Loss of consciousness is possible in completely healthy people and in the presence of various diseases of the cardiovascular, nervous, endocrine and musculoskeletal systems. But most often this condition is associated with dysregulation of blood pressure. Let's figure out at what pressure people faint and what to do in such cases.
- What is fainting?
- At what pressure do you faint?
- How to provide assistance?
- Other causes of fainting
- Vascular syncope
- Cardiac fainting
- Neurological syncope
- Fainting due to metabolic disorders
What is fainting?
Fainting is a sudden and brief loss of consciousness. Regardless of the cause, its development is based on a temporary disruption of blood flow to the brain. The work of nerve cells is directly related to the intensity of their blood supply. The intensity of metabolic processes in neurons is one of the highest in the human body. Therefore, a decrease in blood flow for seconds leads to disruption of their work. This is accompanied by loss of consciousness. About 3% of men and 3.5% of women have fainted at least once in their lives.
Before a person loses consciousness, a presyncope occurs:
- At this moment, victims feel severe weakness, dizziness, constantly increasing noise or ringing in the ears, some describe these sounds as the roar of a crowd.
- Visual effects appear like spots in front of the eyes.
- Nausea appears, but vomiting is extremely rare.
- There may be an unbearable feeling of anxiety, fear of death, a feeling of lack of air, numbness of the face and hands.
- Immediately before losing consciousness, victims complain of weakness in their legs, describing this with the phrases “the ground is collapsing”, “woolly legs”.
Visually, people in a pre-fainting state look pale, their gaze does not focus, and their skin becomes covered in cold sweat. This period lasts seconds. Fainting actually occurs.
In a faint, a person is unconscious. The duration of this state is no more than a few minutes. The patient is pale, the skin is covered with large drops of cold sweat, and due to a significant decrease in muscle tone, the raised limbs fall like whips. The radial pulse is weak. Blood pressure during fainting is low - less than 90/60 mm Hg. Art. Sometimes urination and bowel movements occur. The pupils are dilated and react sluggishly to light. It is fundamentally important that the reaction to light is preserved, although weakened, and the pupils are the same size. If they do not narrow from the light, then this is not fainting, but a more serious condition - clinical death or deep coma. Different diameters of the pupils indicate damage to the brain substance and are observed with hemorrhages under the meninges.
The victim remains in the post-fainting period for several minutes. Muscle weakness, dizziness and headache persist, and nausea may occur. It is important to clarify whether the patient remembers what preceded the fainting, whether he orients himself in space, and whether he recognizes those around him. This is necessary for differentiation from more severe pathological conditions in which the brain is affected (concussion, bruise).
At what pressure do you faint?
Loss of consciousness is possible at any pressure. In relatively healthy individuals, it is more often observed when it sharply decreases to 90/50 mm Hg. Art. A drop in pressure is possible during a sudden transition from a horizontal to a vertical position (orthostatic hypotension), or during fasting. Against the background of intoxication and increased body temperature, vasodilation and blood redistribution occur. In this case, the risk of pressure drop increases. People suffering from hypertension may faint at high blood pressure.
A significant increase in blood pressure (above 200 mm Hg) or loss of consciousness with high blood pressure should alert both the patient and others. This condition may be a manifestation of a stroke.
How to provide assistance?
In a pre-fainting state, it is necessary to lay the victim on a horizontal surface (it is advisable to raise the legs so that they are at an angle of 30-45° to the horizon) and provide access to fresh air, remove constricting clothing, and allow the ammonia vapor to be inhaled.
If loss of consciousness has already occurred and there is a possibility, you need to restrain the victim. This is necessary to prevent injury during a fall. Lay on a horizontal surface in a position with legs raised. Spray cold water on your face. Bring a cotton swab moistened with ammonia to your nose. Call an ambulance.
Among medications, Caffeine, Cordiamine or Mezaton are usually used:
- Caffeine has a stimulating effect on the vasomotor and respiratory centers. Leads to increased heart rate and increased blood pressure.
- Mezatone affects the tone of peripheral vessels. Under its influence, arterioles narrow, which leads to increased blood pressure.
Other causes of fainting
In most cases, fainting occurs in people suffering from hypertension or hypotension. Falls in blood pressure are especially dangerous in people with hypertension in the event of an overdose of antihypertensive drugs. In such people, the vascular system is adapted to high blood pressure. Low blood pressure leads to serious disruptions in the functioning of internal organs. Other common causes of fainting are:
- vascular dysfunction;
- heart pathology;
- diseases of the nervous system;
- metabolic disorders.
