Indications for testing
Blood is one of the most informative resources of the human body. By sending it for laboratory testing, the vast majority of diseases can be diagnosed with high accuracy. Clinical analysis contains many indicators, each of which reflects a specific process and function and serves as an important diagnostic criterion. However, despite the abundance of examinations, the most common and in demand at the MedArt clinic is a general blood test (ESR).
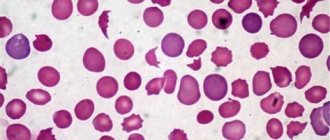
Erythrocyte sedimentation rate is the most important indicator, often confirming the presence of inflammation or other pathology (in the acute and latent stages). The mechanism of this analysis is quite simple, so you don’t need to spend several days to get the result. Red blood cells are much heavier than plasma and other cellular elements, and therefore, by placing blood in a vertically placed test tube, after a certain period of time a specific sediment will form at the bottom of the container, and a translucent liquid will appear at the top.
This is a completely natural phenomenon that occurs as a result of gravity. Red blood cells can stick together, forming entire colonies that settle to the bottom much faster than individual elements. This is due to the larger mass, which may indicate a problem.
ESR and oncology
In the absence of an inflammatory and infectious disease, a significant increase in ESR should raise suspicion regarding the presence of a malignant tumor. At the first suspicion of its presence, a consultation with an oncologist and a thorough additional examination using high-tech equipment and competent specialists are necessary.
Oncology is a multifactorial disease, accompanied by both inflammatory processes and anemia, metabolic disorders, and therefore causing the body to release a large amount of active substances and proteins. Therefore, most patients with various forms of malignant tumors have an elevated ESR.
For example, ESR in lung cancer may increase in the presence of pneumonia near the tumor. With colon or stomach cancer, severe anemia occurs, which leads to an increase in ESR.
There is no specific level for each tumor; most often, the increase is due to a combination of many factors.
The highest level of ESR (80-90 mm/h or more) associated with oncology is usually determined in diseases grouped as “paraproteinemias” (myeloma, Waldenström's macroglobulinemia). With these diseases, structurally abnormal and functionally defective proteins appear in the blood, which leads to changes in the blood.
How to prepare for the test
ESR is included in the list of standard indicators that are displayed in all blood tests (general and clinical). However, special attention is paid to it in the following situations:
- Diagnosis confirmation
- Preventive examination
- Evaluation of the effectiveness of prescribed treatment
- Infectious and inflammatory pathologies
- Autoimmune disorders
- Tumors (malignant and benign) of any location
Many pathologies of internal organs are asymptomatic, and often identifying an ESR deviation from the norm becomes a reason to begin a more detailed diagnosis, thanks to which it is possible to identify the problem in the early stages and begin effective treatment. Most often, after any abnormalities are found, an additional biochemical analysis is prescribed, which allows a more detailed study of the bloodstream.
What to do if ESR is elevated
If a person took a blood test during a routine medical examination and found an elevated ESR, but there were no other deviations from the norm, most likely this is not a big deal. To get rid of doubts, the doctor should prescribe The erythrocyte sedimentation rate. Still a helpful test when used judiciously retest after a few months.
But those who have other changes in their blood may need further testing. Which one will be decided by the specialist who noticed the increased ESR.
How the research is carried out
The accuracy of this diagnostic method depends on many nuances: proper preparation for the test, the professionalism of the laboratory worker and the quality of the reagents. Subject to these conditions, you can guarantee the most reliable result. And if the person donating blood cannot influence the last 2 points, then the preparatory stage completely depends on him. Despite the fact that in this case no special and complex preparation is required, there are a number of mandatory general rules that are strongly recommended to be followed.
First of all, 1 day before the test, you must stop drinking alcoholic beverages, and also refrain from eating for 4-5 hours. Only drinking plain water is allowed. It is also recommended to quit smoking an hour before the test. Secondly, if the patient takes (on an ongoing basis or only at the moment) any medications, then the doctor must be informed about this in advance. Some medications can distort the results, which is why their use may be stopped and reinstated after donating blood. Thirdly, on the eve of the procedure you should not visit sports or gyms. You should also refrain from intense physical activity and avoid emotional stress.
