Detailed description of the study
Prothrombin, or factor II of the blood coagulation system, acts as a precursor to thrombin (the most important component in the formation of a blood clot). It is constantly present in the blood plasma and is activated at the moment of tissue or organ damage. As part of the blood coagulation system, it participates in the formation of a blood clot (thrombus), which prevents excessive blood loss during injury.
Prothrombin time (PTT) and prothrombin index (PTI) are indicators that characterize one of the stages of blood coagulation. Prothrombin time measures the number of seconds it takes for a blood clot to form after certain reagents are added to a blood sample being tested. Prothrombin index is the ratio between the clotting time of control (so-called healthy) blood plasma and the test sample. Determination of these indicators is necessary to assess the functioning of the entire blood coagulation system.
When tissue is damaged and subsequent bleeding occurs, the human body initiates a blood clotting process called hemostasis. Hemostasis involves a series of sequential chemical reactions (coagulation cascade). This cascade involves blood clotting factors, which are activated one after another and lead to the formation of a blood clot.
To ensure a normal coagulation process, there must be a sufficient amount of all factors in the blood, each of which must be functionally active. Insufficient activity can lead to excessive blood loss, excessive activity can lead to excessive clotting.
The test evaluates the overall ability to form a blood clot over a certain period of time (measured in seconds). The prothrombin index expresses the ratio of the clotting time of the test blood plasma to the control (normal) plasma.
Tests of prothrombin time and prothrombin index are ordered on a regular basis when a person is being treated with anticoagulant drugs (Warfarin) to ensure that the drug is having the desired effect.
Also prescribed if a person has signs or symptoms of excessive bleeding, such as frequent unexplained bleeding (nose, gum), multiple bruises.
PTT and PTI studies are performed before planned surgery when there is an increased risk of blood loss or when the person has had episodes in the past that indicate abnormalities in the blood clotting system.
A shortening of prothrombin time and an increase in the prothrombin index may indicate increased blood clotting and is mainly diagnosed in thrombosis, as well as thrombophilia (high risk of thrombosis).
The study of prothrombin time and determination of the prothrombin index indirectly allows us to assess the deficiency of prothrombin complex factors (II, V, VII, X).
During pregnancy, an additional uteroplacental circulation is formed, thanks to which the mother's blood, along with nutrients, flows to the fetus. Increased activity of the blood coagulation system (hypercoagulation) in the third trimester of pregnancy is a physiological process aimed at preparing for childbirth and preventing massive bleeding. Determination of prothrombin time and prothrombin index in pregnant women is mandatory research, since in case of changes associated with insufficient activity of coagulation factors, the risk of bleeding (including postpartum bleeding), placental abruption, and spontaneous termination of pregnancy increases.
Prothrombin time, prothrombin time according to Quick, INR, PTI
A blood test for prothrombin, INR (prothrombin time) is a coagulation test. It determines the clotting time of the patient's plasma after adding a mixture of tissue thromboplastin and calcium ions to it.
Prothrombin test results in different forms.
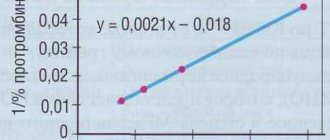
1. Prothrombin according to Quick (%) - like the prothrombin index, allows you to determine the activity of the prothrombin complex of the patient’s plasma in comparison with the measured prothrombin time of the control plasma. This calculation is carried out according to the curve of the dependence of prothrombin time on the percentage of prothrombin complex factors, which is constructed using different dilutions of control plasma. This method of obtaining results is the most accurate, especially in the low value range. Prothrombin according to Quick and the prothrombin index may coincide with each other in the range of normal values. In the zone of low values, which are recommended for the management of patients taking indirect anticoagulants, the indicators of these tests diverge. A prothrombin index of 50 - 60% can be equal to 30 - 40% prothrombin according to Quick. Calculation of prothrombin according to Quick is currently a generally accepted method.
2. INR (International Normalized Ratio), Latin abbreviation INR (International Normalized Ratio) is an additional way of reporting the results of a prothrombin test. It is recommended for monitoring therapy with indirect anticoagulants by the WHO expert committee and the International Committee on Thrombosis and Hemostasis and the International Committee for Standardization in Hematology.
INR is calculated using the formula: INR (INR) = (Patient's prothrombin time / Normal mean prothrombin time) isi, where ISI (International Sensitivity Index of thromboplastin), also known as MICH (International Sensitivity Index) is an indicator of the sensitivity of thromboplastin, which standardizes it relative to international standard.
