Several ways to determine blood type without laboratory tests.
Each person has a certain set of physiological indicators that distinguish him from other people and make him a unique individual. These include the color of hair, eyes, body type, certain characteristics of the body, such as metabolism, tendency to be overweight, etc., as well as weight and height. One of the most important features of the body is the blood type and Rh factor, which determine its basic properties.
But many young people and those who have never been hospitalized often do not have this information. If for some reason you do not want to go to a medical institution for testing, then after reading our article to the end, you will learn how to independently determine your blood type at home.
Image 1. Determine your blood type yourself.
Reference values
The result is given in the form:
- RHD+SEX;
- RHD+SEX with additional comment - “A weak Rh antigen has been detected. For blood transfusion, it is recommended to use Rh-negative red blood cells”;
- RHD-OTR.
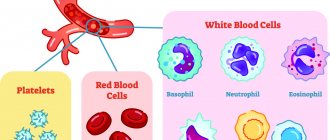
Erythrocytes (red blood cells) carry various proteins (antigens) on their surface. These antigens are inherited from parents.
About 236 erythrocyte antigens have been identified (most of them are rare). They are grouped into blood group systems. One of these systems, which is of great practical importance, is the Rh factor system. Among the Rh antigens, the most important is the D antigen (RhD). It is antigen D that is meant by the term Rh factor. Based on the presence or absence of the D antigen, people are divided into Rh-positive and Rh-negative.
Antigen D (Rh factor) has pronounced immunogenic properties (the ability to cause the formation of antibodies).
Rh conflict (mismatch of Rh affiliation between recipient and donor, mother and fetus) is the cause of hemolytic disease of newborns in 95% of cases, as well as a common cause of severe complications that occur after blood transfusion (post-transfusion complications).
When determining Rh status, several variants of the D antigen are distinguished, which can lead to difficulties in determining it.
Most often, the red blood cells of a Rh-positive person carry all types of D antigen ( normally expressed D antigen
).
Some people have normal types of antigen on their red blood cells, but their amount on the cell surface is reduced - this variant is called D weak
.
If red blood cells do not carry all types of D antigen (they differ qualitatively), then this option is designated as D variant
.
A blood test for Rh status is an important stage in the preoperative preparation of the patient, when there is a possibility that a donor blood transfusion (blood transfusion) will be required. If a person (recipient) with Rh-negative blood is transfused with Rh-positive blood, the recipient’s immune system will recognize this antigen as foreign and trigger the production of antibodies to it (as a rule, a small amount of antibodies is formed, but so-called memory cells (B-lymphocytes) remain) who remember antigen D). Upon repeated contact with foreign erythrocyte antigens, a large number of antibodies are immediately formed, and donor erythrocytes begin to be massively destroyed. This leads to post-transfusion complications - hemolytic anemia (a decrease in hemoglobin capable of carrying oxygen to tissues and organs due to the destruction of red blood cells), acute renal failure, jaundice, post-transfusion shock.
The second possible situation for the occurrence of an Rh conflict is pregnancy, when a Rh-negative mother (there is no D antigen on her red blood cells) is pregnant with a Rh-positive child (the Rh factor is present on the fetal red blood cells). In the later stages of pregnancy, fragments of Rh-positive erythrocytes of the fetus can penetrate into the mother's blood, where they will be perceived as a foreign antigen and cause an immune system reaction - the production of antibodies to the Rh factor. These antibodies, in turn, are able to penetrate the placenta into the child’s body and destroy its red blood cells. During the first Rh-positive pregnancy, the mother’s body usually does not have time to form a sufficiently large number of antibodies, and the fetus does not experience serious complications. However, subsequent Rh-positive fetuses may experience chronic breakdown of red blood cells. Usually, if a miscarriage does not occur, such children are born premature and suffer from anemia (anemia) and jaundice. This condition is called hemolytic disease of the newborn (hemolysis - destruction of red blood cells). It can lead to the death of a child.
Thus, early examination of the mother and fetus for Rh status helps prevent Rh conflict and the death of the newborn.
Sources:
- Mineeva N.V. Human blood groups. Fundamentals of immunohematology. - St. Petersburg. 2004. 188 p.
- Dutkevich I.G. Practical guide to clinical immunohematology (group antigens and antibodies of human blood, blood groups and their clinical significance, methods of immunohematological research). — St. Petersburg: SpetsLit, 2018. 159 p.
- Connie M. Westhoff. The Structure and Function of the Rh antigen Complex. Semin Hematol. January 2007; 44(1): 42–50.
- Pegoraro V, Urbinati D, Visser GHA, Di Renzo GC, Zipursky A, Stotler BA, et al. (2020) Hemolytic disease of the fetus and newborn due to Rh(D) incompatibility: A preventable disease that still produces significant morbidity and mortality in children. PLoS ONE 15(7): e0235807.