If you doubt anything, just call us at this number +375(29) 666-30-96 or make an appointment with a doctor using our online form.
How to prepare
The duration of the analysis does not exceed 5-10 minutes. As a rule, the procedure is accompanied by slight pain and discomfort in the puncture area, but the discomfort passes very quickly. If capillary blood is needed, then before piercing the third or fourth finger of the left hand, the skin in this place is treated with an alcohol cotton ball. After this, using a special medical blade, a small incision is made on the fingertip (its depth does not exceed 3 millimeters). The resulting drop of blood is disposed of with a sterile napkin, after which the laboratory assistant proceeds to collect the biomaterial. Having collected the required amount, the wound surface is lubricated with an antiseptic, and a cotton swab with alcohol is applied to the puncture site.
If the analysis involves taking biomaterial from a vein, then the patient’s forearm is tightened with a medical tourniquet or strap, after which he must work a little with his fist (clench and unclench) for better vascular filling. The site of the intended puncture is treated with an alcohol wipe, after which a needle is inserted into the selected vessel, to which a test tube is connected to collect the released blood. Having collected a sufficient amount of biomaterial, the needle is removed, and a cotton swab with alcohol is applied to the wound.
To calculate ESR, an anticoagulant is placed in the biological material to prevent clotting. Then it is sent to a vertical container for 60 minutes. Since the specific gravity of red blood cells exceeds the weight of plasma, gravity forces them down to the bottom of the container. Because of this, 2 visible layers are formed in the test tube: the upper (colorless plasma) and the lower (erythrocyte accumulations). Then the laboratory assistant takes measurements of the top layer. The indicator corresponding to the mark between the red blood cells and the plasma zone on the test tube scale is ESR (indicated in mm/h).
Today there are 2 main ways to detect ESR:
- Panchenkov's method. The capillary is divided into exactly one hundred compartments, and later 5% sodium citrate is added to it to the “P” level. Then the capillary is filled with biomaterial up to the letter “K”. The resulting mixture is mixed and installed vertically. The assessment takes place after 60 minutes.
- Westergren method. Here, venous blood is used, mixed with sodium citrate 3.8% in a ratio of 4:1. It can be mixed with Trilot B followed by the addition of sodium citrate or saline solution in an amount of 4:1. The study is carried out in test tubes equipped with a 200 mm scale. The result is assessed after 60 minutes. This technique is used everywhere, and its main distinguishing feature is the type of test tubes and measuring scale used.
Despite the coincidence of the results of these methods, the Westergren method is famous for its greater sensitivity to exceeding the ESR indicator, and therefore it is considered highly accurate and informative.
MCH norm indicators
The figure varies depending on gender and age. For newborns (up to 1 month), ESR ranges from 1 to 2 mm/h. These limits are explained by reduced protein concentration. From 1 month to six months it ranges from 12 to 17 mm/h. This sharp increase in the norm is explained by age-related processes that occur in the growing body. Then the data is stabilized - for a child under 10 years of age, normal limits are considered to be numbers from 1 to 10 mm/h.
Since blood viscosity has several gender differences, the ESR rate will be different for men and women. For representatives of the fair sex from 10 to 50 years old, the acceptable limits are 0-20 mm/h, and from 50 years old - from 0 to 30 mm/h. The number may change during pregnancy, which is normal, but requires monitoring by your attending physician. In men from 10 to 50 years old, this figure should be from 0 to 15 mm/h, and over 50 years old - from 0 to 20 mm/h.
| Age, years | ESR norm |
| Baby up to 1 month | 1-2 mm/h |
| Child 1 month – 6 months | 12-17 mm/h |
| Child under 10 years old | 1-10 mm/h |
| Woman 10-50 | 0-20 mm/h |
| Woman over 50 | 0-30 mm/h |
| Male 10-50 | 0-15 mm/h |
| Man over 50 | 0-20 mm/h |
The final result is influenced by many factors: improper preparation, anxiety, taking medications and much more. In addition, the value may even depend on the time of day. As a rule, the maximum is determined around noon.
