Why are they prescribed?
According to GMS Clinic therapist Natalya Polenova, throughout the previous year, doctors in most specialties were treating one “main” disease - a new respiratory viral infection, COVID-19. This disease is fundamentally different from its infectious predecessors in the risk of developing rapidly progressing complications, including life-threatening ones. And tests for inflammation, especially C-reactive protein (CRP), play a very important role in its diagnosis.
“One of the main dangers to life during Covid is the so-called cytokine storm,”
Natalya Polenova says.
— The harbingers of this storm can be considered a persistent (for 5 days) fever of more than 38°C, a decrease in the level of leukocytes less than 3 thousand/ml, an increase in the level of CRP more than 30 mg/dl, ferritin more than 500 ng/ml, interleukin-6 more than 40 pc /ml. The latter is a biologically active substance, a cytokine, directly responsible for the production of acute phase proteins: CRP, procalcitonin and ferritin.”
If a patient with coronavirus disease does not improve and the fever persists for several days, assessing the level of inflammatory markers in the blood may suggest a risk of severe disease. As a result, the doctor understands in time when it is necessary to hospitalize the patient, or decides to intensify therapy - for example, prescribe him glucocorticosteroids, antibacterial therapy and other therapeutic measures.
“Assessing the parameters of systemic inflammation allows us to determine treatment tactics, prevent the development of severe complications, and also evaluate the effectiveness of the therapy during repeated testing,” -
concludes Natalya Polenova.
Erythrocyte sedimentation rate (ESR)
What it is.
A blood test that shows how quickly blood cells settle to the bottom of a test tube over the course of an hour. Allows you to understand whether a person has hidden inflammation. ESR is often prescribed along with general blood tests - we wrote about it in a previous article.
How it works.
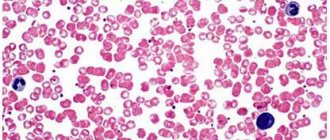
Blood consists of cells: red erythrocytes, white leukocytes and lymphocytes. They float in plasma, a salty liquid with proteins dissolved in it. As it moves through the vessels, all this is continuously mixed, so the blood resembles red paint. But if you leave it standing in a thin wedge capillary tube, the blood stratifies: red blood cells and white blood cells fall to the bottom under the influence of gravity.
Normally, cells descend to the bottom slowly. But if a person begins to experience inflammation, protective immunoglobulin proteins and fibrinogen appear in his blood - a protein that sews up wounds. These two proteins stick to the surface of red blood cells so that they sink faster. If a laboratory technician sees that a red precipitate has formed prematurely at the bottom of the capillary, he has the right to suspect that the person has hidden inflammation. But just to suspect: it happens that the ESR increases for other reasons not related to inflammation.
Why is it prescribed?
ESR is a nonspecific analysis. That is, it allows us to say that somewhere in the body there is inflammation, but it does not explain why it happened. Only a doctor can make a conclusion about this after examining the patient: in order to understand the cause of inflammation, additional information is most often needed.
As a rule, doctors prescribe ESR for a reason, but if they already suspect that there is an inflammatory process going on somewhere. Most often, such patients complain of headache, temperature above 37°C, pain in the neck, shoulders or joints, unexplained loss of weight or appetite.
“ESR is a very non-specific indicator, it can increase in many cases,”
says a therapist at one of the clinics in Moscow.
— As a rule, ESR is prescribed for rheumatic diseases - these are systemic diseases in which the immune system attacks the patient’s own tissues.
These are systemic lupus erythematosus, rheumatoid arthritis, vasculitis. The degree of severity of the process can be judged by the value of ESR. If the ESR norm is usually up to 25, then with these diseases the indicator can be 40 - this indicates the average severity of the process. If the ESR rises to 80, the process is even more difficult.” The doctor clarifies that ESR can be a valuable indicator if you compare its results with the data of a general blood test. If a patient suddenly, against the background of general well-being and a “calm” general blood test, reveals a huge ESR in the range of 80-100, this makes one think about a cancerous tumor. In some rather rare cases, with such an ESR, we can talk about inflammatory diseases, suppuration - but first of all, the doctor must think about cancer.
