assessment is carried out if, during regular sexual activity without contraception, pregnancy does not occur, and the standard examination protocol does not reveal any violations. In addition, a compatibility check is required if a woman has recurrent miscarriages or undeveloped pregnancies.
What can incompatible couples do?
The method of treating marital incompatibility depends on the established diagnosis.
- In case of immune infertility, lymphocyte immunotherapy can be performed, which allows changing the state of the mother's immune system in the direction of protecting the embryo. This treatment method can be combined with immune drugs or hormone therapy.
- In case of genetic infertility, it is recommended to use assisted reproduction methods, which make it possible to evaluate its chromosomal and gene set before embryo transfer in order to exclude the transmission of hereditary diseases.
- If there are antisperm antibodies, the couple is recommended to live with a condom for at least 1 month in order to reduce the level of sensitization in the male and female body. At the same time, desensitizing and immunosuppressive therapy is prescribed.
What is incompatibility of partners when conceiving a child?
From a scientific point of view, people started talking about the incompatibility of partners when conceiving a child relatively recently - approximately from the 50-60s of the last century, when a detailed study of the work of the immune system and genetics began. Some mechanisms have become clear that prevent pregnancy or contribute to its very early termination.
Incompatibility is considered to be any variant of pathological disorders (conflicts), most often of immune origin, that develop when the genetic material of a woman and a man meet. In the absence of such a “meeting,” the partners do not make any complaints. When talking about incompatibility, we are always talking about two people - a man and a woman. This condition has no specific manifestations.
Diagnosis and treatment of incompatibility
In case of severe genetic disorders, the body itself rejects the embryo with mutations, resulting in a frozen pregnancy or miscarriage. If this situation occurs a second time, the help of a geneticist is required. As part of the consultation, the following may be prescribed:
- expert spermogram;
- karyotyping;
- test for mutations in specific genes;
- FISH study of germ cells.
Unfortunately, the listed diagnostic methods do not always help identify the cause of incompatibility. In such cases, a detailed DNA test can be performed - an expensive but very effective way to determine the cause of infertility.