Since childhood, we have all become accustomed to the fact that in order to obtain any certificate, diagnose a simple or complex disease, or undergo a preventive examination, it is necessary to take a finger blood test. This is one of the most common diagnostic procedures. This is due to the fact that any problems that arise in our body lead to changes in the composition of the blood, and taking it from a finger is much simpler and safer than taking a sample of fluid from a vein using a medical syringe. The event, which is carried out by specialists in laboratories today, is called a clinical blood test (CBC), but almost all doctors and patients are accustomed to the name general blood test (CBC), especially since there is no difference between them.
The versatility of finger prick blood testing
As you know, blood is “responsible” for the supply of oxygen and other nutrients to all organs and tissues of the human body. Therefore, any, even minor, deviation from the norm is reflected in the composition of the blood. OAC is the most accessible, easy-to-perform procedure that allows you to quickly and reliably assess the functioning of all organs and systems. Each clinic has its own laboratory, where it is performed absolutely free of charge. Many serious diseases do not show any symptoms for a long time, making their diagnosis and subsequent treatment difficult. Therefore, you need to undergo examination regularly.
A general blood test is not only the simplest and most reliable, but also a universal diagnostic method. It is used for:
- identifying hidden pathologies;
- carrying out preventive examinations;
- monitoring and assessing the patient’s condition during the treatment of a serious, chronic, incurable disease;
- before and after surgery;
- for acute diseases, burns.
Based on the results of the analysis, you can assess the general condition of the body, adjust the prescribed treatment, and so on.
At the same time, the OAC does not allow one to obtain an unambiguous answer to the question of which organ is functioning incorrectly. Various pathologies and diseases can lead to the same change in blood composition. Therefore, having received the results of the testing, the attending physician can only make an assumption about the presence of any disease from a whole list of possible problems. To specify the pathology, more thorough examinations will be required, specific to each of the possible diseases, taking into account the existing symptoms (clinical manifestations).
That is, a general blood test provides such a complete picture, so much information, that in order to make a more accurate diagnosis, in most cases it is necessary to conduct additional examination of the body. But the combination of a number of deviations of parameters from the norm (glucose level, hemoglobin concentration, number of different cells), taking into account other symptoms, allows us to make an assumption about the presence of one of a wide range of diseases:
- an insufficient number of red blood cells, hemoglobin in combination with a lack of iron is a sign of anemia;
- based on the ratio of the number of leukocytes in the sample and the erythrocyte sedimentation rate (ESR), one can assume the presence of an inflammatory process, an infectious, allergic disease, as well as possible genetic, chromosomal, genomic pathologies;
- the presence of abnormal cells in the biomaterial is one of the signs of leukemia;
- exceeding the normal amount of hemoglobin and red blood cells indicates possible diseases of the lungs, heart, liver, kidneys;
- the first assumptions about the presence of such a complex and very common disease as diabetes mellitus can be made by determining the level of glucose in the blood; of course, these data alone will not be enough; additional research will be required. But a finger prick blood test allows you to monitor the condition of such patients; many of them do this on their own using a special device - a glucometer, which does not do a complete blood test, but only evaluates the sugar level.
But to establish an accurate diagnosis, a more thorough examination will be required, taking other biomaterials for analysis, performing an ultrasound, taking a tomogram, electrocardiogram, and so on. Only the doctor will determine which procedures will be required in a particular case.
Where to submit?
Doubts regarding your health sooner or later make you wonder how and where to take a general blood test.
The answer to this question depends on the patient's requirements and capabilities. There are three possible options:
- State clinic,
- Private clinic,
- Medical personnel visiting your home,
In the first case, the diagnostic procedure is carried out within the framework of health insurance. The analysis is absolutely free . The disadvantages of donating blood at a government institution include long queues and the procedure being carried out at a strictly fixed time. It takes more time to examine a blood sample, which cannot be said about private clinics.
You can take the test at a paid institution at any convenient time. The main condition is not to eat for more than 3 hours. It costs more to have a medical professional visit your home. The advantages of the service include the absence of the need to leave the walls of the house, which is especially important if the patient is seriously ill.
Preparing for analysis
Taking blood from a finger is such a simple, “harmless” procedure that there are absolutely no contraindications for its use. However, in some cases, if the patient has diseases such as low blood clotting, low blood pressure, other pathologies, as well as severe agitation, biomaterial is taken in a hospital setting. After the procedure, the person remains under the supervision of medical personnel for some time, which helps to avoid negative consequences.