INR is a mathematical correction. It is used to standardize prothrombin time, which is measured using various thromboplastins with different sensitivities. The optimal INR limits that should be achieved during treatment with indirect anticoagulants depend on the therapeutic goals and are determined by the attending physician. INR and prothrombin according to Quick correlate negatively - this means that a decrease in prothrombin according to Quick corresponds to an increase in INR.
3. Prothrombin time (measured in seconds) reflects the time of plasma clotting after the addition of thromboplastin and calcium mixture. This presentation of the result of the prothrombin test cannot allow for a comparative assessment of the results, due to the fact that different laboratories use different methods and equipment, and most importantly, thromboplastin of different activity and different origin.
4. Prothrombin index is the ratio of the clotting time of the control (“normal”) plasma to the clotting time of the subject’s plasma, which is expressed in %. This indicator in the low range is very dependent on the sensitivity of the reagents used.
Indications
- As a study to identify blood clotting pathologies.
- As a screening test to assess the state of the coagulation system.
- Control of blood clotting during long-term treatment with indirect anticoagulants (coumarins, etc.).
- Study of liver functions to assess the synthesis of prothrombin complex factors in the liver.
Level up:
- tendency to thrombosis: thromboembolic conditions, myocardial infarction, pre-infarction conditions, hypohydration due to increased blood viscosity, hyperglobulinemia;
- drugs that inhibit the action of coumarin (barbiturates, vitamin K) or can inhibit it (corticosteroids, oral contraceptives, meprobamate);
- antihistamines;
- polycythemia;
- malignant tumors.
Downgrade:
- hereditary or acquired deficiency of factors I, II, V, VII and X;
- idiopathic familial hypoprothrombinemia;
- acquired and hereditary hypofibrinogenemia;
- deficiency of vitamin K in the diet (factors II, VII, X are formed in hepatocytes in the presence of vitamin K);
- vitamin K deficiency in the mother (hemorrhagic diathesis in the newborn);
- medications - vitamin K antagonists (anticoagulants - phenylin, etc., coumarins and drugs that enhance their effect: anabolic steroids, clofibrate, glucagon, thyroxine, indomethacin, neomycin, oxyphenbutazone, salicylates; heparin, urokinase / streptokinase).
References
- Zobova, D.A., Paramonova, T.K., Tyurina, N.A. et al. Pathology of the hemostatic system in very early premature birth. – Journal of scientific articles, health and education in the 21st century, 2021. - No. 8. — P.185-187.
- Ponizovich, E.V., Zolotavina, M.L., Chernyavskaya, O.V. Changes in blood hemostasis in patients suffering from viral hepatitis. — Scientific forum: medicine, biology and chemistry, 2021. — pp. 13-17.
- Haram, K., Mortensen, J., Mastrolia, S. et al. Disseminated intravascular coagulation in the HELLP syndrome: how much do we really know? — The journal of maternal-fetal and neonatal medicine, 2017. — Vol. 30(7). — P. 779-788.
Prothrombin time
What is a coagulogram?
A coagulogram is a special study of a patient’s blood sample in a laboratory setting, which can be used to qualitatively and informatively monitor the functioning of hemostasis. This is a complex biosystem that is responsible for maintaining blood fluidity, maintaining a number of processes aimed at stopping bleeding, as well as the timely dissolution of dense blood clots.
The study of hemostasis is also called a hemostasiogram.
In order to maintain basic body functions, blood must be:
- Moderately liquid in order to maintain the ability to transport oxygen and nutrients through vessels to tissues and organs, remove decay products and toxins from the body, maintain the functioning of the immune system, and regulate body temperature;
- Moderately viscous to quickly close holes in large and small vessels in case of traumatic and other types of damage.
In cases where blood clotting is reduced to critical levels, bleeding can lead to massive blood loss and even death of the body.
If we are talking about excess thickness and increased coagulability, there is a high probability of blood clots forming. They can block the most important vessels and cause problems such as thromboembolism, myocardial infarction, and stroke.
A coagulogram is a very important analysis. A properly functioning hemostasis system prevents life-threatening blood loss, as well as the formation of blood clots and blockage of the vascular bed with blood clots, which can lead to unpredictable consequences and even sudden death.
Coagulogram – assessment of blood clotting. Based on the results of the analysis, hidden and obvious pathologies of the body can be detected. Venous blood is used as biological material for research.
