The glucose tolerance test in professional terminology is simply abbreviated to the abbreviation “GTT”. Often, its help is resorted to in order to diagnose diabetes at different stages of its development in the laboratory.
But this is far from the only option for using it. Deviation from the norm according to the results of the presented study helps to identify possible fluctuations in blood glucose. Even healthy people, or those who want to control the dynamics of diabetes development at home, may need such an approach.
It is impossible to do without the presented intervention during pregnancy, which is especially important during long periods.
Doctors highly value this type of examination for its easy accessibility, and patients like the information content of the study. Having figured out how to take the test correctly, even children starting from the age of fourteen are allowed to take it. If the rules of the preparatory stage are followed, the laboratory assistant will be able to provide the most reliable and detailed result, where glucose will be measured without distorting factors.
Classification of glucose-tolerant techniques
Schematically, all presented clinical trial options can be divided into two camps. The first involves the oral approach, which is simply abbreviated as POGTT. The parenteral method is designated according to an identical principle, abbreviating its name to PNGTT.
Content:
- Classification of glucose-tolerant techniques
- Medical indications
- Medical contraindications
- Features of the event
- Procedure algorithm
- Norm and deviations
The second category involves intravenous modification. But, regardless of how biological material is collected for subsequent study in the laboratory, the preparatory rules remain virtually unchanged.
The difference between the two listed types lies in the route of administration of carbohydrates. We are talking about a glucose load, which is performed a few minutes after the first stage of blood sampling. In the oral version, preparation involves the mandatory ingestion of a clearly calculated dose of glucose. The doctor will be able to say exactly how many milliliters will be needed after a detailed assessment of the victim’s current condition.
The intravenous approach uses an injection format of administration. In this case, the dosage is calculated using the same algorithm. But this version is in little demand among doctors due to its relative complexity. It is resorted to only in situations where the patient is not able to drink sweetened water on his own.
Most often, such a radical measure will be needed if a person is in extremely serious condition. The same applies to pregnant women who show clear signs of severe toxicosis. This solution is suitable for those who have any disturbances in the normal functioning of the gastrointestinal tract.
So, in case of a diagnosed illness regarding the inability to normally absorb substances in the process of nutrient metabolism, one cannot do without an intravenous glucose load.
The price of the two types of procedure differs little from each other. Still, the patient is often asked to bring a glucose supply with him.
Normal GTT values
| Fasting glucose | 4.1 - 6.1 mmol/l |
| Glucose in 30 min. after glucose load | 4.1 - 7.8 mmol/l |
| Glucose after 60 min. after glucose load | 4.1 - 7.8 mmol/l |
| Glucose after 90 min. after glucose load | 4.1 - 7.8 mmol/l |
| Glucose after 120 min. after glucose load | 4.1 - 7.8 mmol/l |
C-peptide norms
- in the Invitro laboratory: 260-1730 pmol/l (0.78-5.2 ng/ml)
- in the Helix laboratory: 366-1466 pmol/l (1.1-4.4 ng/ml)
Important! Standards may vary depending on the reagents and equipment used in each particular laboratory.
That is why, when interpreting the results, it is necessary to use the standards adopted in the laboratory where the analysis was carried out. You also need to pay attention to the units of measurement. The following medications may affect your results:
- hormones and oral contraceptives,
- corticosteroids,
- lithium preparations,
- salicylates,
- metalirona,
- ascorbic acid.
Medical indications
Having figured out why such an analysis is done, people begin to wonder why they should undergo such a specific examination if they do not suffer from diabetes. But even a suspicion of it or a bad hereditary predisposition can become reasons for regular testing with a referral from a doctor.
If the therapist considers it necessary to issue a referral for diagnostics, then refusing it simply because of fear or the opinion that this is a waste of time is a bad idea. Doctors simply won’t subject their patients to a glucose load.
Often, prescriptions are prescribed by local doctors for characteristic diabetic symptoms, or by gynecologists or endocrinologists.
The group of those most likely to receive referrals includes those patients who:
- Type 2 diabetes is suspected and a more accurate diagnosis is required;
- for the first time prescribing or reviewing the current course of drug treatment associated with diagnosed diabetes mellitus;
- it is necessary to analyze the dynamics of treatment to exclude the possibility of a complete lack of effect;
- Type 1 diabetes is suspected;
- regular self-monitoring is required;
- gestational type of diabetes is suspected, or after actual detection for subsequent health monitoring;
- prediabetic condition;
- there are disruptions in the functioning of the pancreas;
- abnormalities in the functioning of the adrenal glands were recorded.