Vascular syncope
In the nature of the development of fainting, vascular pathology is the most common - accounting for about 1/3 of all cases. Most often, fainting occurs during a sudden transition from a horizontal to a vertical position. This type of fainting is called orthostatic.
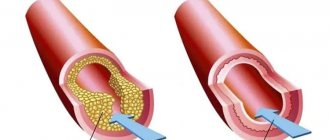
There are several possible mechanisms for the development of vascular syncope. If the vessel wall is damaged, for example, by an atherosclerotic process, blood circulation in the internal organs may be impaired. If the lesion affects the vessels supplying the brain, then fainting conditions are common in such individuals.
A specific variant of vascular syncope is reflex-induced fainting. For their occurrence, irritation of certain reflex zones is necessary. For example, when performing dental procedures, there may be irritation of specific areas of the oral mucosa, which is accompanied by a reflex increase in the tone of the parasympathetic nervous system, dilation of peripheral vessels and a drop in pressure.
Sometimes there may be fainting while swallowing food or water, while urinating or having a bowel movement.
Cardiac fainting
Loss of consciousness is possible if there is a sudden appearance of an obstruction to the flow of blood from the heart or due to a rhythm disturbance.
Obstructions to cardiac output are most often associated with congenital or acquired malformations, in which the lumen of the efferent vessels (aorta or pulmonary artery) narrows. Fainting is often observed in people with cardiomyopathy, a disease in which excessive thickening of the walls of the muscular lining of the heart occurs as it exits the ventricular cavity. At rest, the well-being of people with such diseases is little affected. But during physical activity, the heart, due to obstruction to blood flow, cannot provide the required amount of blood flowing to the brain. Loss of consciousness develops.
Rhythm disturbances that occur suddenly reduce the efficiency of the heart. Irregular contractions or lack of coordination between different parts of the heart reduce the amount of blood pumped out during systole. There is circulatory failure in the brain and fainting.
Neurological syncope
Loss of consciousness may be associated with a transient cerebrovascular accident. This can be observed with pathology of the vertebral vessels or carotid arteries, when they are not able to supply the brain matter with a sufficient amount of blood.
Less commonly, fainting occurs due to pathology of the brain substance itself. With some developmental anomalies (Chiari syndrome), a peculiarity of the structures of the brain stem is observed, some of which are compressed by the surrounding tissues and bones of the skull. In this case, fainting may occur for no apparent reason.
Loss of consciousness is often observed in people suffering from migraines. At the height of pain, a reflex expansion of peripheral vessels and a drop in blood pressure are possible. Most often, fainting occurs with the simultaneous presence of migraine and hypertension.
Fainting due to metabolic disorders
During psycho-emotional arousal, breathing becomes more frequent and deepening. The amount of oxygen supplied exceeds the body's need for it. Hypocapnia develops (a decrease in the concentration of carbon dioxide in the blood, which is the main irritant of the respiratory center), and the activity of the vasomotor center is suppressed. There is a sharp expansion of the peripheral vessels, pressure drops, and fainting occurs.
During fasting, against the background of significant and prolonged physical activity, in patients with diabetes mellitus, with an incorrectly selected dose of medications or untimely consumption of food, hypoglycemia may occur - a decrease in blood glucose levels. Glucose is used by brain cells as an energy resource. When its concentration decreases, the activity of the centers that regulate vascular tone and respiration is suppressed.
Before hypoglycemic loss of consciousness, a feeling of anxiety, trembling fingers, and severe hunger appear. After a few minutes, loss of consciousness occurs, which can last for hours until medical attention is provided.
Any episode of fainting is an indication to see a doctor. Especially if this happened for the first time or is repeated often. There may be serious health problems behind such situations that need to be diagnosed and addressed as early as possible.