This is a complex study, because it is necessary to evaluate each blood parameter separately and analyze all indicators as a whole.
Types of analysis
During the coagulogram, a huge number of parameters are studied. Each of them is important and is responsible for a specific hemostasis function.
Today there are two types of coagulogram:
- Simple;
- Extended.
A simple hemostasiogram helps confirm or refute the presence of problems in the blood clotting system. With the help of this analysis, the doctor can understand where exactly the deviation from the norm is located. If a specialist suspects the presence or development of a pathology, an extended coagulogram is prescribed.
Detailed analysis can also be called quantitative. It implies not only the fact of qualitative changes, but also the definition of specific indicators in numbers.
During a complete coagulation analysis, a number of blood clotting factors are taken into account. Deviation of any indicator from the norm can lead to serious problems for the entire body. Therefore, a simple coagulogram is considered as indicative - it does not provide specific data.
A detailed hemostasiogram is carried out both according to the indications of a specialist to diagnose a number of diseases, and as a standard procedure - before operations, during pregnancy, when taking anticoagulants.
Decoding the prothrombin test according to Quick: table
| Age (years) | Norm (%) |
| Until 6 | From 80 to 100 |
| From 6 to 12 | From 79 to 102 |
| From 13 to 18 | From 78 to 110 |
| From 19 to 25 | From 82 to 115 |
| From 26 to 45 | From 78 to 135 |
| From 46 to 65 | From 78 to 142 |
How to prepare for a thrombin time test
The analysis does not require special preparation. It is recommended to donate blood on an empty stomach, in the first half of the day; you are allowed to drink only clean, still water. To ensure that the results are not distorted, it is recommended not to drink alcohol or fatty foods the day before the analysis, and also to avoid physical and emotional stress. If you are taking blood thinning medications, you need to notify the clinic representative about this, he will note the data in the client’s card.
The best solution is to analyze the entire blood coagulation system: in addition to thrombin time, it is also recommended to take prothrombin time, fibrinogen and APTT. These indicators are basic and allow you to evaluate the curtailment process from all possible angles.
Blood is taken from a vein: specialists from the Evermedic medical laboratory perform the manipulations as carefully and quickly as possible, even if the veins are thin and deep. The research is carried out in a modern, equipped laboratory with powerful microscopes, so the results are ready within the first 24 hours. They can be received either in person or by email.
Content
- Blood clotting process
- Prothrombin time indicators
- Determination of prothrombin time according to Quick
- Methodology for studying prothrombin time
- Indications for prescribing prothrombin time analysis
- Prothrombin time indicators during pregnancy
The coagulation and anticoagulation systems of the blood determine the continuous flow of blood in the vessels, thereby ensuring all the vital functions of the body.
The anticoagulant system keeps the blood fluid, while the coagulation system prevents possible bleeding by forming blood clots.
Prothrombin time, PT
Shortening PV- activation of the extrinsic coagulation mechanism during various types of intravascular coagulation;
- last weeks of pregnancy, taking oral contraceptives;
- treatment with prothrombin complex factor concentrates
PV extension
- deficiency or anomaly of prothrombin complex factors (VII, X, V, II) in cases of taking indirect anticoagulants (warfarin, syncumar, pelentan, etc.);
- diseases of the liver and biliary system;
- treatment with unfractionated heparin (the test responds only to relatively high concentrations of the anticoagulant, approximately 0.5 IU/ml of blood and above);
- DIC syndrome (consumption of coagulation factors in the transition phase and hypocoagulation phase);
- against the background of transfusions of rheopolyglucin, hydroxyethyl starch preparations (infucol, valecam, HES);
- presence of lupus anticoagulant in the blood (possibly);
- defects in obtaining blood for research (hemolysis, overdose of sodium citrate, blood sampling from a heparinized catheter).