What is ESR
Erythrocyte sedimentation rate (ESR) is an indicator whose determination is included in a general blood test. This is a nonspecific laboratory screening test, changes in which can serve as an indirect sign of ongoing inflammatory or other pathological processes, such as malignant tumors and diffuse connective tissue diseases
FACTORS AFFECTING ESR INDICATOR
The ESR indicator varies depending on many physiological and pathological factors.
ESR values in women are slightly higher than in men .
Changes in the protein composition of the blood during pregnancy lead to an increase in ESR during this period.
A decrease in the content of erythrocytes (anemia) in the blood leads to an acceleration of ESR and, on the contrary , an increase in the content of erythrocytes in the blood slows down the sedimentation rate.
The values may fluctuate during the day ; the maximum level is observed during the daytime.
The main factor influencing the formation of “coin columns” during erythrocyte sedimentation is the protein composition of the blood plasma.
Acute-phase proteins, adsorbed on the surface of erythrocytes, reduce their charge and repulsion from each other, promote the formation of coin columns and accelerated sedimentation of erythrocytes.
An increase in acute phase proteins , for example, C-reactive protein, haptoglobin, alpha-1-antitrypsin, during acute inflammation leads to an increase in ESR.
In acute inflammatory and infectious processes, a change in the erythrocyte sedimentation rate is observed 24 hours after an increase in temperature and an increase in the number of leukocytes.
In chronic inflammation, an increase in ESR is caused by an increase in the concentration of fibrinogen and immunoglobulins.
Some morphological variants of red blood cells can also affect ESR. Anisocytosis and spherocytosis inhibit red blood cell aggregation. Macrocytes have a charge corresponding to their mass and settle faster.
In anemia, drepanocytes influence the ESR so that even with inflammation, the ESR does not increase.
REASONS FOR CHANGES IN ESR INDICATORS
Normal ESR value
Depends on gender and age:
- in newborns, the ESR is very slow - about 2 mm, which is associated with a high hematocrit and low globulin content
- by 4 weeks the ESR accelerates slightly
- by 2 years it reaches 4-17 mm
- in adults and children over 10 years of age, ESR ranges from 2 to 10 mm for men and from 2 to 15 mm for women, which can be explained by different levels of androgenic steroids
- in older people, normal ESR levels range from 2 to 38 in men and from 2 to 53 in women.
Increase in ESR value
The most common reason for an increase in ESR is an increase in the plasma content of coarse proteins (fibrinogen, a- and g-globulins, paraproteins), as well as a decrease in albumin content. Coarse proteins have less negative charge. By adsorbing on negatively charged erythrocytes, they reduce their surface charge and promote the convergence of erythrocytes and their faster agglomeration.
- Infections, inflammatory diseases, tissue destruction.
- Other conditions leading to increased levels of fibrinogen and globulins in plasma, such as malignant tumors, paraproteinemia (for example, macroglobulinemia, multiple myeloma).
- Myocardial infarction.
- Pneumonia.
- Liver diseases - hepatitis, liver cirrhosis, cancer, etc., leading to severe dysproteinemia, immune inflammation and necrosis of liver tissue.
- Kidney diseases (especially those accompanied by nephrotic syndrome (hypoalbuminemia) and others).
- Collagenoses.
- Diseases of the endocrine system (diabetes).
- Anemia (ESR increases depending on severity), various injuries.
- Pregnancy.
- Poisoning by chemical agents.
- Elderly age.
- Intoxication.
- Injuries, bone fractures.
- Condition after shock, surgical interventions.
The most significant increase in ESR (up to 50–80 mm/h) is most often observed with:
- paraproteinemic hemoblastoses - myeloma, Waldenström's disease
- connective tissue diseases and systemic vasculitis - systemic lupus erythematosus, periarteritis nodosa, scleroderma, etc.
Decrease in ESR value
- blood thickening
- acidosis
- Polycythemia.
- Sickle cell anemia.
- Spherocytosis.
- Hypofibrinogenemia.
- Hyperbilirubinemia.
- Fasting, decreased muscle mass.
- Taking corticosteroids.
- Pregnancy (especially 1st and 2nd semester).