Causes of fainting
Cardiovascular diseases
Syncope associated with cardiac output obstruction
- aortic stenosis
- mitral stenosis
- hypertrophic cardiomyopathy
Syncope associated with cardiac arrhythmia
Dysregulation of vascular tone and blood volume
- reflex syncope - neurocardiogenic (vasovagal) syncope
- carotid sinus hypersensitivity
- situational syncope (coughing, sneezing, swallowing, urination, defecation, orthostatic instability syndromes)
Primary causes of autonomic failure:
- True autonomic failure
- Multiple system atrophy
- Postural otostatic tachycardia syndrome
- Acute autonomic failure
Secondary causes of autonomic dysfunction
- additional causes of orthostatic instability
Other causes of fainting
- Hypoglycemia
- hyperventilation
Subclavian steal syndrome
- decrease in circulating blood volume
- Carcinoid
- medications
Multifactorial syncope (more common in older patients)
The basis of the clinical diagnosis of syncope is a carefully collected history, which is sometimes absent due to the presence of retrograde amnesia in the patient, especially in elderly patients.
What could be the causes of arterial hypotension? Could stress have any effect on this?
– A sharp decrease in blood pressure can occur in various acute conditions, such as shock, myocardial infarction, blood loss, trauma, burns.
Chronically low blood pressure occurs when:
- adrenal insufficiency;
- hypothyroidism;
- taking certain medications (antidepressants, muscle relaxants, nitroglycerin, Viagra);
- heart defects;
- chronic heart failure;
- severe anemia;
- change in body position from horizontal to vertical (orthostatic hypotension);
- after meals (postprandial hypotension) in elderly people;
- patients with Parkinson's disease;
- after surgery to remove part of the stomach.
Hypotension may also be a variant of the individual norm (if there is no pathology).
People react to stress differently. And yes, one of the reactions to stress and irritation can be a reflex decrease in pulse, blood pressure, even fainting.
A patient with syncope should be asked the following questions:
- At what age did you first faint, and how often do you faint?
- How long did it take from the moment you realized that “something was wrong” with you until you lost consciousness? This is a key question that will allow us to assess the course of the prodromal period.
- What were you doing when the symptoms appeared? What position were you in: lying, sitting, standing, in motion?
- What sensations did you experience before losing consciousness - nausea, fullness in the stomach, increased salivation, sweating, flushing, feeling hot or cold, sudden yawning, tingling or numbness in the arms and legs, flashing “floaters” before the eyes or distorted perception, spots before the eyes ?
- Did you feel any smells, sounds, or visual distortions before you lost consciousness? Were you injured during the fall?
- Did you feel dizzy, nauseous during injections or taking blood for analysis?
- Do you get motion sickness in transport?
- Did you understand what happened to you when you woke up?
- During fainting, did you bite your tongue or cheek, did you feel weakness in half of your body after waking up, did you experience urinary or fecal incontinence during the attack?
It is also important to ask questions to the witness of the syncope, especially when seeing an elderly patient with retrograde amnesia, such as:
- What did the patient complain about before he lost consciousness?
- How long was the patient unconscious?
- Did you have any convulsions while you were unconscious?
- did the patient make involuntary sounds during loss of consciousness?
- did the patient wet himself or lose stool?
- Was the patient tense or, conversely, lethargic at the time of loss of consciousness?
- did the patient look deathly pale, with a gray or sallow complexion?
- Did you quickly realize what happened after waking up, or was you disoriented and paralyzed?
These features of the anamnesis, obtained from the patient and from the witness, make it possible to most accurately identify the cause of fainting.
Giving help
Algorithm for helping an unconscious patient:
If possible, try to support the person to avoid injury due to a fall.- Laying the person on their side will help keep the airway open.
- Elevate your legs if possible.
- Remove the victim from tight clothing.
- Sprinkle your face with water, rub your ears and cheeks.
- Bring ammonia to your nose.
- Determine the patient's pulse and blood pressure.
- If the above steps do not help, call an ambulance.
How can you prevent syncope?
- Lead a healthy lifestyle.
- Get rid of bad habits.
- Avoid stress.
- Do not move to a sitting or standing position too quickly or abruptly.
- Do physical education.
- If presyncope symptoms occur, sit or lie down with your legs elevated. Unbutton your clothes. Wash with water. Eat sweets.
- If high blood pressure is determined to be a common cause of fainting, then you need to take pills prescribed by your doctor to lower it or seek medical help. Self-prescribing medications and adjusting their dosage can be dangerous, as they can sharply lower blood pressure.
If an underlying disease is identified as the cause of syncope, treatment should be taken seriously.