Will a compulsory medical insurance policy help you find out your blood type?
The plastic or paper policies themselves of all current samples do not provide for the presence of any medical information, including blood type. But under any of these policies, you must be served in any government medical institution throughout the Russian Federation, if they provide the services you need and are covered by the insurance.
The policy does not write the blood type anywhere, it only contains the full name, date of birth of the insured citizen and his gender. The document also contains its unique data in the form of a barcode and number. From the text on the card you can find out the name and telephone number of the compulsory medical insurance company that issued it, as well as the validity period of the insurance.
The place and form for indicating the blood type is provided in another document - in the passport. The stamp on pages 18 or 19 can be placed at a blood transfusion station or clinic. Group 0, A, B or AB, as well as Rh+ or Rh-, and below the name of the medical institution should be indicated there.
How is the research conducted?
To determine a blood group using cyclones, you need a flat, even surface (plate) moistened with water, a set of chemical reagents and biological fluid samples, and a specialist can use any blood: capillary, venous, frozen, etc.
- The sides of the tablet are marked so as not to confuse which of them will be applied to one or another type of zoliclones.
- One drop of reagents (usually anti-A and anti-B cyclones) and blood are dropped onto the surface, and the volume of chemicals should be 8-10 times greater than the volume of the biomaterial.
- Wait 3-5 minutes, gently rocking the plate so that the liquids are well mixed and red blood cells do not settle around the edges of the samples.
After a few minutes, a reaction will occur, by which it is possible to determine with high accuracy whether the blood belongs to a certain group.
What blood is most common?
The most common blood is the first group (or zero according to the AB0 classification). The second is a little less common.
The third and fourth are considered rare. The total percentage of their carriers in the world does not exceed 13–15.
The most common types (1 and 2) arose at the dawn of mankind. Their carriers are considered the most susceptible to allergies of various origins, autoimmune processes and other diseases. Blood of this type has changed little over hundreds of thousands of years, so it is considered the least adapted to modern conditions.
The percentage of blood types is also determined by the Rh factor. Positive is much more common than negative. Even 1 negative group, which is the leader among negative blood types, occurs in 7% of people.
The distribution of blood groups also depends on race. A person of the Mongoloid race will have Rh positive blood in 99% of cases, while for Europeans, Rh positive is about 85%.
Europeans are the most common carriers of group 1, Africans are carriers of group 2, and group 3 is the most common among Asians.
Blood types: percentage prevalence
As statistics show, different types of blood vary greatly in prevalence in the world. People with type 0 can be found without much difficulty, and type AB blood is unique in its own way.
The following table will help you finally understand which groups are the most common and which are much less common:
| Group and Rh factor | How common is |
| 0+ | 40% |
| 0- | 7% |
| A+ | 34% |
| A- | 6% |
| B+ | 8% |
| IN- | 1% |
| AB+ | 3% |
| AB- | 1% |
The ranking of blood groups in Russia is headed by the second, after it the most common is 3, and only then come groups 1 and 4.
What should you consider when conducting your analysis?
In order for the analysis result to be as reliable as possible, a number of conditions must be met during the procedure:
Advertising:
- reagents should be stored in a cool place at a temperature of +2-8 degrees in bottles with a tightly screwed cap (if storage rules are violated, they quickly lose their properties);
- For analysis, you cannot use cyclones that have expired (about 30 days) or liquids that contain sediment, flakes or debris;
- the study is performed in a well-lit room at an air temperature of no lower than +15 and no higher than +25 degrees, and there should be no dirt, dust or other factors that can distort the result;
- when applying biomaterial and reagents to the surface of the tablet, the proportions must be strictly observed - if there is too much blood, the reaction is more difficult to track, and in the opposite case (with a small volume) it will be too slow;
- Drops of blood mixed with different types of zoliclones should not be allowed to merge together - if this happens, the test is carried out again; for the same reason, different sticks should be used to mix reagents with biomaterial.
The reaction duration should be at least 3 minutes, and if the result is questionable, the observation time for biomaterial samples should be extended to 5 minutes. However, after 10 minutes, the biomaterial may dry out and red blood cells may naturally precipitate, so you should not trust such a study.
Rh factor
In addition to antigens A and B, many people also have the so-called Rh factor on the surface of their red blood cells. This is also an antigen that is shared by 85 percent of Europeans and 99 percent of Asians. Such people are called Rh positive or RH+
.
Those who do not have the Rh factor in their blood are called Rh negative or RH-
. If blood is transfused from a person with a negative Rh factor to a person with a positive Rh factor, no problems arise. Otherwise, Rh antibodies begin to be produced in the recipient’s blood, which lead to the destruction of red blood cells. Taking into account the presence of the Rh factor, a total of eight blood groups are obtained: 0 Rh+, 0Rh-, A Rh+, A Rh-, B Rh+, B Rh-, AB Rh+, AB Rh-.