An abnormal heart rhythm, or cardiac arrhythmia, occurs when the electrical impulses that initiate the heart's contraction do not function properly, causing the heart to beat too fast, too slow, or irregularly.
Arrhythmias are common and usually harmless. In most cases, a person feels a loss of one or more contractions, interruptions in the functioning of the heart - “it beats, then it doesn’t,” or a very rapid heartbeat. However, there are arrhythmias, the symptoms of which are dangerous, even life-threatening.
Advances in medical technology have enriched the physician with new therapeutic techniques and procedures that make it possible to control and eliminate arrhythmias. In addition, since arrhythmia can worsen, and in some cases, have a damaging effect on the heart (deplete the heart muscle, disrupt the functioning of the valve apparatus, cause an increase in the size of the cavities of the heart), the risk of arrhythmia can be reduced by adopting a healthy lifestyle, including proper nutrition and exercise.
Symptoms of arrhythmia
Arrhythmias may not appear. A doctor can detect an arrhythmia before it shows any signs during a routine clinical examination. But more often, heart rhythm disturbances cause noticeable changes in the condition, which include signs:
- Feeling of palpitations and chest pains
- Very fast heartbeat
- Extremely slow heartbeat
- Chest pain
- Shortness of breath
- Dizziness
- Loss of consciousness or feeling close to fainting
Even such significant symptoms of ill health do not always indicate a serious problem. Very often, people who experience an arrhythmia do not suffer from severe heart disease, while a person with a life-threatening arrhythmia may not have any complaints at all.
Normal heartbeat
The heart consists of 4 cavities. On each side, on the right and left, there are two pumps: on top of the atrium and below - the ventricles.
During cardiac contraction, chambers with a thin muscle layer and smaller sizes contract, helping to fill the relaxed ventricles with blood. Contraction begins when the sinus node—a small group of cells in the right atrium—sends an electrical impulse that causes both atria to contract. The impulse then travels to the atrioventricular node, located in the very center of the heart and lying at the junction of the atria and ventricles. Leaving the atrioventricular node, the impulse passes to the ventricles. As a result, the latter contract and push blood to all organs.
In a healthy heart, this process occurs evenly and constantly with a heart rate of 60-100 per minute in a calm state. In athletes, especially athletes at rest, the heart rate is usually less than 60, since their heart is much more trained than that of an ordinary person and has great muscle strength, pushing out a large volume of blood per contraction. In children, on the contrary, the pulse is normally more than 100 beats per minute, and in infancy it is 140-160 beats per minute.
How to treat paroxysmal supraventricular tachycardia
There are several treatment options at the FMBA center. Depending on the severity of the illness, the attending physician may place you in the therapeutic department. You will be under the constant supervision of professionals and receive timely medical care. This is usually drug therapy. If the symptoms of standard therapy are not enough, then you may be offered catheter ablation of the arrhythmia. At the same time, by puncture access under local anesthesia, under X-ray control using a catheter, an accurate diagnosis of the source of arrhythmia is made and, by precisely influencing it with a radiofrequency pulse or cold, the cause of paroxysmal tachycardia is eliminated.
Causes of arrhythmia
The most common causes of arrhythmia or the condition leading to its development are heart disease, high blood pressure, diabetes, smoking, excessive consumption of alcohol and caffeine, drug abuse, and stress. In some cases, the causes of arrhythmias may be an overdose of certain medications, the use of dietary supplements and herbal preparations.
Scars can occur for various reasons. The most common of these is acute myocardial infarction. Such a scar prevents the formation of an electrical impulse and/or interrupts the passage of an impulse through the heart muscle.
In a healthy person with a healthy heart, the development of a stable arrhythmia is impossible without the presence of an external trigger, such as an electric shock. This happens primarily because in a healthy heart there are no pathological substrates for the development of arrhythmias, including scar tissue.
On the other hand, in hearts with signs of arrhythmia, the formation and/or propagation of the electrical impulse may be impaired, facilitating the development of the disease.
Any of the following conditions can lead to the development of arrhythmia:
○ Inadequate blood supply
. If blood flow to the heart is reduced for any reason, this can alter the cells' ability to form and conduct electrical impulses.
○ Damage or death of the heart muscle
. Damage or death of the heart muscle leads to a change in the path of electrical impulses propagating through it.