In order for the results obtained as a result of testing to be as accurate, reliable and informative as possible, the body must prepare for the test.
- A few days before the scheduled procedure, it is recommended to exclude smoked, fried and fatty foods from the diet. Lipid-rich foods (fatty) cause turbidity in the plasma, making microscopy difficult.
- The reliability of the results is affected by the presence of alcohol in the blood. Ethanol affects the membrane of red blood cells, dissolving it, which leads to their immobility and a decrease in hemoglobin levels. However, it should be remembered that ethanol is completely eliminated from the body approximately 3 weeks after administration. Knowing in advance about the upcoming procedure, it is necessary to stop drinking alcoholic beverages as early as possible.
- Sports training and other physical activity lead to an increase in the level of red blood cells by almost 10%, and the number of other components in the blood (leukocytes, platelets) also increases. Therefore, you should also refrain from playing sports on the eve of donating blood from your finger.
- The substances contained in tobacco smoke also affect the composition of the blood: they reduce the number of leukocytes and increase the concentration of red blood cells. You must quit nicotine at least 1 hour before submitting the material.
- Stressful conditions and high psycho-emotional stress reduce the level of leukocytes. Based on research data conducted at this time, the doctor may not detect the presence of an inflammatory process.
- A few days (from 2 to 4) before the date of donating blood for analysis, you must stop taking medications. If this is not possible due to the complexity of the disease, the impossibility of interrupting or suspending the course of treatment, the patient must warn the attending physician about which medications are being taken.
- For women, the period of menstruation is a complex physiological process leading to changes in blood composition, so at these moments you should refuse to donate blood for OAC.
- Biomaterial is collected in most cases in the morning. Therefore, the patient should skip breakfast. It is better to donate blood on an empty stomach. It is especially difficult to adhere to this rule when it comes to children. It is necessary to explain as convincingly as possible to the baby the need to suffer a little hunger, and tell him about the importance of the upcoming procedure. You can take some snacks with you: juice, yogurt, fruit, cookies and feed your child after the blood is drawn.
After receiving a referral to submit biomaterial for OAC, in the presence of serious pathologies or abnormalities in the functioning of the body, you need to discuss with your doctor the specifics of the procedure in this particular case.
What is a lancet?
When piercing the skin with a scarifier, the laboratory assistant applies a certain physical force. At the same time, it is not always possible to correctly calculate the depth of needle penetration. Therefore, the procedure was often accompanied by pain. And if an adult simply felt discomfort, then taking blood for analysis caused panic in some children, sometimes even leading to hysteria.
Today, adult and children's scarifiers have almost completely replaced new, easy-to-use devices - lancets. The name of this accessory is taken from the German language. Here "lanzette" is a diminutive of "lance", which translates as "spear". The devices are automated and are activated when a special button is pressed or upon contact with the skin. A very thin needle penetrates painlessly under the skin. Sterility is ensured by a removable plastic cap. Lancets are disposable devices. Manufacturers specially make them in such a way that unscrupulous workers, trying to save even on such little things, cannot reuse them.
Carrying out the procedure
Conducting an OAC is a common study. Taking the amount of biomaterial required for analysis is not difficult for either the laboratory assistant or the patient. The procedure is worked out to the smallest detail and consists of several mandatory steps.
- The patient takes off his outer clothing outside the office. In order for blood to flow freely from the wound, you need to keep your fingers warm, so in winter you need to first warm your hands in your pockets and gloves by placing them on the heating radiator. Don't rub your hands together.
- Upon entering the laboratory, the patient sits at the table opposite the laboratory assistant, after which he places his hand on a special pillow for drawing blood.
- To carry out the analysis, a small amount of capillary blood is required, which is usually obtained from the ring finger. This is due to the fact that he practically does not participate in various physical activities, so the risk of injuring the wound in this case is minimal. In addition, the hand and ring finger are separated from each other by an anatomical partition. Therefore, if bacteria gets into the puncture site, the infection will not be able to spread throughout the hand.
- The intended site for taking the test (finger pad) is treated with an antiseptic wipe, after which a small puncture is made on the side with a disposable scarifier to collect blood.
- The first drop of blood released is removed with a sterile napkin or cotton wool. The next portion of the biofluid is carefully collected into a glass adapter using a special tube, and then distributed into capillary blood tubes or placed on a glass slide.
- After completing the procedure, the wound is treated with an antiseptic to speed up the blood clotting process and a sterile cotton swab is pressed onto it.
