Blood in the stool is a symptom of serious diseases, signaling the presence of bleeding in the gastrointestinal tract. By the type, nature, intensity and duration of bleeding, you can roughly determine the cause of its appearance. It is important to consult a doctor, even if there are no obvious inclusions, but the color of the feces has changed. The Anapa Diagnostic Center performs comprehensive diagnostics to identify gastrointestinal diseases and their treatment using medical and surgical methods.
What does the presence of blood in stool indicate?
Blood can be released directly during defecation or independently of it in any part of the intestine, in the stomach, or liver. The nature of the discharge indicates a possible cause:
- Anal fissures. They are characterized by bright, fresh droplets of blood that has not had time to coagulate on the surface of feces. Most often, such bleeding occurs after constipation.
- Intestinal infections. Parasites damage the intestinal mucosa, resulting in bloody inclusions or changes in the color of stool. As a rule, the stool is loose and diarrhea is a concern.
- Sexually transmitted infections. Mini-bleedings occur due to damage to the gastrointestinal mucosa by bacteria. Bloody marks are visible on top and inside the stool.
- Haemorrhoids. The blood is dark and visible on the surface.
- Nonspecific ulcerative colitis. In addition to blood clots and streaks, stool contains mucus and pus. Exacerbation of the disease is characterized by more intense bleeding caused by intestinal perforation.
- Crohn's disease, leading to inflammation of the mucous membranes of the gastrointestinal tract. Clots and blood streaks in feces.
Blood is almost always a concern with neoplasms :
- Cancer, polyps of the small intestine. Heavy bleeding, but already in advanced stages. At the beginning of the development of neoplasms, a person loses weight and complains of weakness and poor appetite.
- Colon cancer. The blood is burgundy-red, but is often mixed with stool and is clearly not visible.
- Cancerous tumors of the rectum. At the beginning of formation, there are bloody streaks, in the later stages - clots with an unpleasant odor.
In men, the presence of traces of blood in the stool may occur when prostate cancer grows in the large intestine. In women, the cause may be intestinal endometriosis or uterine cancer.
Blood in the stool
Iron deficiency
Ulcer
Haemorrhoids
Allergy
61488 07 April
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Blood in the stool: causes of occurrence, what diseases it occurs with, diagnosis and treatment methods.
Definition
The appearance of blood in the stool cannot be ignored, since it is one of the most alarming and serious symptoms of gastrointestinal (GIT) diseases and requires examination and medical attention.
Types of blood in stool
Blood in the stool can be red or cherry-colored, or almost black, bleeding can be profuse or spotting, and the act of defecation can be painful (not only the anus, but also the stomach can hurt) or normal.
In some cases, blood in the stool is not visualized, but is detected during laboratory examination - this phenomenon is called occult blood.
There are acute and chronic bleeding, depending on the speed of development of symptoms. Acute occurs in a matter of minutes and is characterized by large loss of blood. Other symptoms characteristic of this condition are pallor, severe weakness, rapid heartbeat, and a drop in blood pressure. The patient requires emergency medical care.
Chronic bleeding is caused by small but regular blood loss, which results in anemia.
Possible Causes of Blood in Stool
Blood in stool is always a symptom, not a disease. By its color, you can determine in which part of the gastrointestinal tract the bleeding has developed. Depending on this, the following reasons for the appearance of blood in the stool are distinguished:
- Scarlet
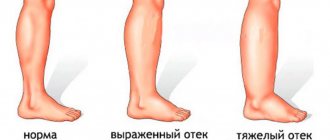
blood not mixed with stool may indicate a crack in the skin or mucous membrane of the perianal area. The appearance of blood is accompanied by intense pain during bowel movements. The condition can develop regardless of the patient's age. Often cracks occur with prolonged and frequent constipation as a result of injury to the mucous membrane of the final section of the rectum and the skin of the perianal area with solid feces. In children, the cause of cracks may be allergic reactions to cow's milk protein, because... liquid feces constantly irritate the skin and mucous membranes. A similar situation is observed with lactase deficiency. Cracks can also appear if the technique of administering enemas is incorrect. - Dark red blood
, which does not mix with feces, is often a symptom of hemorrhoids - a disease characterized by varicose veins of the anus and rectum with the formation of hemorrhoids. This occurs when blood stagnates due to low physical activity, excess weight, constipation, and during pregnancy. With hemorrhoids, blood usually appears after a bowel movement. Patients often complain of itching in the perianal area, burning, and dilated hemorrhoids can be palpated (under the skin in the anal area in the form of small balls of elastic consistency to the touch).