Among the heart disease causes of arrhythmias, the following are of particular importance:
○
Coronary heart disease (CHD)
. Despite the fact that many types of arrhythmias are recorded with ischemic heart disease, the most strongly associated with it are ventricular arrhythmias and sudden cardiac death. The narrowing of the arteries occurs until, as a result of lack of blood supply, part of the heart muscle dies (acute myocardial infarction). This can affect the process of propagation of an electrical impulse throughout the myocardium: small electrical circles of excitation are formed at the border of scar tissue, which disrupt the normal functioning of the heart, causing pathologically fast heartbeat (ventricular tachycardia) and ventricular flutter or fibrillation - ineffective chaotic contractions of the ventricles.
○ Cardiomyopathy
. It manifests itself as primary stretching and thinning of the walls of the ventricles and atria (dilated cardiomyopathy) or excessive thickening and overcontraction of the walls of the left ventricle (hypertrophic cardiomyopathy). With any variant of cardiomyopathy, the efficiency of cardiac output decreases (the amount of blood ejected by the left ventricle into the aorta to nourish all organs and tissues of the body decreases), and part of the blood remains in the left and right ventricles or is thrown back into the atria and the veins flowing into them.
Heart valve diseases. Damage to the heart valves by infectious agents or due to degenerative degeneration leads to narrowing of the valve openings and/or insufficient closure of the valves, i.e. valve insufficiency. When the chambers of the heart become stretched and weakened due to inadequate valve function, the risk of developing various types of heart rhythm disorders increases.
Tactics for managing patients with supraventricular tachyarrhythmias
Oksana Mikhailovna Drapkina , professor, doctor of medical sciences:
– Next lecture – Professor Olga Nikolaevna Miller, “Tactics for managing patients with supraventricular tachyarrhythmias.”
Olga Nikolaevna Miller , Doctor of Medical Sciences, Professor:
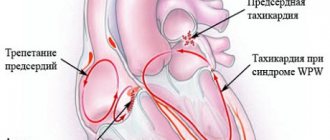
– Good afternoon, dear colleagues! We're really going to talk about supraventricular tachyarrhythmias today. And first of all, I want to present this clinical electrocardiographic classification, according to which, in fact, we, all cardiologists-arrhythmologists, have been working since 2006. It has been changed somewhat, indeed, since 2006, and you see that the so-called sinoatrial reentry tachycardia (or re-entry tachycardia) is distinguished. The group of cardiac arrhythmias of atrial origin has decreased slightly - you see, only two types of cardiac arrhythmias are left in brackets: focal and multifocal, or, as we also call it, chaotic atrial tachycardia. A very large group of atrioventricular tachycardias, which includes AV nodal reciprocal tachycardia, associated with the presence of additional conduction pathways. And, undoubtedly, what is very widely discussed today are two heart rhythm disorders, in particular of supraventricular origin: atrial fibrillation and atrial flutter. We will not discuss them today, but, indeed, the whole world is discussing this problem, and not only “how to treat?”, “how to stop?”, “how to prevent?”, but also very widely discusses antithrombotic therapy.
So we'll start with stopping and, of course, talking about preventing these supraventricular tachyarrhythmias. And first: if we have a patient with reciprocal tachycardia, that is, if it is supraventricular tachycardia caused by the re-entry mechanism, then there is no problem stopping it using transesophageal pacing. Of course, endocardial can also be used, but this is mainly carried out in arrhythmology departments during surgical interventions, for example, during radiofrequency ablation surgery. Basically, in all hospitals, at least those who know these techniques, perform transesophageal cupping. You can use it as reducing, competing, increasing or ultra-fast cardiac pacing. And in these two fragments you see how sinus rhythm is restored with a volley of impulses, where there is an effect on the AV nodal tachycardia on the top film, and below is orthodromic tachycardia, again a volley of impulses, restoration of sinus rhythm. And you see perfectly well that in the sinus rhythm there are signs of pre-excitation, pre-excitation, that is, a short PQ interval, a delta wave and a somewhat widened QRS complex.
Let's see: if it is not possible to stop tachycardia, how should we treat it if we really made the diagnosis correctly? So, sinoatrial reciprocal tachycardia. It is clear that it is caused by the re-entry mechanism, and therefore the first thing you can do is to use vagal maneuvers. You can use anything: squatting, inducing a gag reflex, Valsalva maneuver, that is, a breath-hold test. The best thing, of course, is carotid sinus massage. I remind you that the Aschner maneuver or Aschner test is prohibited today; this pressure on the eyeballs is not recommended for restoring sinus rhythm.