ESR also increases with pneumonia. If we are talking about coronavirus disease, then this analysis may partly indicate the severity of coronavirus pneumonia. Because if the ESR is elevated slightly above normal, to 27-30, the inflammatory process is moderate. If the ESR is 45-50, the inflammation is more pronounced. But ESR is an inaccurate analysis, because it can increase even with dental caries, pregnancy and many other conditions. So, in case of coronavirus disease, you should not rely on it.
What to look for when choosing a laboratory.
In our country and abroad, ESR analysis is done using different methods. The Westergren method is used all over the world, in which 2 ml of venous blood is taken from the patient. This method is considered the most reliable. In our country, ESR is often done using the Panchenkov method, when approximately 100 μl of capillary blood is taken from a patient’s finger. This is simpler and cheaper, but microclots may form in capillary blood during collection, so the method is considered less reliable.
When choosing a laboratory, you need to pay attention that the blood test for ESR is done from venous blood using the Westergren method. Some laboratories write that they do analysis using it, but from capillary blood - most likely, this is a modification of the Panchenkov method, and no one has checked its reliability.
As a rule, patients who donate blood under compulsory medical insurance, that is, free of charge, are tested using the Panchenkov method. Therefore, it makes sense to check in advance with the doctor who sent you for analysis whether he is satisfied with this result.
How to prepare.
Abroad, it is believed that there is no need to specially prepare for the analysis. But in our country it is customary to take the test in the first half of the day and on an empty stomach, in extreme cases - at least three hours after the last meal - it is believed that this way the analysis will be more accurate, because there will be nothing “extra” in the blood.
How to understand the result.
Normally, ESR differs in people of different sexes and ages, and also depends on the method by which the analysis was performed. In general, the indicators are similar, but the range of “norms” that the Westergren method covers is wider than with the Panchenkov method - mainly because the capillary tube used in the first method is longer than the one used in the second.
In healthy adult men under 60 years of age, Westergren's ESR should be between 2-15 mm/hour, and in healthy non-pregnant adult women - within 2-20 mm/hour. ESR increases by 0.8 mm/h every five years: in men up to 20, in women - up to 30 mm/h. In pregnant women, ESR increases from the 4th month of pregnancy, and by the time of birth it can reach 40-50 mm/hour - and this is completely normal.
ESR can be either increased or decreased. A high ESR, that is, 60-100 mm/h or more, is a sign of serious problems: it can be anything from severe bacterial infection and rheumatism to tumors and temporal arteritis. A moderate increase in ESR, that is, 20-60 mm/h, can also indicate an infection, and also anemia, pregnancy or aging. The exact cause can only be identified together with a doctor.
During coronavirus disease, measuring ESR is also very important. An increase in this indicator may indicate that a bacterial infection has joined the virus. A sharp drop in ESR with COVID-19 can also be a sign of a serious complication. For example, macrophage activation syndrome, an immunological disorder that can occur in children with coronavirus disease.
A low ESR may indicate increased blood viscosity. This happens, for example, with polycythemia, when there are too many red blood cells in the blood, in people who take non-steroidal inflammatory drugs, and in athletes with high physical activity. You also need to deal with low ESR together with your doctor.
Increasing ESR
A similar result may be caused by the following pathologies:
- Infection or inflammation.
- Connective tissue diseases (RA, SLE, vasculitis, etc.).
- Burn disease.
- Neoplasms of different etiology and localization.
- Myocardial infarction. In the post-infarction period, the maximum occurs after about 7 days (in this case, you need to contact a vascular surgeon).
- Anemia. These diseases are characterized by a decrease in red blood cells and an increase in their sedimentation rate.
- Injury.
- Amyloidosis (a pathology characterized by the formation of a pathological protein - amyloid).
Despite the discrepancy between normal limits, if a complete blood count of ESR showed an increase in this indicator, this does not necessarily indicate the presence of a problem. This result also occurs in healthy individuals: in women during the menstrual cycle, during pregnancy, or in overweight individuals. This also occurs when taking a number of medications, so you should consult your doctor in advance.
C-reactive protein (CRP) test
What it is.
