Blood is the connecting thread between the entire human body. She is like rivers that feed and give life to man. Almost every event that occurs in our body affects the circulatory system. Pregnancy rebuilds a woman’s entire body, including the circulatory system. The composition of the blood also changes. As a result, the expectant mother may develop thrombophilia. When pregnancy occurs, a woman suffering from thrombophilia should immediately discuss with her doctor medication support and a test regimen that will allow her to monitor her blood condition and prevent complications in time.
Why is thrombophilia dangerous during pregnancy and what kind of disease is it?
Planning pregnancy with thrombophilia
Thrombophilia is a disease in which blood clotting is significantly increased, which entails a risk of developing thrombosis.
The blood clots themselves, under normal circumstances, protect the human body and do not cripple it: if a vessel is damaged, a blood clot forms, which clogs the damaged vessel. But with thrombosis, blood clots can form in completely healthy vessels, blocking the flow of blood and nutrients to the tissues.
A woman may have thrombophilia and plan to become a mother. This is quite natural. But it is not so rare that the disease develops during pregnancy.
In both cases, thrombophilia can become dangerous for both the fetus and the pregnant woman, so it is necessary to monitor the blood condition in order to monitor the development of the disease in time and begin treatment as early as possible.
A little about thrombosis
Against the background of increased viscosity, a blood clot can form at any time, and under such circumstances it will look like a natural physiological process, for example, against the background of dehydration. When platelets come close to each other, they undergo friction and stick together into entire conglomerates. Thrombosis often causes strokes. Therefore, doing an electrocardiogram, even with enviable regularity, is not enough: it is important to keep the viscosity situation under control.
Hereditary thrombophilia and pregnancy
A disease that affects the circulatory system cannot but affect the body as a whole. Thus, thrombophilia contributes to a woman’s ability to conceive a child. Due to insufficient blood supply to the uterus and pelvic organs, the embryo may not take root or may soon be rejected by the body.
The disease may be hereditary. During pregnancy, the development of genetic thrombophilia will be influenced by genes responsible for blood clotting and genes of enzymes that control folic acid metabolism.
If among your closest relatives there are people suffering from this disease, you should undergo a molecular genetic study when planning a pregnancy. And, if it turns out that the disease is inherited, it is advisable to immediately begin treatment in order to avoid problems with the health of the expectant mother and fetus.
Risks for mother and baby
The main danger lies in the formation of blood clots.
Often, after childbirth, a new mother may develop varicose veins. Blockage of blood vessels can negatively affect both the fetus, which will experience oxygen deficiency, and the expectant mother herself. Because of this, the possibility of miscarriage or premature birth, heart attack or stroke may increase significantly. In the early stages, excessively thick blood can lead to a frozen pregnancy. Therefore, it is so important to visit a doctor on time and fully follow his recommendations. If you have any doubts about the prescribed treatment, immediately consult with several doctors, so you can eliminate the risk of medical error or negligence.
What are the dangers of thrombophilia during pregnancy?
Why is thrombophilia dangerous for a pregnant woman? Because a new life with its own circulatory system is born in her body. A person has two circles of blood circulation - large and small. A pregnant woman has another blood circulation, called the placental, through which blood, along with nutrients, flows directly to the fetus. If the blood is too viscous, then its flow rate will be lower than it should be to properly provide the unborn child with oxygen and all other useful substances.
In addition, to protect a woman during childbirth from extensive blood loss, the body increases blood clotting. But in case of illness, blood already coagulates very quickly, so the risk of blood clots increases several times. A thrombus can completely block even large vessels, or significantly reduce its lumen. This will also prevent blood from flowing freely to the fetus.
As a result, with thrombophilia during pregnancy, the consequences for the child may entail the threat of a frozen pregnancy, miscarriage, or the birth of a child with developmental defects. Oxygen starvation can cause developmental delays in the newborn and weak immunity. But the disease can also damage the body of the pregnant woman herself. The consequences may be the appearance of varicose veins, very severe toxicosis that threatens the woman’s life, premature placental abruption with heavy blood loss. If a blood clot blocks a blood vessel in the brain, the disease can be fatal.
What are the consequences of the state of hemoconcentration?
Why is hemoconcentration (blood thickening) dangerous during pregnancy? Both the mother and her unborn baby can suffer from this pathology. The doctor immediately puts this situation under control, since the following consequences may occur:
- Varicose veins,
- The appearance of blood clots
- Stroke,
- Heart attack.
For a child, this situation is even more dangerous. He faces:
- Oxygen starvation,
- Pathological development,
- Fading pregnancy
- Risk of miscarriage,
- Premature birth.
Diagnosis of thrombophilia in pregnant women
It is difficult to diagnose thrombophilia during pregnancy, so at the slightest symptoms of the disease you should consult a specialist. There are not many signs, and they are not always interpreted in favor of the disease.
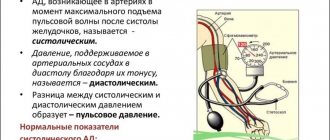
Severe toxicosis, blood clotting disorders (a network of burst vessels or bruises under the nails), high blood pressure, and convulsions are indicative.
Blood clots can form in any vessels and cause pain in various parts of the body, even a pre-infarction condition. The diagnosis of “thrombophilia” can also be suspected by the reaction of the fetus: if it does not receive a sufficient amount of nutrients, it may become excessively active or, on the contrary, freeze.
