A normal umbilical cord consists of three vessels - two arteries and one vein. Sometimes, instead of two arteries, only one artery and one vein are formed in the umbilical cord, thus, only two vessels are identified in the umbilical cord. This condition is considered a malformation of the umbilical cord, but this defect does not have any effect on the postpartum condition of the child and its further development.
Structural features
A normal umbilical cord connects the front of the abdominal wall to the placenta (an organ necessary for the bond between mother and baby). A properly formed umbilical cord has the following components:
- Two umbilical arteries. They carry blood from the fetus to the placenta.
- Umbilical vein. It works like arteries, only in the opposite direction.
- Urachus. This is the name given to the duct that connects the placenta to the baby’s bladder.
- Wharton's jelly. It is a connective matter that protects the vessels of the umbilical cord.
- Vitelline duct. Connects the intestines of the embryo with the yolk sac (responsible for hematopoiesis and the production of germ cells).
What is the pathology?
The only umbilical cord artery in the fetus is a pathology in which the structure of the connecting element changes (instead of two - one). This happens quite often: the probability is 1:20 for a multiple pregnancy and 1:200 for a singleton pregnancy. The risk of developing pathology increases if the expectant mother has diabetes.
One artery may be absent from the very beginning of pregnancy or may lose its function at any time (eg, atrophy). The structure of the umbilical cord is clearly visible on ultrasound from twenty weeks. Most often, a single umbilical cord artery is a single pathology and is not associated with any congenital anomalies (in 75% of cases). However, there is a chance that the child has developmental disabilities (25%). Most often, the pathology problem is accompanied by problems with the heart, kidneys, intestines and bones.
What should be the length of the umbilical cord
This largely depends on individual indicators - there is no strict norm in this case, but usually the length falls within the range of 40 to 70 cm. It is important here that the fetus can move in the womb. But if the umbilical cord is too long or too short, this can lead to certain pathologies and problems.
The length of the umbilical cord may depend on genetic factors, the number of births and many other factors - they cannot always even be determined. For this reason, expectant mothers should be constantly under the supervision of doctors.
Diagnostics
To give birth to a healthy baby, any pregnant woman must be constantly monitored by a doctor and undergo all tests. If there is any suspicion, the unborn child must be carefully examined for various developmental defects and markers of genetic diseases. Don't be afraid of all these studies, because there is nothing more important than health.
The following methods will help identify the only umbilical cord artery during pregnancy:
- Ultrasound (ultrasound examination). The bladder must be full before passing.
- Doppler. Determines the presence and speed of blood flow.
- Examination by a gynecologist. Using special instruments, the doctor can listen to the baby’s heartbeat and, if there is any suspicion, prescribe additional examinations.
If a pathology is detected, doctors will suggest undergoing karyotyping of the fetus. This procedure involves the collection of amniotic fluid or chorionic villi, as well as detailed ultrasound and echocardiography.
The only umbilical cord artery during pregnancy can be seen on ultrasound during transverse scanning, in which the lumen of the vessels is best visible. Diagnosis of pathology is possible from the end of the first trimester. At earlier stages, the umbilical cord is not clearly visualized, so it will not be possible to make an accurate diagnosis. Difficulties may also arise if a woman has oligohydramnios, obesity, or multiple pregnancies.
Causes
Problems with the vessels of the umbilical cord are not fully understood, but most often they are associated with:
- infectious diseases that the pregnant woman suffered in the first trimester;
- intoxication;
- bad habits (alcohol, smoking, drugs or potent drugs);
- diabetes mellitus;
- radiation exposure, poor ecology, hazardous production;
- multiple pregnancy;
- chromosomal disorders.
The most dangerous period of pregnancy is 6-9 weeks. At this stage, the risk of pathologies of blood vessels, placenta and blood flow increases. Artery atrophy (one of them stops functioning) can be caused by: thrombosis, tumors, hematomas or nodes (on one of the arteries). It should be remembered that such conditions occur quite rarely, but require constant monitoring.
A woman's health condition can also lead to the formation of a single umbilical cord artery during pregnancy. Causes may include: diabetes mellitus, multiple pregnancy, kidney disease, heart disease.
Symptoms
Problems with the umbilical cord do not manifest themselves in any way in a woman. They can only be detected during ultrasound or Doppler ultrasound. But there are some symptoms that this pathology may be associated with:
- Increasing the duration of labor with a short umbilical cord. They can last more than 20 hours during the first birth, and more than 15 hours during repeated births.