You can use ATP. I won’t talk about Adenosine, because Adenosine has never been on the pharmaceutical market of the Russian Federation, but ATP can be administered in a dose of 10-20 milligrams. It is administered very quickly, as a bolus, as it is written. But bolus is sometimes a loose concept. Let me just remind you that ATP is indeed injected very quickly, within 1-2 seconds, and without dilution.
You can use Verapamil. Its dose can be 5 or 10 milligrams, it is administered no faster than 2 minutes, so as not to cause severe hypotension during the administration of this drug.
The following medications may be used: Digoxin, beta blockers, Amiodarone are listed here. Digoxin has an advantage in older people. Of course, we understand that Digoxin does not belong to antiarrhythmic drugs if we take into account the Williams classification, but, nevertheless, sometimes Digoxin helps in stopping supraventricular tachyarrhythmias. I am not talking, I repeat once again, about atrial fibrillation and atrial flutter.
If your patient with sinoatrial reciprocal tachycardia has hemodynamic disturbances, then, of course, electrical cardioversion is performed. And I would like to draw your attention to the fact that the discharge power during electrical cardioversion should be small. At least 50 joules is enough to restore sinus rhythm.
And, of course, as I have already shown, electrical cardiac stimulation, which in 100% of cases stops reciprocal tachycardia.
The second question is how to warn? And you see the first phrase that there have been no controlled studies on the prevention of sinus reentrant tachycardia. In general, of course, if antiarrhythmic therapy is hemodynamically poorly tolerated or ineffective, catheter ablation should be performed. But here surgeons must work very delicately, very carefully, because if they act powerfully on the sinoatrial zone, they can damage the sinus node, and then the second point of surgical intervention is the implantation of a pacemaker.
You can use medications, that is, tablets, to prevent episodes of sinus reciprocal tachycardia. This is Verapamil, a beta blocker, just please titrate the dose to the maximum tolerated. In older patients, you can use Digoxin, and also, but only as a last resort, you can use Amiodarone or Sotalol. I repeat once again - in tablets. Why amiodarone last? Because Amiodarone, we have talked about this many times, has a very high organotoxic effect.
The second thing that was presented on the electrocardiographic classification of supraventricular tachyarrhythmia is focal atrial tachycardia. And we must also understand that this is a focus that is located in the conduction system or in the atrial myocardium. Focal atrial tachycardia is not relieved by ATP, is not relieved by vagal maneuvers, and is not treatable by pacing.
If your patient has stable hemodynamics, then in this situation, please reduce the heart rate. What can you use? You can use Verapamil or Diltiazem, as well as beta-blockers.
It has been shown in some studies that drugs of the first A class have a good relief effect, but we are talking about relief. Of the first class A drugs on the pharmaceutical market of the Russian Federation, the only drug is Novocainomide, although you can also use it. The first C class is a good drug, Propafenone, but, unfortunately, we do not have it in injection form. You can try a third class drug - Cordarone.
If your patient has a low ejection fraction or there are clear signs of worsening heart failure, then in no case should you intervene with drugs of the first A, first C class.
And again, in case of hemodynamic disturbances - electrical cardioversion, and the discharge power - I emphasize again - is low, not 360 joules, but only 50-100 joules are enough to restore sinus rhythm.
How to warn? Try to start preventing this atrial tachycardia with beta-blockers, but I repeat once again - do not stop at a fixed dose. Titrate and select this dose of beta-blockers specifically for each patient. If there is no effect, use drugs of the fourth class of antiarrhythmics. And if both groups of drugs do not help, then you can use Amiodarone and Sotalol. Even if these medications do not help and it is not currently possible, for example, to perform radiofrequency ablation of this ectopic lesion, then you can try a combination of medications. In particular, what drugs are welcome? These are drugs of the first A or first C class in combination with beta-blockers or calcium channel blockers, that is, with Verapamil.
As a matter of fact, if we take this algorithm for preventive therapy for focal atrial tachycardia, then a therapist or cardiologist has a lot of options.
But multifocal atrial tachycardia - unfortunately, you see the first line: it says that treatment of the underlying disease is important. Yes, we really understand that the cause of multifocal atrial tachycardia is most often COPD with exacerbations, the same bronchial asthma, multifocal tachycardia can occur in long-term febrile patients, in patients with a severe functional class of chronic heart failure and with severe diabetes mellitus.
