Classification
There are no clear digital gradations for dividing the increase in ESR by degree. Conventionally, moderate and high degrees are distinguished. According to the mechanism of occurrence they distinguish:
- True increase in ESR
. The cause is various inflammations, infectious, and oncological pathologies. Develops as a result of dysproteinemia, which increases erythrocyte aggregation. - False increase in ESR
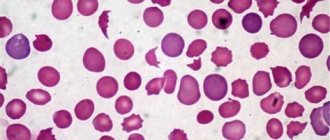
. False acceleration of ESR is observed in anemia, azotemia, alkalosis, and high blood cholesterol levels. The cause of this phenomenon is various pathological processes in which the ESR increases due to changes in the number or shape of red blood cells, the protein-lipid composition of plasma, a shift in blood pH, and the presence of other chemical compounds.
Why do you need to monitor your blood counts?
ESR is a marker that can indicate that something is wrong with the body. If the red blood cells become heavier and sink faster to the bottom of the test tube that is used for testing, you need to undergo an examination to determine what exactly caused the change in the indicator. It is necessary to fight not with the increase in erythrocyte sedimentation rate itself, but with the reasons that caused it. If you ignore changes in your body, you may miss the time needed to prevent severe complications from COVID-19.
You can undergo a complete diagnosis at La Salute. The clinic is equipped with equipment that provides accurate results. If complications are identified, you will also be able to undergo a rehabilitation course with us. La Salute specialists have developed techniques that help restore the body after coronavirus and prevent the development of complications that can worsen the patient’s quality of life.
Sign up for COVID-19 testing at La Salute clinic
Reasons for increasing ESR
Physiological conditions
An increase in ESR does not always indicate a pathological process. Some physiological conditions also cause an increase in ESR. For example, the cause of such an increase in ESR may be food intake, insufficient fluid intake, or intense physical activity. An increase in ESR also occurs during pregnancy. The indicator increases with each trimester, reaching a maximum at childbirth. Numerous studies have noted that ESR gradually increases with age (every 5 years by 0.8 mm/hour). Therefore, in almost all elderly people, an ESR of up to 40-50 mm/hour is observed in the blood. Approximately 10-15% of absolutely healthy people experience an increase in ESR.
Infections
Infectious diseases are recognized as the most common cause of increased ESR in the blood. The pathogenetic mechanism is that the resulting inflammatory proteins (fibrinogen, C-reactive protein) and immunoglobulins (antibodies) to foreign microorganisms, which have a positive charge, are adsorbed on the surface of red blood cells, reducing their negative charge. This weakens the force of mutual repulsion of red blood cells, which leads to their agglutination, aggregation ("sticking together"), the formation of "coin columns", which is why they settle faster than normal.
- Acute infections
. An increase in ESR occurs somewhat later than the onset of clinical symptoms of the pathology, the appearance of leukocytosis in the blood and fever, and correlates with the severity of the infection. With bacterial and fungal infections (tonsillitis, salmonellosis, candidiasis), the ESR is much higher than with viral infections (influenza, measles, rubella). It reaches a maximum after the reverse development of pathological processes, persists for some time after recovery, then gradually decreases. - Chronic infections
. Chronic infections of the urinary system and oral cavity are recognized as a common cause of persistently increased ESR. Quite often, an increase in ESR may be the only manifestation of such sluggish infectious inflammatory processes as tuberculosis, helminthic infestations, and chronic viral hepatitis C.
Aseptic inflammation
The cause of high ESR is also pathological conditions accompanied by tissue damage and decay. These are infarctions of various organs (myocardium, lung, kidneys), surgical interventions, non-infectious inflammation of the gastrointestinal tract (pancreatitis, cholecystitis). Under the influence of tissue breakdown products, proteins of the acute phase of inflammation are produced, mainly fibrinogen, which binds to the membrane of erythrocytes, which causes their aggregation. An increase in ESR does not occur immediately, but approximately on the 2-3rd day; it increases rapidly at the end of the 1st week, when the level of leukocytes in the blood begins to decrease. This phenomenon is especially typical of myocardial infarction and is called the “crossover sign.”
Immune inflammation
The change in the negative charge of erythrocytes in nosologies characterized by immunopathological reactions is caused by the deposition of immune complexes and gamma globulins on the membrane of red blood cells. An increase in ESR develops gradually, reflects the activity of the inflammatory process, and normalizes during remission. ESR serves as an indicator of the effectiveness of pathogenetic treatment. It is noteworthy that its increase occurs much earlier than the onset of symptoms of these diseases (joint pain, skin rashes, etc.).
