Detailed description of the study
The discharge of blood during defecation may not always be noticeable by humans. Nevertheless, this symptom serves as an important indicator of intestinal inflammation or the development of an oncological process in its walls. Damage to the mucous membrane as a result of an inflammatory process of various nature (intestinal infection, autoimmune disease - Crohn's disease or ulcerative colitis), as well as tumor growth, leads to bleeding that is invisible to humans. Chronic blood loss contributes to anemia. Typically, a visit to a doctor is associated with the presence of the following complaints: - The appearance of severe weakness and fatigue; - Pale skin; - Brittle nails and hair; - Decreased appetite; — Reducing body weight. If anemia and a decrease in hemoglobin levels in the blood are suspected, it is necessary to search for the causes and sources of blood loss. Hidden intestinal bleeding is one of the most common causes of this problem. Guaiac-based tests have been used for many years to detect occult blood in stool. This method makes it possible to detect heme, a component of hemoglobin, in a biomaterial. However, many foods (red meat, broccoli, radishes, apples, nuts and others) can cause a false positive test result, and it has low sensitivity (no more than 25%). These disadvantages reduce the accuracy of diagnosing hidden bleeding. The ColonViewHb and Hb/Hp test is based on a new method for detecting occult blood in stool. The essence of the study is to identify hemoglobin and the hemoglobin-haptoglobin complex, which arises due to the destruction of red blood cells, using antibodies to these components. Antibodies bind only to human hemoglobin, which significantly increases the specificity of the test. Determination of the hemoglobin-haptoglobin complex allows increasing the sensitivity of the study, since it is not destroyed by aggressive factors (acid, bile) in the gastrointestinal tract. Colon cancer occupies a leading position in the structure of mortality from cancer. This is largely due to people seeking medical help late and a long period of tumor growth without clinical manifestations. Hidden bleeding from the intestines may be the only sign of the disease for a long time. Therefore, screening for the presence of blood in stool is recommended in most countries of the world for people over 50 years of age.
Determination of hemoglobin/transferrin in feces
This study is aimed at identifying bleeding from the lower gastrointestinal tract. The concentration of fecal hemoglobin and transferrin, determined using the quantitative immunochemical Fecal Occult Blood Test FOB Gold, has great advantages over the previously widespread standard method of qualitative analysis of feces for occult blood. The well-known fecal occult blood test, which uses less specific chemical tests, still has a number of disadvantages, such as a positive reaction to hemoglobin and myoglobin of animal origin coming from food, as well as to some substances. This determines the need to follow a diet before taking a test for hemoglobin in stool . The new version of this test using immunochemical reactions is more sensitive and strictly specific to human hemoglobin, which eliminates the need for a diet before testing for hemoglobin in stool. In addition to these advantages, a new method for determining the concentration of fecal hemoglobin and transferrin ( test for hemoglobin in stool, test for transferrin in stool ) is a potential tumor marker, that is, it can be used for the diagnosis of precancerous lesions of the intestine and the early diagnosis of colorectal cancer.
Determination of the concentration of fecal transferrin, or test for transferrin in feces, in combination with quantitative determination of hemoglobin in feces , is an analysis that today has the highest diagnostic sensitivity when examining patients with cancer and precancerous processes of the large intestine and rectum.
Quantitative analysis of transferrin in feces using an immunochemical method allows one to predict the likelihood, stage and localization of a precancerous and cancerous pathological process. Therefore, today the feasibility of using an immunochemical analysis for hemoglobin in stool and an analysis for transferrin in stool has been proven as a screening for colorectal cancer, which has become a rather urgent problem, given the increased incidence of the disease and the asymptomatic course of cancer.
Quantitative analysis for transferrin and hemoglobin in feces is indicated in the diagnosis of diseases associated with inflammatory, autoimmune, ulcerative processes in the mucous membrane of the lower gastrointestinal tract.
to take a test for hemoglobin and transferrin in feces as an additional test if indicated for chronic hemorrhoids, helminthic infestations, or previous bacterial or viral intestinal infections.
An increased content of transferrin in feces during analysis indicates a predominant damage to the upper intestines, and hemoglobin - to the lower ones. If high values of both indicators are detected, extensive intestinal damage is most likely.
Tests for transferrin and hemoglobin are an alternative to colonoscopy. The analysis allows for the selection of patients requiring colonoscopy. If the values are normal, a colonoscopy is not performed; the decision to conduct the study is made by the doctor. High values of these indicators are the basis for a colonoscopy.