- Vaginal bleeding, especially if there is a cord presentation (located near the cervix).
- Acute or chronic fetal hypoxia.
A lack of oxygen can be recognized by the following signs:
- Rapid heartbeat (more than 160 beats per minute). At a later stage, on the contrary, it can slow down to 120 beats per minute.
- Increased motor activity of the baby. Slowdown may occur over time.
- Meconium in amniotic fluid.
Screening for detection of congenital fetal diseases during pregnancy
Category: Reminders for the public.
Screening during pregnancy is a whole range of studies that allows parents and doctors to obtain the most complete information about the health of their unborn baby. Screening reveals many congenital and physical characteristics. How and when is screening done during pregnancy?
What is screening during pregnancy and why is it done?
Screening during pregnancy is a set of examinations that includes ultrasound and biochemical analysis of venous blood for hormones. As a rule, screening is carried out three times - in the first, second and third trimester.
Early detection of pathologies is very important. This makes it possible to begin treatment of genetic diseases as early as possible and, if not completely cure them, then at least relieve the symptoms as much as possible. If during the examination the doctor notices any abnormalities, the pregnancy is monitored especially carefully, which makes it possible to prevent the development of complications or premature birth. If the detected pathologies turn out to be too severe and incompatible with life, the doctor will refer the patient to terminate the pregnancy for medical reasons.
Screening during pregnancy is harmless for both mother and baby. This is a fairly accurate study, although it should be clearly understood that it does not provide a 100% guarantee. The accuracy of screening depends on many factors - the professionalism of the researchers, the woman’s compliance with the rules for preparing for the examination, and other factors.
First screening during pregnancy
The first screening during pregnancy is carried out between the 11th and 13th weeks. There is no point in undergoing this examination earlier - until the 11th week of pregnancy, many indicators are practically impossible to determine.
The study includes two medical tests - an ultrasound and a blood test.
Ultrasound
Using an ultrasound, the doctor determines the exact duration of pregnancy, evaluates the child’s physique, its size (head circumference, length of limbs, height), the functioning of the heart muscle, the symmetry of the brain, the volume of amniotic fluid, the structure and size of the placenta, as well as the condition and tone of the uterus. For each of these parameters there are normal indicators with which the doctor will compare the results. For an 11-13 week pregnancy these norms are:
- CTP (coccygeal-parietal size, that is, the length of the fetus from the crown to the coccyx) is 43–65 mm. If this figure is higher than normal, it means the child will be large. A deviation to the smaller side indicates slow development (the reason for this state of affairs is often a hormonal imbalance or infectious diseases suffered by the expectant mother), genetic pathologies or fetal death (in this case the heart will not be heard). However, this may also be due to a banal error in determining the timing of pregnancy.
- BDP (biparietal size, that is, the distance from temple to temple) - 17–24 mm. A high BDP means a large fetus, but only if all other indicators indicate the same. Otherwise, we may be talking about a brain hernia or hydrocephalus. A low BDP indicates slow brain development.
- TVP (thickness of the collar space) - 1.6–1.7 mm. Deviation from this norm (TVP above 3 mm) is considered a sign of some severe chromosomal pathologies - Down syndrome, Edwards syndrome, etc. However, one should not panic ahead of time - no one will make such a serious diagnosis only on the basis of TVP. To confirm, you need to take a blood test for hormones and do a biopsy of the outer dense membrane of the embryo for subsequent research.
The length of the nasal bone is 2–4.2 mm. A nasal bone that is too small may indicate a pathology or simply that the baby will have a snub nose. HR (heart rate) - 140–160 beats per minute. A slight (up to 40 beats per minute) deviation in one direction or another is considered normal.
The size of the chorion, amnion and yolk sac. The chorion is the outer membrane of the fetus, which will eventually become the placenta. If it is located on the lower wall of the uterus, they speak of chorion presentation. This is a potentially dangerous situation that can lead to miscarriage, in which case bed rest is recommended for the pregnant woman.
Amnion is the inner membrane that holds amniotic fluid. The normal volume of amniotic fluid at 11–13 weeks is 50–100 ml.
The yolk sac is an embryonic organ that, in the first weeks of the fetus’s life, plays the role of some internal organs that will be formed later. By the time of the first screening, the yolk sac should practically disappear (then the examination form will indicate “not visualized”). If its size is about 6 mm, then the fetus may have certain pathologies.
Cervix. Normally, its length at the time of the first screening is 35–40 mm. A shorter cervix means a risk of premature birth.