A venous blood test in which the concentration of C-reactive protein in a sample is determined. This test is a more accurate indicator of inflammation than ESR because C-reactive protein appears in the blood only during inflammation.
How it works.
The liver produces C-reactive protein in response to the call of immune cells that have encountered a problem, from a bacterial or viral infection to cancer cells. When it encounters dead or dying cells, the protein binds to them and triggers another defense mechanism - it activates the complement system. This means that normally there is either no CRP in the blood, or very little. And if it appears, it means there is definitely inflammation going on somewhere.
Why is it prescribed?
Although CRP is a more reliable marker of inflammation than ESR, the mere fact of its presence in the blood does not indicate anything about the causes of inflammation, so it is not suitable for diagnosis. As a rule, the analysis is prescribed to clarify the diagnosis or to monitor treatment: for example, if a patient with COVID-19 has a CRP level of more than 10 mg/l, then this, along with other signs, may indicate a moderate course of the disease.
“CRP is a more accurate indicator than ESR,”
says another specialist at a Moscow clinic
- it reflects the severity of bacterial inflammation.
If a patient has high white blood cells and high CRP, this strongly suggests that they have a bacterial infection that needs to be treated with antibiotics.” In pneumonia, CRP will reflect the extent of lung damage. The norm is from 0 to 6. If a person has a common cold, it will be in the range of 10-12. But if CRP, for example, is in the range of 100-300, we are most likely talking about serious pneumonia.
“If a person has pneumonia confirmed on an X-ray or CT scan, CRP will fall as they recover,”
explains another doctor.
“At the same time, there are clinical conditions when a person who has recently suffered coronavirus disease maintains a residual temperature within the range of 37.1-37.2°C. If the CRP is normal, this indicates that the patient has actually recovered. And if CRP is high, the person needs further treatment.”
How to prepare. How to ESR
What to look for when choosing a laboratory.
The normal level of CRP depends on the method used to determine the protein. If the method is standard, then all people should have CRP in the range of 0-10 mg/l. And if the method is highly sensitive (hs-CRP), then the protein level should be less than 3 mg/l. Highly sensitive analysis is more expensive, but is not always needed. Therefore, if a doctor has prescribed this test, it makes sense to clarify what kind of analysis is needed.
How to understand the result of the analysis.
Normally, CRP should not be high. However, you can only understand why it has increased with your doctor. For example, CRP can remain at levels from 3 to 10 mg/l during pregnancy, a sedentary lifestyle and smoking - or perhaps due to diabetes, periodontitis or hereditary diseases.
A level from 10 to 100 can indicate both myocardial infarction and bronchitis. And if the level is more than 100, it can be extensive injuries, bacterial and viral infections.
Only a very strong increase in the level of CRP - more than 500 mg/l - clearly indicates acute bacterial infections. But this does not mean that if the level of CRP is lower, then there is no bacterial infection. Additional examinations can help to understand whether this is true or not: for example, bacterial culture. Without additional information and consultation with a doctor, it is very difficult to say anything definite about the reason for the increase in CRP.
In what cases does ESR not need to be treated?
Elevated ESR can also occur due to poor nutrition, if the diet is dominated by unhealthy foods high in fat, as well as an excess of spicy foods.
The level of ESR is also affected by a lack of vitamins in the body. In this case, the doctor may even prescribe a special therapeutic diet.
If you have recently had surgery, increased subsidence will be normal.
Therefore, if you notice a deviation from the norm in your blood test, do not rush to sound the alarm, and treatment without knowing the cause will not be beneficial.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
If you find an error, please select a piece of text and press Ctrl+Enter
Procalcitonin test
What it is.
A blood test in which the concentration of the protein procalcitonin is determined in a sample. This study is more accurate than ESR and CRP, because it confirms with a high degree of probability that it was pathogenic bacteria that caused the inflammation, and not other causes. However, the procalcitonin test is more expensive than other tests, so doctors usually start with simpler and more affordable tests. However, the test does not allow us to understand which bacteria cause the inflammatory reaction.
How it works.