- The appearance of blood in the stool is one of the symptoms of intestinal polyps (proliferation of the mucous membrane). Polyps may not make themselves felt for a long time, and bleeding develops only when they are damaged. Typically, trauma to a polyp is not accompanied by pain, with the exception of polyps of the anal canal - then the patient complains of itching, discomfort and a feeling of incomplete bowel movement.
- Blood in the stool can be present in various infectious diseases, accompanied by diarrhea, severe abdominal pain, fever, chills, and vomiting.
Infections cause rapid dehydration of the body, so the patient requires treatment in an infectious diseases hospital. - Blood in the stool appears in various inflammatory non-infectious diseases: for example, in Crohn's disease and ulcerative colitis, ulcers form, which often bleed. Blood is released in clots and loose stools. If ulcerative defects have formed in the upper intestines, the blood may be black.
- The release of blood clots
mixed with stool may be a symptom of injury to the diverticulum wall. Bleeding is accompanied by abdominal pain and is transient. - Intense bleeding
often develops when an intestinal tumor disintegrates and the organ wall is damaged. Blood may be mixed with stool, mucus and pus. - If the chair becomes black color
And
liquid consistency
(tarry stools, melena), defecation is accompanied by abdominal pain, severe weakness, increased heart rate and decreased blood pressure, then we are talking about the development of severe bleeding from the upper gastrointestinal tract.The cause of massive blood loss can be a stomach or duodenal ulcer, bleeding from varicose veins of the esophagus with cirrhosis of the liver, disintegration of a stomach tumor, damage from poisoning with caustic and destructive poisons.
- dark pink stool
is considered dangerous , especially in young children. Most often, this is a symptom of the development of intestinal volvulus and requires emergency surgical intervention. Children are restless, refuse to eat, cry, vomit and bursting pain in the abdomen. - The presence of occult blood in the stool can be detected during a test during a routine examination or as part of a special examination.
Among the factors predisposing to the occurrence of diseases, the symptom of which is blood in the stool, can be identified:
- a sedentary lifestyle, which provokes stagnation of blood in the venous plexuses of the rectum and disruption of the passage of feces through the intestines and leading to the development of constipation and hemorrhoids;
- overweight;
- low amount of fiber in the diet;
- alcohol and coffee abuse;
- female gender (pregnancy and childbirth are a risk factor for the development of constipation and hemorrhoids);
- introduction of complementary feeding to infants - with a sudden change in diet, infants may develop constipation and intussusception;
- anal sex - leads to injury to the rectal mucosa and the formation of chronic cracks;
- infection with the human papillomavirus increases the risk of formation of papillomas in the perianal area;
- malignant neoplasms of the gastrointestinal tract in family members.
Which doctors should you contact when there is blood in the stool?
The appearance of blood in the stool requires contacting a proctologist, surgeon, oncologist, or infectious disease specialist. After the examination, the doctor will prescribe a set of instrumental and laboratory tests.
Diagnosis and examinations if there is blood in the stool
- Complete blood count (to identify signs of anemia during hidden bleeding).
Black stool is a sign of bleeding
It is important to consider that blood is not always visible in feces. If the source of bleeding is located in the upper gastrointestinal tract, then it loses its red color and becomes black. In such cases, they talk about occult blood in the stool .
Black feces and tar-black clots are characteristic of dangerous diseases:
- Bleeding from the veins of the esophagus.
- Stomach or duodenal ulcer.
- Erosive gastritis.
- Gastroesophageal reflux disease of the esophagus.
- Neoplasms of the esophagus.
- Intestinal tuberculosis.
- Colon cancer, benign tumors.
- Polyps.
- Cirrhosis of the liver.
The reason may also lie in problems with blood vessels and damage to the arteries of internal organs. In children, the presence of blood in the stool may indicate dysbacteriosis, intestinal obstruction, and allergic reactions.
You cannot examine the contents of the toilet on your own; it is a waste of time. Even a specialist will never make a diagnosis based solely on external signs and stool analysis.
Symptoms
Bleeding from the upper gastrointestinal tract is characterized by tarry stools, if the blood loss is extensive, then the stool may be tarry, the stool is black, semi-liquid, with an unpleasant odor.
There may be fresh blood in the stool if the blood loss is extensive. In this case, there is severe pain in the chest, bloody vomiting with clots the color of coffee grounds. This symptomatology is typical for bleeding from the stomach, duodenum, and esophagus. The appearance of blood from the anus is characteristic of bleeding from the colon or terminal ileum. When bleeding from the lower gastrointestinal tract, the stool is bloody, the discharge from the anus is bright red, the blood is mixed with the stool, and with extensive bleeding, symptoms of loss of circulating blood, hemorrhagic shock, and hypovolemia appear. When bleeding from anal fissures, scarlet blood is released during bowel movements.