No less often, the reason for referral to a diagnostic room is confirmed metabolic syndrome. As evidenced by the reviews of some patients, they were sent to undergo the test for diseases associated with liver activity or ailments caused by malfunctions of the pituitary gland.
A test of this kind cannot be avoided if a person has been diagnosed with impaired glucose tolerance, as well as simply people suffering from varying degrees of obesity. They are guided by nutritionists to further build an individual program of rational nutrition and physical activity.
If, during the study of the hormonal background of the body, if endocrine abnormalities are suspected, it turns out that these indicators are far from normal, then without a glucose tolerance test the final verdict will not be given. As soon as the diagnosis is officially confirmed, you will have to come to the diagnostic room on an ongoing basis. This will allow self-monitoring to insure against deterioration of well-being.
Due to the fact that not all patients know where to take such a test, they turn to pharmacists with a request to purchase portable biochemical analyzers. But experts remind us that primary diagnosis should still begin with a detailed analysis obtained in laboratory conditions.
But for self-monitoring, mobile glucometers are a great idea. Almost any pharmacy can offer several options from global manufacturers, the models of which differ in functionality.
But there are also some nuances here:
- home devices analyze only whole blood;
- they have a larger error than stationary equipment.
Against this background, it becomes clear that it will not be possible to completely avoid going to the hospital. Based on the officially documented information received, the doctor will subsequently make a decision on adjusting the therapeutic program. Therefore, if before purchasing a portable device a person may still think about whether such a step is mandatory or not, then this does not happen with a hospital examination. It is necessary to review a previously approved treatment program.
For home use, the simplest appliances will do just fine. They are capable of not only detecting glycemic levels in real time. Their responsibilities include calculating the volume of glycated hemoglobin, which will be marked on the device screen with the designation “HbA1c”.
How is carbohydrate metabolism disorder diagnosed during pregnancy?
Stage 1 . When a pregnant woman first visits a doctor up to 24 weeks, the level of fasting venous plasma glucose is assessed:
- result
- with fasting venous plasma glucose ≥ 5.1 mmol/L (92 mg/dL), but
- when the fasting venous plasma glucose level is ≥ 7.0 mmol/l (126 mg/dl), a preliminary diagnosis of manifest (newly diagnosed) diabetes mellitus (DM) is established.
According to some recommendations, if a pregnant woman is at risk for developing gestational diabetes (GDM), then an OGTT with 75 g of glucose is carried out immediately upon registration, and if the result is negative, again at 24-28 weeks.
Stage 2 . All women who have not been diagnosed with carbohydrate metabolism disorders in early pregnancy undergo an OGTT with 75 g of glucose between 24 and 28 weeks of pregnancy.
Medical contraindications
Despite the fact that for most patients the analysis does not pose any threat, it still has several significant contraindications. Among them, in the first place is individual intolerance to the active substance, which can provoke a severe allergic reaction. In the worst case scenario, this can result in almost instantaneous anaphylactic shock.
Among other phenomena and conditions that pose a potential danger when conducting a glucose tolerance study, note:
- diseases associated with the gastrointestinal tract, which most often concerns exacerbation of chronic pancreatitis;
- acute stage of the inflammatory process;
- untreated infectious lesion of any origin, distorting the accuracy of the clinical picture;
- toxicosis with severe manifestations;
- postoperative period.
Separately, situations with patients who should, for some reason, be kept in bed are considered. Such a ban is more of a relative nature, which means that an examination can be carried out if its benefits outweigh the harm.
The final decision is made by the attending physician according to the circumstances.
Features of the event
Whatever method of measuring glycemia is approved by the treating specialist, it may provide unreliable information. Most often, the cause of false data is the carelessness of the victim himself. In order for the results to reflect what is happening in the body as accurately as possible, you will need to follow simple preparatory rules.
Most of all, patients are interested in the fact whether breakfast affects the reliability of information. But coming to the diagnostic room on an empty stomach is the key to success. Even eating light food can distort the truth, let alone tea with sugar.
Other tips on how to prepare properly include the following:
- refusal to drink alcoholic beverages in any quantity even on the eve of the planned reception;
- smoking, which for the purity of the experiment should be excluded at least from the evening of the day before the examination;
- sudden physical activity that is not typical for the body at the usual pace of life;
- staying hydrated and avoiding sugary foods along with other eating habits.
Often indicators are distorted by various stressful situations. Moreover, we are talking not only about a nervous breakdown or one-time emotional overload, but about accumulating stress due to the unfavorable environment around.