Ultrasound is performed in two ways - transabdominal, in which the ultrasound machine sensor is located on the abdomen, and transvaginal, in which it is inserted into the vagina. Transvaginal ultrasound provides more complete and accurate information, but is usually performed only in the first trimester. This method is usually used when examining overweight women, since the fat layer in the abdominal area does not allow a detailed examination of the fetus and uterus.
It is necessary to prepare accordingly for an ultrasound. Before a transabdominal ultrasound, it is advised to drink about a liter of water so that at the time of the examination the bladder is full - then the uterus will shift slightly towards the abdomen and the picture will be clearer. With a transvaginal ultrasound, the degree of bladder fullness does not matter at all, but before the examination it is better to go to the toilet - it will be more comfortable. Before the examination, you need to take a shower or freshen up with wet wipes. The accumulation of gases can distort the results of ultrasound, no matter what method it is performed. Therefore, expectant mothers suffering from flatulence are advised to take anti-flatulence medications the day before the examination and not eat anything that produces gas.
Blood analysis
Biochemical screening, also called a dual test, is done to determine the level of two hormones (hence the name) - free b-hCG and PAPP-A.
- b-hCG (human chorionic gonadotropin) begins to be produced from the first days of pregnancy. Its amount gradually increases until about the 9th week, and then begins to gradually decrease. On average, for a period of 11–13 weeks, 50,000–55,000 mIU/ml is considered normal. An elevated level of hCG may indicate a multiple pregnancy, or, in the worst case, genetic pathologies of the fetus or the presence of diabetes mellitus in the mother. Reduced hCG is typical for frozen pregnancy, ectopic pregnancy, fetal death, or certain malformations (Patau syndrome and Edwards syndrome).
- PAPP-A is plasma protein A. The maintenance norm for a period of 11–13 weeks is 0.79–6.01 mU/l. Low PAPP-A is a sign of chromosomal pathologies such as Down syndrome and Edwards syndrome, fetal death and miscarriage, fetal malnutrition (underweight) and preeclampsia.
- High PAPP-A is a sign of multiple pregnancy, large fetal size or low placenta.
In order for the blood test to provide the most accurate information, it must be taken on an empty stomach, at least 8 hours after the last meal. 2-3 days before the test, you should refrain from fried, fatty, spicy, smoked foods, chocolate, nuts, and seafood. It is also recommended not to have sexual intercourse. All this is not so significant, but it can affect the result in one way or another.
Second screening during pregnancy
The second screening during pregnancy is carried out at 16–20 weeks. Like the first one, it consists of the same two stages - ultrasound and blood tests.
Ultrasound
This time, the doctor determines not only the size, but also the position of the fetus and its bone structure, the condition of the internal organs and the place of attachment of the umbilical cord, as well as the volume of amniotic fluid. Here are the approximate basic indicators of the norm for a period of 16–20 weeks:
- BPR - 26–56 mm.
- DBC (femur length) - 13–38 mm.
- KDP (humerus length) - 13–36 mm.
- OG (head circumference) - 112–186 mm.
AFI (amniotic fluid index, that is, the volume of amniotic fluid) - 73–230 mm. Oligohydramnios can negatively affect the condition of the child’s bone structure and the development of his nervous system.
Localization of the placenta. There is some risk only when the placenta is located on the anterior wall of the uterus - with such a localization, placental abruption is possible.
Umbilical cord. One of the most important parameters is the location of the umbilical cord attachment. Marginal, split or membrane attachment is fraught with fetal hypoxia and difficulties during childbirth; it often becomes an indication for cesarean section. The umbilical cord is supplied by 2 arteries and 1 vein, although sometimes only one artery is present. This can cause fetal hypoxia, heart defects, disturbances in the child’s cardiovascular system, and cause low body weight in the baby. However, if all other tests and examinations do not show deviations from the norm, there is no need to worry.
Cervix. The length of the cervix at this stage should be 40–45 mm. A short cervix means a risk of miscarriage.
Visualization. Unsatisfactory visualization can be caused both by the position of the fetus or the excess weight of the expectant mother, as well as by edema or hypertonicity of the uterus.
Blood analysis
As during the first screening, during the second a blood test is taken for b-hCG, and the level of free estriol and AFP is also checked. Here are the norms for their maintenance at 16-20 weeks of pregnancy:
- b-hCG - 4.67-5-27 ng/ml.
- Free estriol is a hormone, the level of which can be used to judge the condition of the placenta. The normal range is 1.17–3.8 ng/ml. Elevated estriol is typical for multiple pregnancies or a large fetus. Reduced - for the threat of miscarriage, placental insufficiency, anencephaly and Down syndrome.