Neurocardiogenic or vasovagal syncope
This type of fainting is characterized by a young age of onset of the disease, multiple repetitions of episodes of loss of consciousness over many years. The patient mentions a tendency to motion sickness and lightheadedness at the sight of blood. Most often, such fainting occurs in warmth, at rest, after physical exertion. It begins in a standing or sitting position, never lying on your back. The prodromal period usually lasts from 30 seconds to several minutes and includes symptoms such as nausea, possibly vomiting, abdominal discomfort, a feeling of heat, cold sweats, a feeling of flushing, dizziness, an increasing feeling of lightheadedness leading to loss of consciousness. Such fainting usually does not lead to bodily harm or injury. Changing to a horizontal position can interrupt the loss of consciousness. Witnesses note marked lethargy and describe how the patient “slipped” to the floor during the attack. There is no disorientation or paralysis upon awakening. There may often be a feeling of extreme fatigue that lasts for several hours.
Symptoms
Clinical symptoms of the period before syncope:
- pale, bluish skin;
- cold sweat;
- tachycardia;
- lack of orientation in space;
- numbness of the limbs, lack of sensitivity.
During the period of fainting, the signs change:
- the skin takes on a gray tint;
- weak pulse, muscle tone;
- pupils dilated;
- there is no consciousness.
If the condition is caused by fainting, it takes 5 to 30 seconds for the person to return to consciousness.
Make an appointment with a neurologist
Arrhythmic syncope
As a rule, these are patients over 60 years of age with a history of heart disease. Loss of consciousness occurs suddenly, with a minimal prodromal period (“I found myself lying on the floor”) and is often accompanied by physical injuries (fractures, cuts) and even an accident if the attack occurs while driving a car. The duration of the attack does not exceed 30-40 seconds.
Fainting due to congenital arrhythmic syndromes - the so-called channelopathies - is characterized by young age, a family history of sudden death in other family members, spontaneous miscarriages, sudden infant death. Loss of consciousness associated with fright, swimming (drowning), surprise. Fainting in males during physical activity, after eating a high-carbohydrate meal or poor sleep should raise suspicion of Brugada syndrome.
During epileptic seizures, from which it is very important to differentiate syncope, a typical aura occurs in the form of visual, olfactory, auditory sensations, often the same before each attack. Deja vu or jamevu. Personal injury is very common. Accompanied by fecal and urinary incontinence. Those around describe prolonged tonic-clonic convulsions, starting with stiffness, turning into lethargy, and note a turn of the head to the side during loss of consciousness. There is a bite of the tongue and cheeks. After the attack, there is confusion, disorientation, inability to remember events, and neurological deficits or paralysis of one side (Todd's palsy) often persist.
After collecting anamnesis, we perform a medical examination, during which we note the presence of injuries and physical injuries, which often indicate the presence of either cardiac pathology or the epileptic nature of the attack. Blood pressure is measured while lying on your back, sitting and standing for 30 seconds and after 2 minutes in a standing position, which helps to identify postural changes in pressure - orthostatic collapse. Pressure measurements must be taken on both sides to avoid missing aortic dissection. Heart examination - assessment of pulse, cardiac impulse, systolic ejection murmur at the base of the heart - to identify cardiogenic pathology. Also an important diagnostic technique is carotid sinus massage, which is carried out by applying pressure to the carotid artery high in the neck at the angle of the lower jaw for 5 seconds while continuously recording an ECG. After 30 seconds, similar events are carried out on the other side. A result is considered positive when provoking a pause of 3 seconds leads to the reproduction of clinical symptoms.
Along with a thorough medical examination, a 12-lead ECG is necessary. This completes the triplet, allowing a reliable diagnosis of fainting to be made. Additionally, the ECG allows you to predict the further development of events and the patient’s management tactics. Based on the data obtained, the doctor must determine whether the fainting event is an interrupted episode of sudden death or this condition is not life-threatening for the patient. This prediction is more important, even than making a diagnosis.
You can get advice from highly qualified specialists on the treatment of fainting in Samara at the specialized neurological clinic First Neurology, which is staffed by a neurologist, cardiologist, epileptologist and functional diagnostics doctor.
The diagnostic examination includes a study of biochemical blood tests, ECG, ultrasound of the heart, and, if necessary, Holter, EEG to exclude epilepsy.
We are waiting for you at one of the three clinic addresses.
What is low blood pressure anyway?