In the instructions on how to correctly carry out the diagnostic procedure, there is a separate line warning about the need to first cure a runny nose, flu or a common ARVI. Only after the destruction of the source of infection will it be possible to achieve complete reliability.
Donation is strictly contraindicated for patients who have been prescribed specific medications. This usually applies to patients in mental health clinics who are prescribed medications with glucose-lowering substances or hormonal drugs.
It would also be appropriate to warn the doctor in advance that the person is susceptible to certain other chronic diseases or has a hereditary predisposition to fluctuations in blood sugar.
Regardless of what stage of pregnancy a woman goes to check her glycemic limits, there is always a risk of getting a falsely elevated result. This is explained by physiological changes that occur in her body too quickly.
Despite this, such a test does not pose any harm to the fetus if it is carried out strictly according to the indications and according to the protocol.
General information
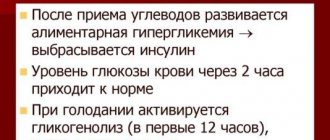
Glucose is a simple carbohydrate that enters the body with regular foods and is absorbed into the blood in the small intestine. It provides the nervous system, brain and other internal organs and systems of the body with vital energy. For normal well-being and good productivity, glucose levels must remain stable. Its level in the blood is regulated by pancreatic hormones: insulin and glucagon. These hormones are antagonists - insulin reduces sugar levels, and glucagon, on the contrary, increases them.
Initially, the pancreas produces a molecule called proinsulin, which is divided into 2 components: insulin and C-peptide. And if insulin remains in the blood for up to 10 minutes after secretion, then C-peptide has a longer half-life - up to 35-40 minutes.
Note: until recently, it was believed that C-peptide has no value for the body and does not perform any functions. However, the results of recent studies have revealed that C-peptide molecules have specific receptors on their surface that stimulate blood flow. Thus, determination of C-peptide levels can be successfully used to detect hidden disorders of carbohydrate metabolism.
Procedure algorithm
The manipulation itself is not particularly difficult to implement. The only problem is the duration, since you have to spend about two hours. The reason that affects such long periods is the variability of glycemia. Here we also have to take into account the performance of the pancreas, which does not function properly in all subjects.
The scheme of how testing is done includes three stages:
- fasting blood sampling;
- glucose load;
- re-fence.
The first time blood is collected after the patient has not eaten for at least 8 hours, otherwise the reliability will be blurred. Another problem is over-preparing, when a person literally starves himself the day before.
But, if the last meal was more than 14 hours ago, then this turns the selected biological material unsuitable for further study in laboratory conditions. Because of this, it is most productive to go to your appointment early in the morning without eating anything for breakfast.
At the glucose loading stage, the patient must either drink the prepared “syrup” or receive it through an injection. If the medical staff preferred the second method, then they take a 50% glucose solution, which has to be administered slowly for about three minutes. Sometimes the victim is diluted with a solution containing 25 grams of glucose. A slightly different dosage is recommended for children.
With alternative methods, when the patient is able to ingest the “syrup” himself, 75 grams of glucose is diluted in 250 ml of warm water. For pregnant women and children, the dosage varies. If a woman practices breastfeeding, then she should also consult with a pediatrician in advance.
People who suffer from bronchial asthma or angina pectoris deserve special attention. It is easier for them to consume 20 grams of fast carbohydrates. The same applies to those who have suffered a stroke or heart attack.
The active substance is taken as the basis for the solution not in ampoules, but in powder. But even after the patient finds it in the pharmacy in the required quantity, it is strictly prohibited to independently carry out a glucose load at home. This can lead to serious complications.
The final stage involves repeated sampling of biological material. Moreover, this will be done several times within one hour. This is a forced measure aimed at determining physiological fluctuations in blood composition. Only by comparing several results will it be possible to paint the broadest possible laboratory picture.
The verification mechanism is based on the action of carbohydrate metabolism. The faster the components of the “syrup” that enters the body are consumed, the sooner the pancreas copes with them. When it turns out that the “sugar curve” after exposure to carbohydrates continues to remain almost at the same level for the next few samples, this is a bad sign.
At best, this indicates prediabetes, which needs urgent correction to prevent progression.
But experts remind that even a positive answer is not a reason to panic. All the same, in case of any deviations from the norm, a repeat test will have to be carried out. Another key to success should be correct decoding, which is best entrusted to an experienced endocrinologist with experience.
If, even after several repeated attempts, I demonstrate an identical result, the doctor may send the patient to undergo related diagnostics. This will allow you to accurately determine the source of the problem.