- AFP is a protein produced in the fetal gastrointestinal tract. The norm is 15–27 U/ml. A slightly lower AFP may mean that the gestational age was determined incorrectly (slightly underestimated). If the AFP is very low, the cause may be Edwards or Down syndrome, the threat of miscarriage or fetal death. High AFP is characteristic of neural tube pathologies, esophageal atresia, and Meckel's syndrome. High AFP is also possible in women who have had an infectious disease during pregnancy.
Third screening during pregnancy
The third screening during pregnancy is carried out at 30-43 weeks. Based on the results of this screening, the doctor decides on the need for a cesarean section or the possibility of a natural birth. The basis of the third screening is the same ultrasound. Sometimes Doppler sonography is prescribed - a study of the functioning of blood vessels. Here are the approximate norms for this stage of pregnancy:
Ultrasound
- BPR - 67–91 mm
- DBK - 47–71 mm
- WPC - 44–63 mm
- Exhaust gas - 238–336 mm
- IAZh - 82-278 mm
The thickness of the placenta is 23.9–43.8. A placenta that is too thin is not a particularly dangerous deviation from the norm. The reason may be the woman’s miniature physique, infectious diseases she has suffered, or hypertension. An excessively thick placenta is a sign of anemia, diabetes, and Rh conflict. An indicator such as the degree of maturity of the placenta is also taken into account - at a period of 30–35 weeks, the 1st degree of maturity is considered normal. If the placenta thickens and ages too quickly, premature birth, fetal hypoxia and slow development are possible.
Prenatal screening is very important and should not be neglected. Timely identified pathologies and deviations from the norm can save the life and health of your child. This is worth remembering, especially for those parents who refuse an examination for fear of finding out that the baby’s development is not going according to plan.
Accompanying illnesses
Women with a single umbilical cord artery often have a second bud, but it has simply atrophied. Atrophy of the left artery, in contrast to the right, is often combined with developmental anomalies in the baby. For example, such a pathology may be accompanied by malfunctions of the heart and genitourinary system.
Experts noted that the number of cases where one artery was present in pregnancies that ended in miscarriage due to trisomy has become more frequent. This trend was also noticed in women with dark skin and diabetes. The absence of one of the arteries increases the incidence of perinatal mortality associated with serious malformations by 4 times.
Scientists conducted a study on the relationship between problems with arteries and developmental anomalies. The result revealed that 15 fetuses (out of 30) have health problems. Moreover, 12 of them were found to have serious pathologies: heart defects, skeletal defects, and diaphragm defects. In some cases, abnormalities may appear after childbirth.
Danger to the fetus
Although it was said above that children often have concomitant pathologies with a single umbilical cord artery, there may be no consequences. In most cases, the pathology does not have a serious impact on the baby either before or after birth. Most often, one artery is able to cope with the increased load. Therefore, if the doctor sees this defect, you should not be upset right away. You will just have to undergo additional examinations and monitor your condition more carefully.
In some cases, there is a risk that the child has developmental abnormalities: chromosomal changes, serious problems with the heart, blood vessels, urinary system, abdominal organs, etc. That is why it is important to identify the presence of other anomalies as early as possible. It should be remembered that single artery syndrome without other pathologies is not considered a sign of Down syndrome or other chromosome-related disorders.
If the pathology is accompanied by other defects, there is a high risk to the baby’s health. The consequences of a single umbilical cord artery in the fetus may be as follows:
- frozen pregnancy (in long term – intrauterine death);
- developmental delays;
- chronic hypoxia;
- malnutrition.
Variants of umbilical cord pathologies
Here are some undesirable situations and problems that occur during the development of the baby or already during childbirth:
- Entanglement of the fetus. This is most often observed if the cord is too long - more than 70 cm. The danger of this situation is obvious: with a certain location of the umbilical cord, it can pinch the child’s vital organs or contribute to suffocation. If there is such a danger, doctors prescribe a caesarean section to avoid such serious consequences during natural childbirth.
- Formation of nodes. If the umbilical cord tissue becomes twisted and tangled, knots may appear. Most often this happens in the early stages. The dangers here are serious - this is a disruption of the blood supply to the fetus, and a decrease in the required level of oxygen and nutrients. There may also be problems during childbirth. The solution is the same as in the previous case: be under the supervision of doctors who, in case of an emergency, will decide on surgical intervention.