Preparing for the study
The stool is collected in a sterile, disposable container. When preparing a patient for the study, alcohol and NSAID drugs (non-steroidal anti-inflammatory drugs - ortofen, indomethacin, etc.) acetylsalicylic acid, warfarin (and other anicoagulants), corticosteroid drugs reserpine, phenylbutazone should be discontinued 2 days in advance.
To obtain reliable results, samples should not be used in patients during menstruation, as well as during rectal bleeding due to hemorrhoids or constipation.
You cannot examine stool obtained after an enema and taking laxatives, as well as X-ray examination of the stomach and intestines using contrast agents.
When is a referral for analysis issued?
In addition to screening the age group over forty years, the doctor writes a referral for this test in the following cases:
|
The analysis reveals the slightest damage to the walls of the intestine. If an admixture of blood higher than normal is detected in the stool, the test is repeated and, if the result is confirmed, the patient is sent to see a proctologist or gastroenterologist.
Interpretation of results/Information for specialists
NEGATIVE RESULT
Hemoglobin and haptohemoglobin complex – NOT DETECTED
Absence of hemoglobin and haptohemoglobin complex in the stool sample is normal
A false negative result is also possible against the background of an occasionally bleeding polyp (neoplasm) and in the absence of bleeding at the moment.
IMPORTANT: a negative test result does not completely exclude intestinal pathology, for example, in the case of episodic bleeding of a polyp. In this case, it is possible to recommend repeated examinations (at least three times) at intervals determined by the attending physician, and to use instrumental diagnostic methods for final verification of the diagnosis.
Normal values
| Index | Meaning |
| Macroscopic examination | |
| Consistency | Dense |
| Form | Decorated |
| Color | Brown |
| Smell | fecal, unsharp |
| pH | 6 – 8 |
| Slime | Absent |
| Blood | Absent |
| Leftover undigested food | None |
| Chemical research | |
| Reaction to occult blood | Negative |
| Reaction to protein | Negative |
| Reaction to stercobilin | Positive |
| Reaction to bilirubin | Negative |
| Microscopic examination | |
| Muscle fibers with striations | None |
| Muscle fibers without striations | units in the preparation |
| Connective tissue | Absent |
| Fat neutral | Absent |
| Fatty acid | Absent |
| Fatty acid salts | insignificant amount |
| Digested plant fiber | units in the preparation |
| Undigested plant fiber | units in the preparation |
| Intracellular starch | Absent |
| Extracellular starch | Absent |
| Iodophilic flora is normal | units in the preparation |
| Pathological iodophilic flora | Absent |
| Crystals | None |
| Slime | Absent |
| Columnar epithelium | Absent |
| Epithelium is flat | Absent |
| Leukocytes | None |
| Red blood cells | None |
| Protozoa | None |
| Worm eggs | None |
| Yeast mushrooms | None |
Decoding indicators
Consistency Liquid feces may indicate overly active intestinal motility, colitis, or the presence of protozoal invasion.
Too tight stools indicate excessive absorption of fluid in the intestines, constipation, and dehydration.
Foamy stool occurs when the pancreas is insufficient or the secretory function of the stomach is impaired.
Pasty feces may indicate dyspepsia, colitis, or accelerated evacuation of feces from the large intestine.
Form
Pea-shaped feces occur with hemorrhoids, anal fissures, ulcers, fasting, myxedema (mucoedema).
Feces in the form of a thin ribbon are observed with stenosis of the small intestine, as well as in the presence of neoplasms in it.
Color
Black color (the color of tar) can be caused by eating certain foods (currants, chokeberries, cherries), taking medications with bismuth or iron, as well as bleeding in the stomach or duodenum, cirrhosis of the liver.
A red tint appears when there is bleeding in the large intestine.
Light brown stool color occurs due to liver failure or blockage of the bile ducts.
Light yellow stool occurs with pathologies of the pancreas and due to excessive consumption of dairy products.
Dark brown color indicates an excess of meat in the diet, as well as increased secretory function in the large intestine.
Green stool is a sign of typhoid fever.
Odor A putrid odor occurs due to the formation of hydrogen sulfide in the intestines and indicates the presence of ulcerative colitis or tissue breakdown, tuberculosis, putrefactive dyspepsia.
A sour smell indicates increased fermentation processes.
A foul odor indicates a malfunction of the pancreas, a lack of bile entering the intestines.
Acidity Increase pH
observed in formula-fed infants, in adults - with putrefactive dyspepsia, as well as with high activity of intestinal microflora.