Of this group of diseases, the most common causes of increased ESR in children are considered to be acute rheumatic fever, in adults - rheumatoid arthritis, in the elderly - polymyalgia rheumatica.
- Joint diseases
: ankylosing spondylitis (ankylosing spondylitis), reactive arthritis. - Diffuse connective tissue diseases (collagenoses)
: systemic lupus erythematosus, Sjogren's syndrome, systemic scleroderma, dermatomyositis. - Systemic vasculitis:
giant cell arteritis, granulomatosis with polyangiitis, polyarteritis nodosa. - Inflammatory bowel diseases
: Crohn's disease, ulcerative colitis. - Other autoimmune pathologies
: glomerulonephritis, autoimmune hepatitis, thyroiditis.
Hemoblastoses
The cause of a pronounced increase in ESR (up to 100 mm/hour and above) is tumors of the B-lymphocyte system (paraproteinemic hemoblastosis). These include multiple myeloma, Waldenström's macroglobulinemia, and heavy chain disease. These pathologies are characterized by the secretion of a large number of paraproteins (abnormal proteins), causing hyperviscosity of the blood and changing the membrane potential of red blood cells. Moreover, an increase in ESR often develops several years before the onset of the first symptoms (itching, sore throat, bleeding). An increase in ESR, although less sharp, occurs in patients with other oncohematological pathologies (leukemia, lymphoma).
Oncological diseases
Sometimes the cause of an increase in ESR in the blood is solid (non-hematopoietic) tumors. The increase in ESR is explained by two mechanisms: an increase in the level of fibrinogen, tumor markers and the breakdown of malignant formation. The degree of increase in ESR is determined not by the histological structure of the tumor, but by its size and damage to surrounding tissues. Often the appearance of elevated ESR in the blood precedes clinical symptoms.
Rare causes
- Metabolic disorders
: amyloidosis, familial hypercholesterolemia, generalized xanthomatosis. - Endocrine pathologies
: thyrotoxicosis, hypothyroidism. - Heavy metal poisoning
: intoxication with arsenic, lead. - Use of medications
: dextrans, estrogen-containing drugs (oral contraceptives).
General information
New methods for diagnosing and determining the causes of diseases appear in modern medicine regularly. However, determining ESR in human blood is still an effective diagnostic method.
It is used for diagnostic purposes in both children and adults. Such a study is prescribed both when a patient who is concerned about a certain disease contacts a doctor, and during preventive examinations. Any doctor can interpret this test. ESR is included in the group of general blood tests (CBC). If this indicator is elevated, you need to determine the cause of this phenomenon.
Diagnostics
Any, even asymptomatic, increase in ESR requires contacting a doctor to find out the cause. The doctor asks the patient in detail whether there was an increase in body temperature, whether the patient experienced pain in the joints, muscles, fatigue, etc. This can help in the diagnostic search. An additional examination is prescribed, depending on what nosology is suspected:
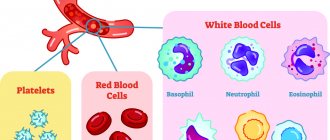
- Blood tests
. The concentration of hemoglobin and blood cells (erythrocytes, platelets, leukocytes) is measured. Very often an increase in the level of fibrinogen and C-reactive protein is detected. The blood is checked for the presence of autoaggressive antibodies (aCCP, antineutrophil cytoplasmic antibodies, antibodies to double-stranded DNA). In severe bacterial infections, high levels of presepsin and procalcitonin are observed in the blood. - Identification of the infectious agent
. Antibodies to antigens of viruses, bacteria, parasites are determined using ELISA methods and serological tests. PCR detects DNA and RNA of microorganisms. Microscopy, bacteriological culture of urine, sputum, and blood are performed. A stool test is performed for worm eggs. - Radiography
. With tuberculosis, an X-ray of the lungs shows an increase in mediastinal lymph nodes and infiltration in the upper lobes of the lungs. In paraproteinemic hemoblastoses, x-rays of the bones reveal numerous foci of bone tissue destruction. Multiple myeloma is characterized by a “puncture sign” on a skull x-ray. - Ultrasound
. An ultrasound scan of the abdominal cavity reveals thickening of the walls of the gallbladder in cholecystitis, enlargement and diffuse changes in the pancreatic parenchyma in pancreatitis, and enlargement of the liver and spleen in hemoblastosis. - Angiography.