And therefore, of course, we will first of all focus on reducing the heart rate. And for this purpose, you can use Verapamil or beta blockers, but it is clear that the latter are contraindicated due to exacerbation of COPD.
It is possible to use Amiodarone, but remember also that when Amiodarone is administered, broncho-obstructive syndrome may develop in patients with COPD.
Cases of successful restoration of rhythm with the help of magnesium sulfate have been described, that is, when you administer a 25% solution of magnesium sulfate in a dose of 2 grams, which is 8-10 milliliters of this drug, and no faster than 3-5 minutes, you can restore sinus rhythm. You can repeat exactly the same dose after 5-10 minutes.
It is written further: drugs of the first C class are effective, in particular Propafenone. But, once again, due to the lack of an injection form, we cannot use this drug today.
But electrical pulse therapy or electrical cardioversion, electrical pacing for multifocal atrial tachycardia is ineffective. There are many ectopic foci, and therefore once again I draw attention to the first line - the treatment of the underlying disease occupies an important place.
AV nodal reciprocal tachycardia. Previously, it was believed that it could develop for no particular reason. Today, if there is no coronary heart disease, sick sinus syndrome, or any pathological changes in the area of the atrioventricular junction, then this is a manifestation of connective tissue dysplasia syndrome. I won't dwell on this.
Let's see how to stop AV nodal tachycardia. Of course, the number one drug is calcium channel blockers, undoubtedly, that is, Verapamil. The effectiveness of Verapamil and this group of drugs is 95%, according to some data even 98%. Beta-blockers and Digoxin are still written in the same line. But remember that the effectiveness of beta-blockers is low, only 50%, and Digoxin exhibits its antiarrhythmic effect in this type of heart rhythm disorder only in the second hour.
If you are treating a patient without structural heart pathology, that is, the ejection fraction is sufficient, there is no problem. You can use Propafenone if it is in injectable form, but in 2013 representatives still promise that it will be on our pharmaceutical market.
In most cases, as is written in all recommendations, Amiodarone and Sotalol are not used. It will not be a mistake, of course, if you introduce the same Amiodarone. No one has ever seen sotalol injected. Of course, it will not be a mistake whether you stop or not stop this AV nodal reciprocal tachycardia.
But further it is written that class IA drugs are used to a limited extent. Why? Because Novocainomide, which exists in injections, unfortunately, has a vagolytic effect on the atrioventricular connection, and having, for example, tachycardia with a frequency of 160 per minute. And by introducing Novocainomide, you can get the same type of tachycardia, but it will already occur at a frequency of, for example, 180-200. Vagolytic action, that is, acceleration of the movement of the impulse in this vicious circle. Or, of course, cardiac pacing will stop reciprocal tachycardia in 100% of cases.
What else would I like to remind you? That beta blockers should not be administered in combination with Verapamil, Diltiazem, or in rapid succession, because this can lead to severe bradycardia and even asystole. And in this regard, I would like to recall the expression of Richard Fogoros, who in his book “Antiarrhythmic Drugs” wrote back in 1999 that the idea of antiarrhythmic drugs as a “softening balm” is not just naive, but even dangerous. For if we adhere to this view of antiarrhythmic drugs as a “softening balm,” then in the case when the arrhythmia does not respond to a certain drug, what does the doctor do? Either he naturally increases the dose of the same drug, or, even worse - I want to emphasize, Richard Fogoros writes correctly - he adds another drug. Not a single ambulance doctor will write a note on the accompanying certificate if he administered the drug and did not stop the tachycardia; if the patient’s hemodynamics are stable, bring him to the hospital, then we will figure it all out and try to stop this type of tachycardia.
What else do you need to remember? If, with AV nodal reciprocal tachycardia, the ejection fraction is low or there are obvious manifestations of heart failure, understanding that Verapamil is 98% effective, then you need to use either Amiodarone or Digoxin. Do not forget that Verapamil does have a negative inotropic effect and in this situation, despite such high efficiency, it is contraindicated.
If you encounter AV nodal reentrant tachycardia, the patient has low blood pressure numbers. Yes, indeed, it is described in the literature that vozopressors can interrupt such tachycardia. Because of which? Due to a reflex increase in vagal tone when trying to raise blood pressure numbers. We are talking, naturally, about Mesotone, a 1% solution that you can administer for arrhythmic collapse or severe hypotension in a dose of 0.1-0.2 milliliters.