When bleeding occurs, the patient experiences increased sweating, weakness, disorientation, pallor, tachycardia, and syncope.
With hidden bleeding from the upper gastrointestinal tract, there may be no vomiting mixed with black flakes, and the state of anemia increases.
What examinations need to be completed
If blood is detected in the stool and systematic drops on toilet paper, you should contact a proctologist. The doctor will prescribe tests and instrumental examinations to identify gastrointestinal pathologies.
At NeoMed, to establish the most accurate diagnosis, a comprehensive examination is carried out, which will reveal the source of bleeding, the cause and degree of harm caused to the body. Often hidden blood loss leads to anemia. The scope of the diagnosis is determined by the doctor. It includes:
- Analysis of feces for occult blood and helminths.
- Blood test for hemoglobin.
- Examination of the anus to identify cracks and external hemorrhoids.
- Sigmoidoscopy is an instrumental examination of the mucous membrane of the rectum and distal parts of the sigmoid colon.
- Colonoscopy is an endoscopic examination of the intestine and its internal walls from the inside. At NeoMed, the procedure is carried out in medicated sleep without pain or discomfort.
- Ultrasound of the intestines, stomach, and, if indicated, liver.
- X-ray of the gastrointestinal tract.
- Gastroscopy is an endoscopic examination of the stomach and esophagus. Performed if bleeding is suspected in the stomach, esophagus, or duodenum.
- CT and MRI of the internal organs of the digestive system to identify benign and malignant formations.
During all endoscopic examinations, when indicated, a biopsy is performed - materials are taken for histology. This is the best method for early detection of cancer. If bleeding is detected, it is stopped immediately. And detected polyps are removed during the examination.
Do not hope that the blood will disappear and the stool will become light; it is possible that every day is already expensive to establish a diagnosis and begin treatment. They are already waiting for you at the Anapa clinic “NeoMed”, call and make an appointment.
Diagnostics
Before diagnosing the source of bleeding, it is necessary to stabilize the patient's condition.
Intravenous administration of fluid or blood components is used, and respiratory resuscitation is additionally performed. Diagnostic methods:
- taking anamnesis;
- collection of clinical symptoms;
- laboratory diagnostics - general blood test, coagulogram, liver tests;
- digital examination of the rectum;
- instrumental diagnostics:
- endoscopic examination of the upper gastrointestinal tract if upper bleeding is suspected;
- angiography;
- irrigoscopy or CT enterography - for hidden bleeding;
colonoscopy – for bleeding from the lower sections;
Causes of bloody stool
Bloody feces
is a symptom of a number of diseases of the intestines and lower gastrointestinal tract of an oncological, inflammatory or infectious nature. Experts divide the triggering factors that cause bleeding into several groups:
| Group of reasons | What are they? |
| Neoplasms of a malignant nature | Most often, they are represented by colorectal cancer, even in the initial stages of which small amounts of blood may appear. If the tumor is not treated and it disintegrates, serious blood loss is possible due to the melting of large blood vessels. |
| Pathological conditions characterized by proliferation of the colon mucosa | Abnormal growths include polyps, which are one of the most common causes of blood in the stool. This especially applies to the villous type of polyps, since they are rich in blood vessels. |
| Chronic diseases of the intestines and anus |
|
| Infections and poisoning |
|
| Congenital and acquired disruptions in local circulation | Circulatory deficiency or disturbances in the pelvic and abdominal areas, leading to the development of angiodysplasia or intestinal ischemia. |
| Complications of various diseases |
|
Treatment
Treatment depends on the location of the bleeding and its intensity.
In case of minor bleeding, nutrition is adjusted, hemostatic drugs are prescribed, and deficiencies of microelements and vitamins are corrected. Additionally, the patient receives enteral or parenteral nutrition.
In case of acute bleeding, intensive therapy is necessary to stabilize the patient - restoration of circulating blood volume with the help of plasma substitutes or blood components. If respiratory function is impaired, it is necessary to restore respiratory function.
For varicose veins of the esophagus, endoscopic sclerotherapy, clipping, and vein ligation are used.
If this is ulcerative bleeding, endoscopic coagulation or angiographic embolization of the pathological vessel and intensive drug therapy with proton pump inhibitors are advisable.
For intestinal diverticulosis, the coagulation method is used, and hemostatic clips are used.
Preventing blood in stool
- 1. Annual preventive examinations with doctors.
- 2. Timely treatment of diseases.
- 3. Occult blood test.
- 4. Healthy lifestyle.
- 5. Eating foods containing fiber.
- 6. Daily physical activity.