- Vegetarian diet.
- Overhydration.
- Myodystrophies.
- Severe symptoms of circulatory failure
The most common reason for a significant decrease in ESR is an increase in blood viscosity in diseases and syndromes accompanied by an increase in the number of red blood cells (erythremia, secondary erythrocytosis).
CONCLUSION
In conclusion, it should be noted that, despite its widespread use in clinical practice, the determination of ESR has limited diagnostic value. At the same time, most authoritative experts in the field of clinical medicine clearly point out that the diagnostic capabilities of this method are far from being fully used, and the main problem for the practice of domestic CDL lies in the methodological features of the test. The two methods presented, the Panchenkov method and the Westergren method for determining ESR, are very necessary methods, because with their help you can confirm various inflammations. But you need to be careful, because for research you need to strictly follow the rules of analysis using modern developments, which not only improve the quality of test results, but also significantly increase the safety of the patient and staff when taking blood samples. In the near future, it is planned to release multi-parameter smart cards, along with ESR, allowing to evaluate the anemia factor, aggregation factor, viscosity, hematocrit index and hemoglobin index.
Conclusions:
ESR is a nonspecific laboratory blood indicator; a change in ESR can serve as an indirect sign of the current inflammatory process and is relevant to this day;
When studying ESR using different methods, different results are obtained;
The ESR from venous blood is significantly higher than from capillary blood;
The Panchenkov method is technologically outdated and takes longer than other methods for determining ESR;
When performing ESR using the Panchenkov method, it is more difficult to comply with the sanitary and epidemiological regime.
Head of the Clinical Diagnostic Laboratory Tatyana Shah
Increasing ESR
A similar result may be caused by the following pathologies:
- Infection or inflammation.
- Connective tissue diseases (RA, SLE, vasculitis, etc.).
- Burn disease.
- Neoplasms of different etiology and localization.
- Myocardial infarction. In the post-infarction period, the maximum occurs after about 7 days (in this case, you need to contact a vascular surgeon).
- Anemia. These diseases are characterized by a decrease in red blood cells and an increase in their sedimentation rate.
- Injury.
- Amyloidosis (a pathology characterized by the formation of a pathological protein - amyloid).
Despite the discrepancy between normal limits, if a complete blood count of ESR showed an increase in this indicator, this does not necessarily indicate the presence of a problem. This result also occurs in healthy individuals: in women during the menstrual cycle, during pregnancy, or in overweight individuals. This also occurs when taking a number of medications, so you should consult your doctor in advance.
Natural causes of increased erythrocyte sedimentation rate
If the ESR is elevated, this can be caused by various reasons, but these are not always malignant tumors.
- In women, ESR increases during menstruation, as well as during pregnancy. The absolute norm for a pregnant woman will be 44-46 mm/hour, but remember that at the beginning of pregnancy, ESR, on the contrary, is reduced.
- The cause of increased subsidence can be stress, excessive tension and emotional stress.
- This indicator also increases with allergic reactions of the body.
- Various reactions, inflammation due to cuts or splinters are also the cause.
- Pay attention to the medications you take - sometimes the ESR increases because of them.
The reasons given above are not the most serious. If we are talking about natural processes in a woman’s body, there is absolutely no need to worry. It’s another matter when the ESR increases due to internal inflammation, which can develop into a dangerous disease.
Therefore, it is so important not to resort to self-medication, and find out from your doctor the reason for the high rate.
Decrease in ESR
A reduced erythrocyte sedimentation rate often signals the presence of water-salt metabolism disorders or active muscular dystrophy. This is often a symptom of erythrocytosis, leukocytosis, hereditary spherocytosis, hepatitis and DIC syndrome. In addition, a similar result is characteristic of polycythemia and the conditions leading to it (CHF or damage to the pulmonary system). Low ESR can also be a consequence of fasting, vegetarianism, taking a number of steroid hormones, and is also often detected in the 1st and 2nd trimester of pregnancy.
You can take an ESR test and undergo other hematological tests at our MedArt medical center. With the help of modern equipment, you can find out absolutely accurate indicators, and highly qualified workers will competently advise you on this or that issue.