- Umbilical cord prolapse. This is a process in which the umbilical cord can penetrate the cervix and even the vagina as soon as the amniotic fluid has broken. This is a risky situation for childbirth, because there is a risk of developing oxygen deficiency and fetal hypoxia. In this case, emergency hospitalization of the woman in labor and the adoption of appropriate measures to help the mother and child are indicated.
- Cysts. If the umbilical cord is formed with a small number of cysts, there may be no symptoms and no serious prognosis. The problem appears when there are many such cysts and they have a certain structure. There are often cases when cysts are analyzed after birth - then the umbilical cord is sent for histological examination.
- Vascular thrombosis. This is a rarer pathology that can occur if the woman carrying the child suffers from diabetes or certain blood clotting pathologies. The prognosis for such a problem is usually serious and unfavorable, but a thorough examination is required.
- Umbilical cord hernia in newborns. This is an anomaly in which the child’s abdominal organs, covered by the visceral peritoneum, protrude through the abdominal (anterior) wall. The actions of doctors depend on the degree of the hernia. In difficult cases, a woman must give birth by caesarean section in a specially prepared operating room. The child is also indicated for surgical intervention.
The umbilical cord, despite the fact that visually it looks very simple, is the most important organ in the life of a developing baby. That is why there are now many studies that help determine his condition and position in order to reduce the risks of pathologies or take timely actions that will save the child.
Correct behavior of a pregnant woman
Most women, after making such a diagnosis, are confused and very worried. They are concerned about intrauterine development and the future health of the baby. No medicine or remedy will add a missing artery, but you can minimize the risk of serious consequences.
Therefore, a pregnant woman should:
- stress less;
- free yourself from hard work;
- prevent constipation;
- maintain a daily routine;
- eliminate psycho-emotional stress;
- walk more and relax;
- eat more fruits and vegetables.
If you follow these simple recommendations and constantly monitor the condition of the fetus, then there will be no negative consequences. The only umbilical cord artery during pregnancy in this case may not cause any problems.
A few more words about functions
We have already said that the umbilical cord is responsible for ensuring that the fetus is provided with all the necessary nutrients during development. These are proteins, fats and carbohydrates that are obtained through the mother's blood. But it is important to understand that this is not only about a biological connection. Numerous studies show that the umbilical cord also forms the so-called mental connection between the child and the mother. It is for this reason that a woman who is carrying a baby is advised to carefully monitor her condition, try to avoid nervous tension and be in a good mood. As it turns out, the baby is very sensitive to any psychological experiences of the mother - and the umbilical cord is also involved in this process. That is why it is necessary to understand the functions of the umbilical cord and know how important it is in the pregnancy process.
Management of pregnancy during pathology
As mentioned above, if there is a pathology, you need to monitor your well-being and the condition of the baby (especially the nature of the movements). Any changes or suspicions should be reported to the doctor managing the pregnancy. He will monitor the woman’s condition over time and prescribe a full examination if problems are detected.
Additional research will also be needed:
- Ultrasound at 28 weeks;
- screening and full examination at 32 weeks;
- weekly Doppler.
If a blood flow disorder or a delay in the child’s development is suddenly detected, the woman will be offered hospitalization. There they will provide supportive therapy until the baby’s condition stabilizes. You should be aware that a child born as a result of such a pregnancy will need careful monitoring (to identify serious abnormalities).
Opinion of gynecologists
At the moment, there is no consensus on how dangerous it is to have a single umbilical cord artery during pregnancy. Reviews from doctors only agree that careful monitoring of the woman and baby is necessary. Experts believe that the most important research methods are ultrasound and Doppler. They are carried out at certain periods, but if there are problems, examinations are done more often.
In general, gynecologists think like this:
- There is some connection between the absence of one artery and pathologies of the baby’s organs and systems.
- If, in addition to this problem, there are other developmental defects, then the risk of chromosomal diseases is high. In this case, it is worth undergoing amnio- or cordocentesis.
- If there is nothing suspicious other than the arteries, then there is a small risk of developmental disorders. To clarify the situation, it is better to undergo a karyotyping procedure.
According to reviews, a single umbilical cord artery during pregnancy is not too scary, and is not that rare. Many women claim that everything went well and ended with the birth of a healthy baby.
Material and methods
A screening Doppler study and analysis of spectrograms of uteroplacental and fetal blood flow were carried out in 357 pregnant women. The study was carried out at various stages of the gestational period, starting from 19-20 weeks of pregnancy. Emphasis was placed on studying changes in uteroplacental perfusion in low-risk pregnancies.