- With low blood clotting and high blood pressure, bleeding may not stop for about 1-2 minutes. The cotton wool should be pressed as tightly as possible, and the hand should be raised with a finger up.
In young children (newborns) and some patients suffering from various pathologies, it can be very difficult to take blood for analysis from a finger prick. In this case, the puncture can be made on the earlobe or heel. Disposable sterile lancets are used as an applicator to puncture the skin of babies. The uniformity of the applied pressure minimizes pain and does not cause a negative psychological reaction in children.
Features of recycling
All consumables for injection procedures and sampling of biomaterials, including capillary blood, must be disposed of after use. In particular, the reuse of disposable lancets in most cases is impossible due to the design features: after performing a puncture and taking a sample, the needle is automatically hidden inside the body and blocked there. This is done in order to prevent the spread of infection. At home, when using universal lancets together with a glucometer, usually only the needles are changed, which are also a source of danger. They should not be thrown into the bin with normal household waste.
In medical institutions, all consumables that were used for collecting and conducting blood tests, syringes and other accessories after use are placed in special tanks for class B medical waste. Before disposal, they are disinfected under high temperature, chemicals or other means. Only after they become safe for people and the environment are they destroyed.
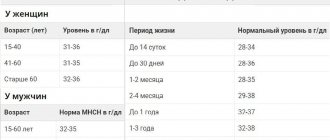
Decoding UAC indicators
Carrying out a clinical blood test allows us to identify deviations of the main indicators from the norm, which differ in men, women and children. Moreover, they also differ for children of different ages. Therefore, when interpreting the results, it is necessary to take into account the gender and age of the patient. The main parameter values are presented in the following table.
| No. | Parameter name | Normal value of the parameter depending on the gender of the patient | Purpose | Possible pathologies in case of deviations from the norm to the side | |
| wives | husband. | decrease | increase | ||
| Hemoglobin (Hb) | 120-140 g/l | 130-160 g/l | Transports oxygen from the lungs to tissues, internal organs and carbon dioxide in the opposite direction. | Anemia. | Dehydration, intestinal obstruction, congenital heart disease. |
| Red blood cells (RBC) | 3.7-4.7 g/l | 4.0-5.0 g/l | Red blood cells, in addition to transporting oxygen, help maintain the biological oxidation reaction. | Blood loss, anemia, overhydration. | A slight increase may be a consequence of a burn, diarrhea, or a consequence of taking diuretics. A significant increase indicates the possibility of kidney pathology, various neoplasms, disease and Cushing's syndrome. |
| Color Index (CPU) | 0,85–1,15% | Shows the concentration of hemoglobin in red blood cells. | Anemia. | Stomach cancer, polyposis, lack of folic acid in the body. | |
| Reticulocytes | 0,2–1,2% | Immature forms of young red blood cells produced by the bone marrow. | Aplastic and folate-deficiency anemia, kidney disease. | Iron deficiency, hemolytic anemia, blood loss. | |
| Platelets (PLT) | 180–320×109/l | Plates formed by bone marrow cells that are responsible for blood clotting. | Aplastic, hemolytic anemia, thrombocytopenic purpura, hemolytic disease, lupus erythematosus. | Inflammatory processes, polycythemia, tuberculosis, myeloid leukemia, rheumatoid arthritis. | |
| ESR (erythrocyte sedimentation rate) | no more than 20 mm/h | no more than 15 mm/h | Characterizes the protein content in blood plasma. | Chronic circulatory failure, hyperbilirubinemia, erythremia, high levels of bile acids. | Infectious and inflammatory processes, cancer, pathologies of internal organs (kidneys, liver), endocrine system, autoimmune disorders, intoxication. |
| White blood cells (WBC) | 4.0–9.0×109/l | White blood cells protect the body from various types of infectious diseases (viral, bacterial, parasitic) and help eliminate dying cells. | A decrease in the level of white blood cells is called leukopenia. Indicates the presence in the body of viral diseases, bone marrow hypoplasia, cancer with the spread of metastases in the bone marrow, collagenosis, typhoid fever, rubella, systemic lupus erythematosus, viral hepatitis. | Exceeding the norm is called leukocytosis and indicates the presence of diseases such as meningitis, pneumonia, otitis media, pancreatitis, erysipelas, bronchitis. May be a consequence of purulent processes (sepsis), acute inflammatory disease. | |
| Lymphocytes | 1.0–4.5×109/l | One of the types of leukocytes directly involved in the creation of the immune defense system. | Myocardial infarction, pneumonia, HIV, sepsis, lymphoma, autoimmune diseases. | Influenza, adenovirus, other viral infections, lymphocytic leukemia, tuberculosis, threotoxicosis. | |