Analysis for thrombophilia during pregnancy and its planning
In order to detect or exclude the disease, two blood tests are taken - a general blood test and a coagulogram, a comprehensive analysis of blood clotting indicators.
Blood for a coagulogram is taken from a vein on an empty stomach (it is advisable not to eat 12 hours before taking the test). Before a blood clotting test, you should not:
- smoke;
- take alcohol and psychotropic substances;
- eat fatty and spicy foods;
- Warn the laboratory assistant about taking medications if it is not possible to refuse the medications.
It is especially important to undergo tests for thrombophilia when planning pregnancy, if there are cases of the disease in the family, so that the diagnosis of a hereditary disease will help start treatment on time.
Causes
While carrying a baby, the expectant mother is faced with a huge number of tests. A general blood test and hemocoagulogram are mandatory tests that are included in the recommended list of laboratory tests performed during pregnancy.
“Thick” blood is a clinical concept that is defined when the amount of formed elements in the blood is significantly increased. Typically, various thrombus formation disorders lead to the development of this situation during pregnancy. These pathologies can appear both in the early and late stages of pregnancy.
It should be noted that normal blood is quite liquid. This physiological feature is necessary for its transport and nutritional functions to be fully realized.
There are quite a lot of different nutrients dissolved in the blood, as well as oxygen. All these elements are needed by the fetus for its active growth and development.
The development of pathological disorders associated with the formation of thick blood is caused by the following causes:
- Individual characteristics of the expectant mother. If a woman had any hematological disorders before pregnancy, then during pregnancy they will progress significantly. This situation usually occurs in families where several members have various diseases of the cardiovascular system. A history of heart attack or stroke in close relatives of a pregnant woman is also a predisposing factor to increased thrombus formation.
- Violation of the drinking regime. Insufficient intake of water into the expectant mother's body can lead to her blood becoming thicker. This violation occurs quite often if a woman suffers from toxicosis. Frequent vomiting contributes to dehydration, which leads to severe blood thickening.
- Insufficient supply of essential vitamins and microelements. Vitamin balance is very important during all periods of pregnancy. Carrying a baby is a very energy-intensive time. To carry out all biological reactions, enzymes are needed, which cannot be formed in the mother's body without certain vitamins and microelements.
- Frequent consumption of sweets and other “fast” carbohydrates . A large amount of sugar entering the blood leads to a significant change in its viscosity. If the expectant mother eats a lot of sweets and candies throughout her pregnancy, this can not only contribute to increased blood clot formation, but even lead to the development of signs of diabetes mellitus.
- Oversaturation of the body with iron-containing drugs . These drugs are usually prescribed to pregnant women who have had a decrease in hemoglobin during pregnancy. Excessive intake of iron-containing drugs can lead to an increase in platelets in peripheral blood.
- Impaired functioning of the spleen . This organ is necessary for the body to maintain optimal concentrations of blood cells. Hypersplenism is a pathological condition that is characterized by significant disturbances in the functioning of the spleen.
This pathology, which occurs during pregnancy, also contributes to the progression of thrombosis.
It is important to note that there are a number of specific pathologies that occur mainly only during pregnancy. antiphospholipid syndrome can lead to an increase in blood viscosity and disruption of its fluidity Doctors note that the incidence of this pathology is only growing every year.
Severe blood loss or traumatic shock resulting from some type of injury may also cause baseline blood counts to change. These pathologies can also appear if a pregnant woman shows signs of internal bleeding. This condition is already extremely unfavorable and requires urgent medical attention.
- Finger joints hurt during pregnancy: causes of pain in the hands
Calculate gestational age
Treatment of thrombophilia when planning pregnancy
Medicines, diet and strict regimen are the three main directions in the treatment of the disease.
Medicines for thrombophilia are anticoagulants, drugs to reduce blood clotting, they are prescribed individually and exclusively by specialists.
Additionally, for the treatment of thrombophilia when planning pregnancy, it is recommended to take Omega-3. Taking Omega-3 reduces blood viscosity, reduces the production of thromboxane, which constricts blood vessels, and improves the fluidity of red blood cell membranes. All this has an antithrombotic effect when taken on a regular basis. Therefore, doctors recommend a continuous course of Omega-3 to prevent thrombosis, especially for women with high blood clotting rates.
The Pregnoton Mama complex, recommended for pregnant women and preparation for pregnancy, contains Omega-3 in an effective dosage. You can take the drug throughout the entire period of pregnancy.
How to influence the situation
There are several simple ways to bring your blood condition back to normal. First of all, during a consultation with a cardiologist, they will recommend establishing a drinking regime using purified water, juices and fruit drinks. But tea and coffee, which cause a diuretic effect, should be consumed in doses. In addition, it is important to balance the diet by removing excess cholesterol and sugar, which increase viscosity, from the menu. The diet needs to be expanded with vegetables and sea fish, vegetable proteins, fruits - sour and sweet and sour.
Liquefaction also occurs from some herbal infusions - lemon balm, hawthorn, gingko biloba, willow. Seafood, nuts, vegetable oils, raspberries, viburnum and sea buckthorn are also healthy. Be that as it may, paying close attention to your own diet and drinking regime will only be beneficial - it will help prevent heart attack, stroke and other consequences of a dangerous condition!