Expression forms for prothrombin time
Index
| Calculation | Note | Correlation | |
| Prothrombin time ( PT), sec | Plasma clotting time after adding thromboplastin-calcium mixture. | Does not allow for a comparative assessment of results in connection with the use of thromboplastins of different MI (see INR) | |
| Prothrombin index (PI), % | PT of normal control plasma (or average PT of normal range)/PT of patient plasma) x 100 | The test results depend on the sensitivity of the thromboplastin used. | Negative - with prothrombin ratio and INR |
| Prothrombin ratio (PR), % | Patient plasma PT/normal control plasma PT (or average normal range PT) x 100 | The test results depend on the sensitivity of the thromboplastin used. | Positive – with INR, negative – with prothrombin index |
| Prothrombin according to Quick (%) | Similar to PTI, but calculation is made depending on the concentration of prothrombin complex factors | The test results depend on the sensitivity of the thromboplastin used. | Negative – with CR and INR, coincides with PTI in the area of normal values |
| Prothrombin time expressed as INR | (PT of patient plasma/PT of normal control plasma (or average PT of normal range) | ISI (International Sensitivity Index) is an indicator of the sensitivity of thromboplastin relative to the international standard (indicated in the kit passport), which allows you to compare the results obtained using thromboplastin of different sensitivities. | |
The first three expressions, although presented in the form of numbers, are, due to the lack of calibration, essentially qualitative indicators with an indefinite scale. In addition, a significant drawback of determining prothrombin time in seconds is low reproducibility due to non-standardized thromboplastin. Therefore, it is impossible to compare results for one patient obtained in different laboratories, on different devices, or with test kits from different series. The expression of PTI as a percentage has no meaning and confuses doctors, since there is no direct proportional relationship between the number of factors and the measurement of PT in seconds. Prothrombin according to Quick and prothrombin time, expressed as INR, for PT are complementary. Quick's prothrombin (%), like the prothrombin index, allows you to determine the activity of the prothrombin complex of the patient's plasma in comparison with the measured prothrombin time of the control plasma. But in this case, the calculation is carried out according to the curve of the dependence of prothrombin time on the % content of prothrombin complex factors, constructed using different dilutions of control plasma. This way of presenting results is more accurate, especially in the low value range. The prothrombin index and Quick prothrombin may coincide with each other in the range of normal values. In the area of low values recommended for the management of patients taking indirect anticoagulants, the performance of these tests diverges. A prothrombin index of 50-60% may correspond to 30-40% prothrombin according to Quick. Calculation of prothrombin according to Quick is currently a generally accepted method.
INR (International Normalized Ratio ), Latin abbreviation INR (International Normalized Ratio) is an additional way of presenting the results of a prothrombin test, recommended for monitoring therapy with indirect anticoagulants by the WHO expert committee, the International Committee on Thrombosis and Hemostasis and the International Committee for Standardization in Hematology. INR is a mathematical correction that standardizes prothrombin time, which allows you to compare results obtained in different laboratories. INR and prothrombin according to Quick correlate negatively - a decrease in prothrombin according to Quick corresponds to an increase in INR.
To monitor the level of anticoagulants, WHO has developed the following recommendations:
| Clinical condition | Recommended INR |
| Prevention of primary and recurrent deep vein thrombosis and pulmonary thromboembolism | 2,5 (2,0-3,0) |
| Preoperative preparation: surgical interventions in the hip area | 2,0 (2,0-3,0) |
| All other surgical procedures | 2,5 (1,5-2,5) |
| Treatment of deep vein thrombosis, pulmonary thromboembolism and prevention of recurrent venous thrombosis | 3,0 (2,0-4,0) |
| Prevention of arterial thromboembolism, including in patients with prosthetic valves | 3,5 (3,0-4,5) |
Recommended levels of hypocoagulation when taking warfarin
- high INR from 2.5 to 3.0;
- average INR from 2.0 to 3.0;
- low INR from 1.6 to 2.0.
Blood clotting process
If we briefly describe the coagulation process, it will consist of the following phases:
- prephase or vascular-platelet hemostasis;
- prothrombinase;
- thrombin;
- fibrin;
- postphase, which consists of two parallel processes: retraction (reduction and thickening of the blood clot) and fibrinolysis (dissolution of the blood clot).
Thus, for the formation of a blood clot, several components are necessary: the vessel wall, blood elements, and the plasma blood coagulation system.
This process looks like this: damage to the vascular endothelium causes activation of enzymes of the coagulation system, which, in turn, forms fibrin threads, which are the framework for the formation of a blood clot.
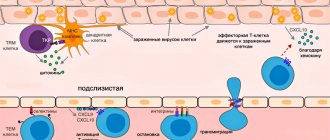
The coagulation system is activated in two ways:
1. External - when coagulation factors come into contact with damaged tissues outside the vessel.
2. Internal - associated with destroyed blood cells and damage to the endothelium, that is, the process starts inside the vessel itself.