| Granulocytes | 1.2–6.7×109/l | They are a type of granular leukocytes that are susceptible to allergic and infectious diseases. | Aplastic anemia, tuberculosis, sarcoidosis, systemic lupus erythematosus, acute rheumatism, pemphigus, scarlet fever. | Allergic and inflammatory processes, myxedema, ulcerative colitis, chickenpox, Khldzhkin's disease. | |
| Monocytes | 0.1–0.6×109/l | Cells that have not yet matured. Penetrating into tissues, they are transformed into macrophages, capable of cleansing the body of dead cells, foreign elements, and various pathogens. | Damage, bone marrow dysfunction, radiation sickness, hairy cell leukemia. | An increased number of monocytes is called monocytosis. Signals about the possible presence of subacute endocarditis, brucellosis, mononucleosis, tuberculosis, syphilis, leukemia, sepsis, malaria, lymphoma, toxoplasmosis. |
Analysis devices
Modern technologies are widely used not only in technology, but also in medicine. New laboratory medical equipment is being created to facilitate various analyzes and studies. In particular, automated analyzers have been developed for clinical (general) blood analysis. They allow you to obtain a more detailed analysis, which also records other parameters that are not included in the list of necessary ones for the KLA.
Using modern equipment, laboratory staff have the opportunity to process a larger amount of biomaterial in the same period of time, compared to a qualified laboratory technician. This is especially important, for example, when conducting examinations at enterprises, during medical examinations, and so on.
But even the most accurate equipment is not always able to work error-free, and given the fact that some indicators are calculated based on already obtained results, an error at the initial stage can lead to the receipt of erroneous data for other parameters. Therefore, many doctors, especially older ones, prefer to have the blood test done manually by a laboratory assistant.
In addition, an experienced laboratory technician, who during his work has processed not even hundreds, but thousands of blood tests, approaches the process creatively, taking into account all the features and nuances of the procedure, while the analyzer carries out calculations using average, standard parameters.
For example, during the processing of material, the analyzer can detect a low level of hemoglobin, which indicates possible anemia. But he will not be able to identify the cause of its occurrence. While the laboratory technician will not only calculate the parameter, but will also pay attention to the structure and size of red blood cells and will be able to determine the cause of the problem.
But in order for a person to quickly and efficiently process biomaterial, he must undergo preliminary training and gain significant experience. While it is possible to train an employee to use the analyzer in a significantly shorter time.
References
- Nazarenko G.I., Kishkun A.A. Clinical assessment of laboratory research results // M.: Medicine - 2006. - 544 p.
- Tatkov O.V., Stupin F.P. General blood test. Information collection // M.: Publishing solutions. — 2021. — 72 p.
- Fauci, Braunwald, Kasper, Hauser, Longo, Jameson, Loscalzo Harrison's principles of internal medicine, 17th edition, 2009
- Mosby's Diagnostic and Laboratory Test Reference 14th Edition, 3251 Riverport Lane
- St. Louis, Missouri 63043: Elsevier Publishing Hall 2019
Negative consequences
Despite the fact that this procedure is safe and has no contraindications, it is still an interference in the normal functioning of the body and, depending on the individual characteristics of the patient, can lead to some negative consequences, such as:
- severe pain, which can occur with high sensitivity, a low pain threshold of the patient, or as a result of inaccurate puncture of the skin;
- the occurrence of a hematoma at the puncture site, minor subcutaneous bleeding, which usually resolves on its own;
- body characteristics may include nausea, dizziness, weakness;
- If antiseptic rules are not followed, infection and infection may occur.
Drawing blood from young children can be associated with extreme distress, sometimes even shock.
Carrying out a capillary blood test is a simple, effective diagnostic method that allows you to identify the onset of the disease at its very beginning, therefore it is advisable to donate blood from a finger prick at least once a year for OAC. You should not attempt to decipher the analysis yourself. The attending physician will more accurately determine the existing problems and prescribe additional diagnostics.
Important Notes
Material for research
Children under 7 years of age: venous blood/capillary blood (for special indications).
Children over 7 years of age and adults: venous blood.
Capillary blood collection for research is carried out only for children under 7 years of age (for special indications).
According to GOST R 53079.4-2008, indications for taking capillary blood are possible in newborns, in patients with very small or hard-to-reach veins, with large-area burns, and in severely obese patients.