The uterine arteries were removed using the traditional method; the study was carried out bilaterally; blood flow was recorded both directly in the uterine and arcuate arteries. The average value from three consecutive measurements was taken as the final result. The separation of blood flow in the uterine and arcuate arteries was aimed at identifying higher pulsation indices (uterine artery) and lower ones (arcuate artery) for an in-depth analysis of changes in the systolic pulse wave and diastolic blood flow velocity.
To assess the state of blood flow, the following “angle-independent indicators” were used: systolic-diastolic ratio (SDR), resistance index (RI); The pulsatility index was also assessed. The SDO was taken as the basis for assessing uteroplacental perfusion. Systolic and diastolic blood flow velocity were subjected to separate analysis.
The exclusion criteria from the study were: hypertensive disorders in a pregnant woman, including preeclampsia, hypotension, connective tissue diseases, kidney pathology, collagenosis, diabetes mellitus, Rh sensitization, disorders in the hemostatic system. Thus, the study was conducted in patients with low-risk physiological pregnancies.
Prevention of complications
Since the pathology cannot be cured, some preventive measures can be taken. This will reduce the risk of complications and various pathologies.
A woman must do the following:
- Prepare for pregnancy in advance (quit alcohol and smoking, eat right, take vitamins, improve your health).
- Register on time (up to 12 weeks).
- Regularly visit the doctor managing the pregnancy, follow all his recommendations, and undergo examinations.
- Eat rationally. You should eat more foods containing fiber (fruits, vegetables, herbs). You should also give up junk food (fried, spicy, canned, etc.).
- Undergo Doppler testing, which shows the state of blood flow and any changes in the vessels. With its help you can see the presence or absence of deviations.
- Have an ultrasound scan on time, where the doctor will immediately see the baby’s growth retardation, low weight, fetoplacental insufficiency, and hypoxia.
- Do not refuse hospitalization if there is a threat of placental abruption or increasing fetal hypoxia.
- Enough rest and sleep.
- Avoid physical activity and various experiences.
The presence of a single umbilical cord artery during pregnancy is a serious pathology that requires constant monitoring by specialists. After diagnosis, a woman should not worry; in most cases, everything ends with the birth of a full-fledged child.
Results and discussion
According to the screening examination, among 375 pregnant women, Doppler indices were not impaired in 314 (83.7%) pregnant women; 53 (14.1%) had any disturbances in hemodynamic parameters. Thus, every seventh pregnant woman who came for a routine ultrasound examination had some kind of hemodynamic disturbances without expressed complaints or deterioration in health. The distribution of violations is shown in table
.
1
.
Table 1. Violations of hemodynamic parameters (n=53)
Unclassified disturbances of hemodynamic parameters included one case of a combination of blood flow disturbances in the middle cerebral and right uterine artery.
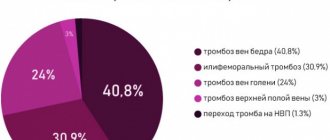
As can be seen from table. 1, the most common violation of blood flow in the mother-placenta-fetus system was a violation of uteroplacental perfusion (67.9%), with the vast majority being a unilateral violation (94.4%). It should be noted here that the critical condition of the fetus was noted when there were complaints from the patient about worsening fetal movements.
In table 2 shows hemodynamic disturbances in the uterine artery basin.
Table 2. Impaired uteroplacental perfusion (n=36)
As can be seen from table. 2, the bulk of the change in blood flow occurred in the left uterine artery (66.7%) versus the right (27.7%). The asymmetrical disturbance of hemodynamic parameters can be explained by an anatomical factor - dextroposition of the enlarged uterus, which leads to a change in the angle of origin of the uterine artery and increased resistance in it. In uncomplicated pregnancy, these changes are insignificant and do not lead to a deterioration in uteroplacental perfusion, however, with the growth of the pregnant uterus, the angle of origin of the uterine artery increases; A significant role in changes in uteroplacental blood flow, as the study showed, is played by the morbid background, which creates the basis for the implementation of predisposing unfavorable anatomical factors. This explanation for the asymmetrical disturbance of blood flow is supported by a study using contrast-enhanced multislice computed tomography, which revealed a more frequent origin of the uterine artery on the right at an angle of more than 90° [18].
Analysis of the incidence of primary disorders of uteroplacental perfusion was carried out from 18-19 weeks of pregnancy; the frequency of this distribution is shown in Fig. 1. As can be seen, the maximum frequency of hemodynamic disorders in the uterine artery basin was detected at the 32nd week of gestation (±3 days). This period of detection of disturbances in uteroplacental perfusion can be explained by the maximum tension of the compensatory and adaptive mechanisms of the pregnant woman’s body, as well as the transition of a compensated state to a subcompensated one.