Blood pressure is the force with which blood pushes against the walls of the arteries. At the moment when the heart contracts, the pressure is highest - it is called upper, or systolic. In the interval between heartbeats, the pressure in the vessels drops - it is called lower, or diastolic.
Normal blood pressure ranges from 90/60 to 120/80 mmHg. The numbers 90 and 120 indicate systolic pressure, and 60 and 80 indicate diastolic pressure. If the readings are less than 90/60, the blood pressure is considered low. This condition is called hypotension.
Our specialists
Tarasova Svetlana Vitalievna
Expert No. 1 in the treatment of headaches and migraines. Head of the Center for the Treatment of Pain and Multiple Sclerosis.
Somnologist.
Epileptologist. Botulinum therapist. The doctor is a neurologist of the highest category. Physiotherapist. Doctor of Medical Sciences.
Experience: 23 years.Derevianko Leonid Sergeevich
Head of the Center for Diagnostics and Treatment of Sleep Disorders.
The doctor is a neurologist of the highest category. Vertebrologist. Somnologist. Epileptologist. Botulinum therapist. Physiotherapist. Experience: 23 years.
Bezgina Elena Vladimirovna
The doctor is a neurologist of the highest category. Botulinum therapist. Physiotherapist. Experience: 24 years.
Dyachenko Ksenia Vasilievna
Head of the center for the treatment of dizziness and balance disorders.
The doctor is a neurologist of the highest category.
Angioneurologist. Neurorehabilitation specialist. Physiotherapist. Candidate of Medical Sciences.
Experience: 19 years.Drozdova Lyubov Vladimirovna
The doctor is a neurologist. Vertebroneurologist. Ozone therapist. Physiotherapist. Experience: 17 years.
Zhuravleva Nadezhda Vladimirovna
Head of the center for diagnosis and treatment of myasthenia gravis.
The doctor is a neurologist of the highest category. Physiotherapist. Experience: 16 years.
Palagin Maxim Anatolievich
The doctor is a neurologist. Somnologist. Epileptologist. Botulinum therapist. Physiotherapist. Experience: 6 years.
Mizonov Sergey Vladimirovich
The doctor is a neurologist. Chiropractor. Osteopath. Physiotherapist. Experience: 8 years.
Romanova Tatyana Alexandrovna
Pediatric neurologist. Experience: 24 years.
How to monitor your blood pressure and control its reduction?
– In order to prevent another decrease in blood pressure, it is necessary, firstly, to determine the cause (hypothyroidism, anemia, adrenal insufficiency, taking high doses of antihypertensive drugs, etc.) and, if possible, eliminate it.
Secondly, try to avoid provoking situations and factors , observe safety conditions during verticalization, and lifestyle recommendations.
And in situations where a person anticipates developing hypotension or fainting (increased sweating, nausea), you can help yourself by using the physical counterpressure maneuvers that I described earlier.
Reproduction of CityDog.by materials is possible only with the written permission of the editors. Details here.
Read also
Pelvic pain
Pelvic pain is pain in the muscles that form the pelvic floor and organs located in the small pelvis, caused by microtrauma, chronic deformation of the sacrococcygeal region due to anatomical…
Read more
Vertebral artery syndrome
The main vascular highways carrying blood to the brain pass in the neck - these are two carotid and two vertebral arteries. A decrease in blood flow through the vertebral arteries will lead to the development of acute...
More details
Syringomyelia
Syringomyelia is a disease caused by the formation of spaces in the substance of the spinal cord filled with cerebrospinal fluid. They expand the spinal cord at the level of the lower cervical and thoracic regions...
More details
Hepatic encephalopathy
Hepatic encephalopathy is a brain lesion that occurs against the background of liver pathology and is caused by liver failure. There is acute hepatic encephalopathy, which occurs on…
More details
Pinched nerve
This morning you arrived at your country house. While taking out a heavy and large bag of tools from the trunk of your car, you suddenly felt a very strong, shooting pain in your lower back on the right side. Raise...
More details
What foods can help with low blood pressure, and which ones should not be consumed?
– For low blood pressure, as I said earlier, it is recommended to consume large amounts of table salt (up to 10 g/day) and liquids (up to 3 l/day), and caffeine-containing drinks.
With postprandial hypotension, you need to adhere to a certain type of diet: eat often, in small portions, more proteins and fats, avoid carbohydrates (especially refined ones), eat warm or cold (not hot) foods. And you should give up alcohol.