Normally, there is practically no procalcitonin in the blood. However, in response to the bacterial invasion, almost all cells in the body begin to intensively create this white, so that its level in the blood rises sharply. Most likely, the level of procalcitonin in the blood increases in response to bacterial poisons that they secrete during their life processes - so that during a viral infection, injury and attack by parasitic fungi, the level of procalcitonin increases quite a bit.
So far, researchers do not fully understand what role procalcitonin plays in antibacterial defense. But the very fact of increase allows the level of procalcitonin in the blood to be used as a fairly reliable marker of bacterial infection.
Why is it prescribed?
To reliably distinguish a bacterial infection from a viral one. For example. with ordinary, uncomplicated coronavirus disease, the level of procalcitonin in the blood is within normal limits.
If the concentration of procalcitonin increases, it means that a bacterial infection has joined the viral infection, and it is time to prescribe antibiotics. The procalcitonin test is used to monitor the condition of patients being treated in hospital, for example, with severe COVID-19.
“Procalcitonin is rarely used in outpatient practice,”
says another specialist.
— It came into fashion recently, with the beginning of the coronavirus disease epidemic.
It is believed that he predicts its severe course. But in fact, this test came from intensive care - it indicates sepsis, that is, blood poisoning. There is no need to do this test yourself.” How to prepare. For people who are being treated at home, a procalcitonin test is practically not prescribed. But in general, the preparation rules are the same as for ESR and SRB.
How to understand the result of the analysis. The appearance of procalcitonin in the blood is always a bad sign, even if the protein level has increased slightly. Moderately elevated levels of procalcitonin - from 0.15 to 2 ng / ml - in adults may indicate a local mild or moderate bacterial infection, an autoimmune reaction, or severe renal failure. If the level of procalcitonin rises above 2 ng/ml, we are talking about bacterial infection of the blood, that is, sepsis, a severe bacterial infection like meningitis, or a cancer of the thyroid gland.
How is diagnosis carried out?
The erythrocyte sedimentation rate is currently determined during a general blood test. It is very comfortable. The expectant mother does not need to prick her finger repeatedly or take venous blood.
Doctors recommend determining this indicator at least three times during the entire period of gestation. These tests are usually prescribed at 12, 21 and 30 weeks of pregnancy.
You can take this laboratory test either in a regular clinic or in a private medical laboratory. You must come for the study on an empty stomach. Before taking the test, you can drink some water if you are thirsty. No special preparation is required.
The technique involves collecting blood in several ways. For quite a long time, this analysis was carried out only by the capillary method. To do this, the finger is pierced using a special medical instrument. It should be noted that, according to statistics, this method is less well tolerated, as it is more painful and traumatic.
Currently, in almost any medical institution, blood sampling is carried out via venous access. For this purpose, as a rule, special vacuum tubes are used. Through their use, the method has become very widespread. It is easier to tolerate and causes much less discomfort.
After blood is collected, it is placed in a special tube. In order for the process of sedimentation of red blood cells to begin, a special chemical substance is added to it - an anticoagulant. It is with its help that red blood cells do not stick together, but begin to settle.
The study is carried out within an hour. During this time, the blood is stratified into two fractions of different densities - plasma and formed elements. After the allotted time for research has expired, the laboratory assistant measures the thickness of each layer. It also records the resulting erythrocyte sedimentation rate result. This indicator is measured in special units of measurement - mm/hour.
Important to remember
- Inflammation tests—ESR, CRP, and procalcitonin test—help determine whether there is underlying inflammation in the body
- The most sensitive test of this trio, the procalcitonin test, allows you to distinguish a viral infection from a bacterial one, but does not allow you to find out which bacteria caused the infection. Typically, it is used in a hospital to monitor the condition of critically ill patients.
- Less sensitive tests - ESR and CRP - allow you to understand whether there is inflammation or not. CRP does this more accurately than ESR, but is more expensive, so it is rarely prescribed “just in case.” However, both CRP and ESR are often prescribed to patients who are recovering at home
- There is no point in doing inflammation tests as part of a check-up: in healthy people they will not provide any interesting information. And even if they do, it will be very difficult to figure out the results on your own. It is better to leave the appointment of tests for inflammation to the doctor - he will determine which test is needed, help you understand the results and prescribe competent treatment.