Rice. 1. Frequency of detection of hemodynamic disorders in the uterine arteries.
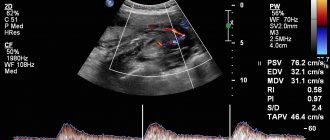
In each individual case, an in-depth analysis of the blood flow velocity curves in the uterine artery basin was carried out. In all cases, the blood flow velocity curves were characterized by two phases with a pronounced systolic peak wave and high diastolic velocity, and unidirectional blood flow in all phases of the cardiac cycle (Fig. 2).
Rice. 2. Spectrogram of normal blood flow in the uterine artery at 27 weeks of pregnancy.
In Fig. Figure 2 shows a spectrogram of normal blood flow in the uterine artery and numerical expressions of hemodynamic parameters. When analyzing the Dopplerogram, attention is drawn to the peak-shaped systolic impulse, high uniform diastolic blood flow with a moderate predominance in the early diastolic phase relative to the end diastolic phase. SDO corresponds to the norm for this stage of pregnancy: 2.11 (norm ≤2.6).
In Fig. Figure 3 shows a spectrogram of a unilateral disturbance of uteroplacental perfusion. When analyzing the Dopplerogram, attention is drawn to an increase in blood flow resistance (mainly due to a decrease in the diastolic component), equal to 3.35 (normal ≤2.4). Diastolic blood flow is preserved and uniform.
Rice. 3. Spectrogram of blood flow disturbances in the uterine artery at 37 weeks of pregnancy.
In Fig. Figure 4 shows a spectrogram of a unilateral disturbance of uteroplacental perfusion - SDO is 3.89 (normal ≤2.6). When analyzing the profile of the blood flow spectrum, attention is drawn to the unevenness of the diastolic component with the formation of a dicrotic notch in the early diastolic phase; the amplitude of the dicrotic notch corresponds to the level of end-diastolic blood flow velocity. Diastolic blood flow was maintained throughout the entire phase.
Rice. 4. Spectrogram of blood flow disturbances in the uterine artery at 23 weeks of pregnancy.
In Fig. Figure 5 shows a spectrogram of a pronounced unilateral disturbance of uteroplacental perfusion - SDO is 11.25 (normal ≤2.6). When analyzing the profile of the blood flow spectrum, attention is drawn to the unevenness of the diastolic component with the formation of a pronounced dicrotic notch in the early diastolic phase; the amplitude of the dicrotic notch in a number of cardiac cycles exceeds the level of end-diastolic blood flow velocity. Diastolic blood flow is preserved, but reaches extremely low values in the final phase (4.8 cm/s); zero and reverse blood flow is not recorded.
Rice. 5. Spectrogram of pronounced disturbances of blood flow in the uterine artery at 25-26 weeks.
It should be noted that an isolated disturbance of blood flow in the uterine arteries does not always lead to a disturbance of perfusion in the umbilical cord artery due to the anatomical separation of the vessels of the maternal and placental blood flow. At the same time, the preservation of low resistant properties of blood flow in the umbilical cord arteries (with impaired blood flow in the uterine artery basin) does not at all mean the absence of the initial stages of impairment of the fetal condition. The debut of tension in the compensatory mechanisms of fetal blood flow and their transition to a decompensated state can be reflected in the centralization of fetal blood flow—changes in fetal cerebral hemodynamics [11, 19].
It is necessary to identify the main pathogenetic causes of impaired perfusion parameters and increased blood flow resistance. These include: changes in the coagulological properties of blood (which leads to changes in blood fluidity and its laminar properties), changes in the number of vessels of predominantly small diameter (infarctions and thrombosis), a decrease in the diameter of vessels (vasculopathy of various origins) and spasm of arterioles [20].
It is vascular spasm that predominantly plays a key role in hemodynamic disturbances in the examined cohort of women: blood flow resistance increases due to a decrease in the diastolic component. An in-depth examination of all patients with impaired maternal-placental blood flow excluded the presence of coagulopathies of various origins according to an extended hemostasiogram and thromboelastogram. In turn, the absence of changes in the coagulation and anticoagulation systems of the blood allowed patients to be prescribed a drug that affects the platelet component of hemostasis (dipyridamole). Infarctions and thromboses predominantly of the uteroplacental bed were excluded based on clinical examination and pathomorphological examination of the placenta. All systemic vasculopathies (including preeclampsia) were also excluded during the initial examination of patients.