How to prevent it? But, strictly speaking, there are no large clinical studies on the prevention of AV nodal reciprocal tachycardia. Abroad, these are mainly surgical interventions. And you see, some drugs were compared, and in fairly high doses. Pay attention to the dose of Digoxin, Verapamil, Propranolol - they had the same effectiveness. As for Propafenone - it is effective in 80% of cases - I will show another graph in general on the effectiveness of drugs.
The next thing is oral administration of Amiodarone and the maintenance dose, you see, was 200-400 milligrams, and for 66 days it prevented paroxysms in all patients. I specifically put three question marks because I found this study. There were a total of 17 patients in the study. Of course, there is no evidence base here. But, nevertheless, I repeat once again that these patients are mainly taken for surgical treatment.
If it is not possible to carry out surgical treatment, then with a reduced ejection fraction, of course, and with a severe functional class of CHF, you need to use Amiodarone.
Some antiarrhythmics that are listed in this table (and you see - the years 1987, 1999 and the last year - 2008) are good at preventing AV nodal reciprocal tachycardia, in particular, we have Propafenone in Propanorm tablets. With AV nodal reciprocal tachycardia, what was discussed now is up to 80%, in no way inferior to either Sotalol or Amiodarone.
Another study by our Russian authors - Professor Bunin and co-authors, 2010 - showed that Propanorm, as a representative of the first C class, is quite good - you see, 75% and 81% - prevents both focal atrial tachycardia and AV nodal reentrant tachycardia , and AV reentrant tachycardia associated with an accessory conduction pathway. The effectiveness of this drug is very good.
The next type of tachycardia that I wanted to talk about very briefly is the so-called orthodromic tachycardia - tachycardia associated with additional conduction pathways. How to stop orthodromic tachycardia, that is, tachycardia with narrow complexes? The first point is occupied by all these drugs. If you don’t reread everything, then I can simply say that any antiarrhythmic drug for narrow complex tachycardia, except for drugs of the first B class: except for the Lidocaine class. That is, drugs of the first A class can be used, drugs of the first C class, beta-blockers, which affect the atrioventricular node. We don’t care where to break this re-entry circle: either act on the accessory pathway or on the atrioventricular connection. These are antiarrhythmics and third class, and, of course, Verapamil drugs.
As for tablet drugs, it is written here: the combination of Diltiazem and Propranolol had an effectiveness of 94%. But if you have never tried to use this combination, the first time yourself, it is necessary under the supervision of your doctor, then just do not recommend this combination of drugs to the patient. Moreover, this combination, you see - 94%, turned out to be even more effective than the use of a drug of the first C class, in particular we are talking about Flecainide.
And, of course, transesophageal pacing, because orthodromic tachycardia is AV reentrant tachycardia. I repeat once again: all reciprocal tachycardias are very easy to stop.
Regarding preventive therapy, you see this percentage of how well antiarrhythmic drugs work. Not a bad drug, you see, Sotalol, Propafenone, Flecainide, and 100% - I am always confused by 100% in general in medicine and especially in arrhythmology - but, nevertheless, the combination is not bad: Propafenone (Propanorm) + beta-blockers - 100% . Again, when you open this study, you will see that there were a total of 27 or 26 patients in the study. Basically, if we have a patient with accessory atrioventricular connections—of course, it's radiofrequency ablation of those accessory pathways.
Another little piece is atrial fibrillation plus additional pathways. We quite often see such cardiograms, very ugly. If you look at this cardiogram, it will very much remind you of monomorphic ventricular tachycardia. But we will see a clear inequality of RR intervals. Yes, the QRS complexes are wide, but there is a clear inequality of RR intervals, because if it were monomorphic ventricular tachycardia, there may be an inequality, but it is delicate, it should not be more than 0.02 seconds, that is, no more than 20 milliseconds . Here we see ordinary atrial fibrillation, but, unfortunately, the discharge of impulses occurs through an additional pathway available to the patient. That's why it's such an ugly film. And if you see a patient with such an electrocardiogram, in addition to the fact that we will now discuss how to stop such tachycardia, immediately tell the patient: “You must definitely go to a surgical clinic.”