In case of infarctions of various organs caused by thrombosis, radiography or computed tomography with contrast reveals a filling defect at the site of vessel occlusion. With systemic vasculitis (Horton's, Takayasu's arteritis), areas of vascular stenosis are visible. - Histological studies
. If the cause of increased ESR is oncological pathology, a biopsy is necessarily performed. A common symptom is the detection of a large number of atypical cells. In patients with malignant blood diseases, a predominance of blast cells is noted in the bone marrow aspirate, and atypical lymphoid proliferation is noted in the lymph node biopsy.
How to get tested
You need to take the test calmly, it’s too late to get nervous - everything has already happened in the body and all that’s left is to get the information. It would be more correct to pose the question differently: where to take it. It is advisable for an oncology patient to undergo tests in a specialized institution, where not only analysis on the machine is available, but also monitoring of the results obtained “in manual mode”. With specific treatment, especially after the use of medications, the conventional boundary of normality of indicators may temporarily shift. Often, haste in interpreting the result results in excessive examination and unnecessary treatment.
If you want an optimal and unconditionally professional approach, accuracy and objectivity, come for a consultation at our clinic.
Book a consultation 24 hours a day
+7+7+78
Bibliography
- Lugovskaya S.A., Morozova V.T., Pochtar M.E., Dolgov V.V. /Laboratory hematology// M.: Publishing house. Unimed-press; 2002.
- Pervushin Yu.V., Lugovskaya S.A., Marchenko L.A., Kovalevich N.I. / Hematological studies in clinical laboratory diagnostics//Stavropol; 2006
- Nazarenko G.I., Kishkun A.A. / Clinical assessment of laboratory research results // M., 2000.
- Oganesyan A.A., Garbatsevich M.S., Kostyukovich D.I. and others /ESR: old test, new opportunities // Lab. diagnostics. Eastern Europe; 2012; No. 4.
- Chizhevsky A. L. /Biophysical mechanisms of erythrocyte sedimentation reaction// Novosibirsk: Science, 1986.
Correction
Conservative therapy
A transient increase in ESR after exercise, food intake or medications does not require correction. Elderly people with high ESR without other clinical and laboratory signs of any pathology also do not need any intervention. To normalize the pathological increase in ESR, it is necessary to treat the nosology that caused its development.
- Fighting infection
. For bacterial infections, antibiotics are prescribed according to sensitivity. If the patient's condition is serious and requires immediate treatment, broad-spectrum antibiotics (penicillins, cephalosporins, fluoroquinolones) are used. For influenza, oseltamivir is used; for other acute viral infections, symptomatic therapy is used. For the treatment of chronic viral hepatitis, combinations of peligated interferon with ribavirin and entecavir are effective. - Anti-inflammatory therapy
. For diseases accompanied by immune inflammation, anti-inflammatory drugs are needed - glucocorticoids (prednisolone), cytostatics (azathioprine, methotrexate), 5-aminosalicylic acid derivatives (sulfasalazine). If they are ineffective, tumor necrosis factor inhibitors - monoclonal antibodies (infliximab) are used. - Blood thinning
. If the cause of the heart attack is thrombosis or embolism, antiplatelet agents (clopidogrel, acetylsalicylic acid) and anticoagulants (heparin, warfarin, dabigatran) are prescribed. Thrombolytics (streptokinase) are used to dissolve a blood clot. - Chemotherapy.
Antitumor drugs (alkylating agents, antimetabolites) are used to treat cancer. Malignant blood diseases require a combination of several chemotherapy drugs.
Surgery
In case of acute abdominal pathology (cholecystitis, pancreatitis), it is necessary to perform a surgical (sometimes emergency) operation - pancreatic resection, laparoscopic cholecystectomy. Endovascular thrombectomy is performed to remove the thrombus. In case of myocardial infarction, percutaneous coronary intervention (stent placement) is performed. Unsuccessful conservative therapy for oncohematological diseases is considered an indication for bone marrow transplantation.
Important to remember
- Inflammation tests—ESR, CRP, and procalcitonin test—help determine whether there is underlying inflammation in the body
- The most sensitive test of this trio, the procalcitonin test, allows you to distinguish a viral infection from a bacterial one, but does not allow you to find out which bacteria caused the infection. Typically, it is used in a hospital to monitor the condition of critically ill patients.
- Less sensitive tests - ESR and CRP - allow you to understand whether there is inflammation or not. CRP does this more accurately than ESR, but is more expensive, so it is rarely prescribed “just in case.” However, both CRP and ESR are often prescribed to patients who are recovering at home
- There is no point in doing inflammation tests as part of a check-up: in healthy people they will not provide any interesting information. And even if they do, it will be very difficult to figure out the results on your own. It is better to leave the appointment of tests for inflammation to the doctor - he will determine which test is needed, help you understand the results and prescribe competent treatment.