Decrease in pH
occurs when the absorption process in the small intestine is disrupted, with excessive consumption of carbohydrates, or with increased fermentation processes.
Slime
Mucus can be found both on the surface of the stool and inside it; it is found in ulcerative colitis and constipation.
Blood Blood in the stool is detected during bleeding in the gastrointestinal tract caused by neoplasms, polyps, ulcers, hemorrhoids, and inflammatory processes.
Excessive amounts of bacteria and fungi can cause a false positive response.
Remains of undigested food Undigested food in the feces (lientorrhea) indicates a dysfunction of the pancreas, chronic gastritis, and accelerated peristalsis.
Undigested dietary fiber in stool analysis
Protein The presence of protein in stool indicates pathologies of the duodenum or stomach, colitis, enteritis, hemorrhoids and some other gastrointestinal diseases.
Stercobilin
The absence or significant decrease in stercobilin in the feces (the reaction to stercobilin is negative) indicates blockage of the bile duct or a sharp decrease in the functional activity of the liver. An increase in the amount of stercobilin in feces is observed with increased bile secretion and hemolytic jaundice.
Bilirubin The detection of bilirubin in the stool of an adult indicates a disruption in the process of its restoration in the intestine under the influence of microflora. This indicates intestinal dysbiosis, increased peristalsis, or taking antibacterial drugs during preparation for the test or shortly before.
Connective tissue and muscle fibers are undigested remains of meat and are found when there is a lack of pancreatic enzymes.
Fat Fat in the stool is one of the signs of insufficient pancreatic function or impaired bile secretion.
Excessive fat in stool (steatorrhea)
Plant fiber A large amount of digested plant fiber in the feces indicates the rapid passage of food through the stomach due to a decrease in its secretory function, the absence of hydrochloric acid in it, as well as an excess amount of bacteria in the large intestine and their penetration into the small intestine. Undigested fiber has no diagnostic value, since there are no enzymes in the gastrointestinal tract to break it down.
Starch An increased content of starch in feces, which appears when there is a lack of digestion processes in the stomach, small intestine and dysfunction of the pancreas, is called amilorrhea. Additionally, a lot of starch may be found during diarrhea.
Intracellular starch granules in stool analysis
Iodophilic flora (pathological) The presence of pathological microflora (staphylococci, enterococci, E. coli, etc.) indicates a decrease in the number of beneficial bacteria in the intestines and, accordingly, dysbacteriosis. When consuming large amounts of carbohydrates, clostridia begin to multiply intensively, causing fermentative dysbiosis.
Crystals
Calcium oxalate crystals in feces indicate insufficient stomach function, helminthic infestations, and allergies. Triple phosphate crystals indicate increased decay of proteins in the colon.
Epithelium
A significant amount of columnar epithelium in the stool is found in acute and chronic colitis. The presence of squamous epithelial cells has no diagnostic significance.
Leukocytes
Leukocytes in stool appear in cases of colitis and enteritis of the intestine, dysentery, and intestinal tuberculosis.
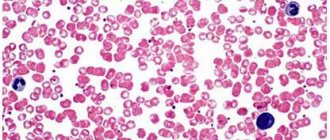
Red blood cells
Red blood cells appear in the feces during hemorrhoids, rectal fissures, ulcerative processes in the large intestine, and during the disintegration of tumors.
Protozoa
Non-pathogenic protozoa are present in healthy people. Pathogens can be detected in feces delivered to the laboratory no later than two hours after collection of the biomaterial. Their presence indicates an invasion.
Worm eggs
Helminth eggs in feces indicate helminthic infestation.
Larvae of roundworms of the genus Strongyloides in feces
Yeasts May be present in stool during corticosteroid or antibacterial therapy. The presence of the fungus Candida albicans indicates intestinal damage.
Sources
- Nomenclature of medical services (new edition). Approved by order of the Ministry of Health and Social Development of the Russian Federation dated October 13, 2021 No. 804n. Valid from 01/01/2018. As amended by Order of the Ministry of Health of Russia dated March 5, 2020 N 148n (including as amended, which came into force on April 18, 2020).
- Shakova H.H. Assessing the reliability of scatological research depending on the storage time of the material. Advances of modern natural science, magazine. 2003. No. 8. P. 131-131.
- Bugero N.V., Nemova I.S., Potaturkina-Nesterova I.I. Factors of persistence of protozoa in the fecal flora in intestinal dysbiosis. Bulletin of new medical technologies, magazine. T. XVIII. No. 3. pp. 28-31.