So, what to buy? With a wide QRS complex, only three drugs are indicated: Propafenone, Amiodarone and Novocainomide (it is called Procainomide abroad).
Of course, you should avoid prescribing Digoxin, but with WPW syndrome, we all know about Digoxin - under no circumstances. Verapamil is not allowed with wide complexes, Lidocaine is not allowed, as well as beta-blockers. Why? I will return to this film again. Imagine that you, as a doctor, mistook this irregular heart rhythm for ventricular tachycardia. It is good that at the moment Amiodarone takes priority in stopping ventricular tachycardia. But if you still love and give priority to Lidocaine as, from your point of view, a safer drug, imagine that for this atrial fibrillation with conduction through an additional conduction pathway you will administer Lidocaine. You will simply end up with the death of the patient. Therefore, we know about Digoxin and Verapamil, and, of course, we don’t forget about beta blockers. But you may ask: “Why is Lidocaine mentioned here?” It’s not for nothing that I returned to this film to show this feature.
How to prevent it while the patient is on the waiting list, waiting in line for radiofrequency ablation? What is used? A good, excellent drug is Propafenone (Propanorm), you can prescribe Amiodarone or Sotalol. But I repeat once again: due to the high frequency of organotoxic effects from Amiodarone, still try to use it last, especially if the patient is planning for surgery. Sometimes long-term administration of drugs - we are talking about Amiodarone - can interfere with surgeons during electrophysiological studies and surgical intervention.
Why are first class A drugs not used? Because they do affect the accessory pathway, but they do not affect conduction through the normal atrioventricular conduction system. Why is Verapamil not used with beta blockers? They, on the contrary, affect the atrioventricular connection and have virtually no effect on conduction in the accessory pathway. So, Propaphenone (Propanorm), Amiodarone, Sotalol, which kill two birds with one stone: they inhibit the conduction of excitation through the atrioventricular system and affect the accessory pathway.
If a patient has chronic heart failure, but preserved systolic function - I always emphasize this too, that is, we are talking about diastolic dysfunction, that is, if the ejection fraction is preserved - combination antiarrhythmic therapy can be used. Yes, of course, we treat the underlying disease, where we use basic basic medications, including beta-blockers, and if titrated, selected doses of beta-blockers do not help, then you can add Propafenone (Propanorm) to the beta blockers. The combination of Propafenone + Verapamil is possible in the absence of again pronounced manifestations of heart failure. And, if there is no effect from other combinations, the combination of Propafenone + Amiodarone is possible. But it is advisable to begin this combination therapy in a hospital setting.
And almost the last pictures. I always start with the fact that if you have a patient with any kind of supraventricular tachycardia, and if this supraventricular tachycardia causes hemodynamic disturbances, you don’t need to remember any antiarrhythmic drugs - you need to perform electrical cardioversion. The discharge power, I repeat once again, is small. The only thing is that if you are using an older model non-synchronized defibrillator, then for atrial fibrillation the power of the first shock is - note - 200 joules.
And the last picture. As for surgery. Here, however, the title also contains typical atrial flutter and supraventricular tachycardia, and we will pay attention to the yellow and green columns first of all. I wasn’t going to talk about atrial flutter today, so we will evaluate those tachycardias that we just talked about. Not bad efficiency, actually. We are talking about radiofrequency ablation. You see – 90-94%. The mortality rate is very low, and repeat radiofrequency ablations in the yellow and green bars are 8% and 5%.
The most important thing is with AV nodal reciprocal tachycardia, when our surgeons go to the atrioventricular connection - after all, the length of the node is 6 millimeters, the width is only 3 millimeters - it is very difficult to influence the fast and slow conduction channels, so the most important thing is for surgeons not to damage the atrioventricular node. Abroad, if we damage the atrioventricular connection, we get the so-called artificial complete AV block, and then we have to implant a pacemaker - this is considered a complication of this operation.
Risk factors for developing cardiac arrhythmia
Risk factors for developing cardiac arrhythmias include:
- ✔ Genetics.
In people with congenital abnormalities of the heart, arrhythmias occur more often. Moreover, a number of arrhythmias (eg, Wolff-Parkinson-White syndrome, some supraventricular tachycardias, some forms of long QT syndrome) are congenital. - ✔ Thyroid diseases.
With increased thyroid function, increased production of hormones occurs, overall metabolism increases, and heart contractions become more frequent and irregular. Atrial fibrillation most often develops. With insufficient thyroid function, metabolism decreases, which causes bradycardia, and in some cases, extrasystole. - ✔ High blood pressure.