A detailed study of clinical, anamnestic and laboratory data in the examined contingent of pregnant women with a primary isolated disorder of uteroplacental perfusion revealed a number of asymptomatic and low-symptomatic forms of infectious and inflammatory processes of various localizations. This primarily concerned the ENT organs (chronic tonsillitis, chronic rhinitis, chronic sinusitis, chronic tubo-otitis) - 33.3% and the urinary tract (asymptomatic bacteriuria) - 28.6%. In a number of cases, the idiopathic (without established etiology) nature of the violation of uteroplacental perfusion was revealed - 28.6%. In 9.5% of cases, a combination of chronic infection of the ENT organs with asymptomatic bacteriuria was observed. Thus, the main factors of isolated disturbance of blood flow in the uterine arteries were extragenital foci of chronic infection (71.4%), which is the main prerequisite for an in-depth examination of this group of patients: consultation with an ENT doctor, control of urine sterility before birth.
The occurrence of transient hemodynamic disturbances in the presence of foci of chronic infection is explained by the theory of remote action of bacterial exotoxins. An indirect pressor effect on the muscular component of the vascular wall is exerted by exotoxins of living bacteria that are immunogenic, acting through cells of the immune system (macrophages, mast cells), thereby stimulating the latter to release cytokines, which have a vasopressor effect [21].
The appearance of a dicrotic notch, as one of the most unfavorable factors, is also explained by the pressor effect on the vessel, but against the background of a reduced response of the vascular wall to the pulse wave, when its response is delayed, which in turn leads to a decrease in blood flow velocity in the early diastolic phase. From a biophysical point of view, the extensibility of the vascular wall is the main factor in reducing blood flow resistance [22]. Thus, with an increase in the velocity gradient in systole, the energy of the pulse wave does not transform into stretching of the vessel, but is accumulated in its wall without the necessary increase in its diameter, and in the early diastolic phase, as the pulse wave declines, the vessel realizes the accumulated potential energy with a delay, which is graphically expressed in the appearance of a dicrotic notch in the spectrogram.
When a violation of hemodynamic parameters was detected, etiotropic therapy (sanitation of foci of chronic infection) and pathogenetic treatment (dipyridamole 75 mg/day in 3 doses) was recommended to the examined contingent of women; a number of women refused the proposed therapy. The effect of therapy was assessed 10-15 days from its start by changes in Doppler parameters. Data on the effectiveness of therapy are presented in table. 3. Etiotropic therapy for asymptomatic bacteriuria included fosfomycin trometamol 3 g once, followed by monitoring the sterility of urine before delivery; Therapy for inflammatory foci of the ENT organs was prescribed by an otorhinolaryngologist, included local antiseptic and physiotherapeutic treatment, and antibiotic therapy was administered according to indications (amoxicillin/clavulanate 375 mg 3 times a day for 7 days).
Table 3. Distribution of therapy effectiveness according to Doppler measurements
As can be seen from table. 3, the most unfavorable outcome (lack of improvement in hemodynamic parameters) was observed in the subgroup of women without any therapy (25.0%).
A significantly high rate of treatment effectiveness was observed in the subgroup of women who received both isolated etiotropic therapy and simultaneously etiotropic and pathogenetic therapy (17.9% in both subgroups).
There was a fairly low percentage of effectiveness of isolated pathogenetic treatment without sanitation of infectious and inflammatory foci (5.6%), as well as a low percentage of effective pathogenetic treatment against the background of ineffective etiotropic treatment (10.7%).
However, in the group of patients with idiopathic forms of uteroplacental perfusion disorders, pathogenetic treatment was effective in 37.5% of cases.
Thus, when hemodynamic disorders are detected in the uterine artery basin, it is necessary to conduct a targeted search for the etiological factor and take measures to eliminate it. The question of the need to add a pathogenetic component to etiotropic treatment - a drug with anti-aggregation, anti-adhesive and arteriodilating properties (dipyridamole) remains debatable, since the percentage of treatment effectiveness is determined by etiotropic therapy and does not increase with the addition of dipyridamole.
At the same time, as the study showed, isolated administration of dipyridamole (without etiotropic treatment) is extremely ineffective (7.1%). At the same time, in the group of women with idiopathic disorders of uteroplacental hemodynamics, the administration of dipyridamole demonstrated a higher percentage of effectiveness (37.5%), however, due to the small size of this group, further research is also required.