This increases the risk of developing coronary heart disease. High blood pressure also causes the wall of the left ventricle to thicken, which can change the way impulses are conducted through it. - ✔ Diabetes mellitus.
Diabetes mellitus in the stage of decompensation (uncontrolled blood sugar levels) greatly increases the risk of developing coronary heart disease and arterial hypertension. In addition, episodes of hypoglycemia (low blood sugar) can be a trigger for the development of cardiac arrhythmias. - ✔ Electrolyte disturbances.
Electrolytes such as potassium, magnesium, sodium and calcium form the basis for the formation, maintenance and conduction of electrical impulses in the heart. Too high or too low concentrations of electrolytes in the blood and in heart cells affect the electrical activity of the heart and can cause the development of arrhythmias. - ✔ Use of stimulants.
Psychostimulants such as caffeine, nicotine, etc. cause the development of extrasystole and can also lead to the development of more severe heart rhythm disturbances over time. The use of amphetamines and cocaine can damage the heart muscle with the development of any of the existing arrhythmias and even lead to sudden cardiac death due to the development of ventricular fibrillation.
Description of supraventricular arrhythmia
Supraventricular arrhythmia (SVA) is also defined as atrial or supraventricular. The source of the spread of extraordinary contractions is in the atria, that is, above the ventricles, hence the name of the pathology.
The formation of NFA is based on the formation of a pathological focus of trigger activity, which sends periodic extraordinary impulses. In some cases, the electrical signal is transmitted through the atria or in the atrioventricular node via the reentry mechanism, then a cyclic propagation of the impulse is observed, leading to an acceleration of cardiac activity.
The development of supraventricular arrhythmia can occur against the background of cardiovascular diseases, which is typical for old age, or without visible clinical signs during the formation of the body, that is, in children and adolescents.
If the pathology is associated with other cardiovascular disorders, then it is important to undergo regular examinations with a cardiologist. Otherwise, you will have to find out the dangers of supraventricular arrhythmia from your own experience.
Screening and diagnosis of arrhythmia
To diagnose arrhythmias, the doctor usually asks the patient if they have any heart disease and/or thyroid problems. In addition, specific types of medical testing are always performed to detect arrhythmia. This may be a short or long-term passive recording of an electrocardiogram (a day or more), or an attempt to provoke an arrhythmia while simultaneously continuously recording the heart rhythm.
Passive monitoring methods include:
- Electrocardiography (ECG). During an ECG, electrodes attached to specific locations on the arms, legs, and chest record the electrical activity of the heart. An electrocardiogram examines the intervals and duration of each phase of heart contraction.
- Daily ECG monitoring using the Holter method. A portable ECG recorder is installed for a day or more to record the electrical activity of the heart as a person performs his usual daily activities, as well as during sleep.
- Echocardiography. Allows you to use an ultrasound sensor to obtain an image of the chambers of the heart, clarify their sizes, the movement of the walls and valves and other information.
Arrhythmia can be induced using the following tests:
- Tests with physical activity . Some arrhythmias are triggered or worsened by exercise. During the “stress” test, a treadmill or stationary exercise bike is used. During the test, a continuous ECG recording is made. To perform a “stress” test, medications can be used that stimulate the heart in a similar way to physical exercise. Typically, this method is used when it is impossible to perform physical exercise, as well as to establish a diagnosis of coronary heart disease.
- Tilt table test . When a person has unexplained loss of consciousness, slant tests may be helpful. In this case, rhythm and blood pressure are monitored in a horizontal position for 20-30 minutes. Then a special table is moved to a vertical position and rhythm and blood pressure are also monitored for 10 minutes. In this way, the condition of the heart and the specialized nervous system that controls the functioning of the heart when changing body position and moving from a horizontal to a vertical position is assessed.
- Electrophysiological study and mapping . This study is carried out using the thinnest catheters - electrodes, which are carried into the heart cavity. When electrodes are installed in the area of certain areas of the conduction system of the heart, they can be used to study the propagation of an electrical impulse throughout the heart, induce arrhythmia, while studying its localization and mechanism, and also test the therapeutic effect of various medications. This is the most informative and accurate method for diagnosing most arrhythmias. In addition, when performing EPI, it is possible not only to identify, but also to eliminate the arrhythmogenic focus using a special thermal effect called radiofrequency. In this way, most supraventricular and some types of ventricular tachycardias are eliminated. Currently, this method is also used for atrial fibrillation.
Diagnostics
Tachycardia can be sinus and paroxysmal; they differ from the location of the electrical impulse that causes the heart to contract. To make a diagnosis, the doctor of the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency performs a physical examination, collects anamnesis and prescribes tests.
Physical examination includes:
- external examination of the patient;
- heart rate measurement;
- blood pressure measurement.
Instrumental research:
- ECG;
- ECG with additional load on the body;
- daily ECG monitoring;
- ECHO;
- stress echocardiography;
- MRI;
- CT cardiography.
Complications of arrhythmia
.
A number of heart rhythm disorders can increase the risk of developing conditions and diseases such as:
- Stroke
. When the atria fibrillate, they are unable to adequately pump blood to the ventricles. Slowing blood flow in the atria leads to the formation of clots. If a small piece breaks off from the clot, it can enter the bloodstream, spread throughout the body and clog the cerebral arteries, causing the development of ischemic stroke, i.e. damage or death of part of the brain, and sometimes leads to death. - Congestive heart failure
. Due to a prolonged period of bradycardia or tachycardia, such as atrial fibrillation, the heart may not pump efficiently. By controlling your heart rate, you can improve left ventricular contractility and reduce signs of heart failure.
How to get treatment at the Scientific Center named after.
A.N. Bakuleva? Online consultations
Symptoms of paroxysmal supraventricular tachycardia
Paroxysmal tachycardia always has a sudden, distinct onset. The patient feels a push or compression, and sometimes a prick, in the area of the heart.
The attack may be accompanied by symptoms:
- dizziness;
- noise in the head;
- lightheadedness or fainting;
- sweating;
- nausea;
- trembling in the body.
To correctly diagnose tachycardia, it is important to conduct a thorough interview and examination of the patient. Highly qualified doctors of the Cardiology Center of the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency will be able to quickly identify the disease.
Treatment and prognosis for supraventricular arrhythmia
If the patient is asymptomatic or causes minimal discomfort, specific treatment is not carried out. In such conditions, it is enough to adhere to a healthy lifestyle and eat right so that the arrhythmia does not worsen. If the pathology provides the patient with psychological discomfort, then antiarrhythmic drugs can be prescribed - sotalol, amiodarone, propafenone.
In severe cases, when the arrhythmia is not corrected with medications, surgical treatment is resorted to. The following types of operations can be performed:
- implantation of a pacemaker - indicated for weakness of the sinus node, when the atria cannot fully contract or the impulse is chaotic;
- implantation of a defibrillator - installed for prolonged tachycardias that cannot be controlled with medications;
- Radiofrequency ablation is a minimally invasive operation that, in some forms of arrhythmia, helps to get rid of the pathology by 100%. In particular, good effectiveness of RFA is observed in WPW syndrome.
Classification of supraventricular arrhythmia
The pathology is quite variable, so it is divided according to the nature of its manifestation into three types: tachycardia, bradycardia, extrasystole.
All extrasystoles differ in frequency, location and number of ectopic foci, as well as the time of occurrence of the attack.
By frequency
The frequency of premature contractions, which are counted per minute, divides all extrasystoles into:
- single - there are no more than five extrasystoles;
- paired - the ECG shows two extrasystoles located one after the other;
- group - premature contractions occur several in a row;
- multiple - more than five extrasystoles are determined.
According to the location of the outbreak
It can be determined directly in the atria or in the atrioventricular node. In any case, they talk about supraventricular arrhythmia.
Atrial arrhythmias are localized in the corresponding part of the heart
Atrioventricular arrhythmias are characterized by the location of an ectopic focus in the septum located between the atria and ventricles.
By number of outbreaks
When determining one ectopic focus using special research methods, they speak of monotopic extrasystole.
The presence of two or more pathological foci indicates polytopic extraordinary cardiac contractions.
By time of occurrence
Using an ECG, the time period during which the extraordinary contraction occurs is determined. There are three types of extrasystoles, distinguished by the time of formation:
- early - occur at a time when the atria contract;
- interpolated - the localization site is at the junction of the contractions of the atria and ventricles;
- late - characteristic of the period of ventricular contraction; they can also form during relaxation of the heart (in diastole).