Spinal stroke is a type of myelopathy (diseases of the spinal cord of a neurological nature). Among all strokes it accounts for 1-1.5% of cases. Also, as in the case of the brain, it has two forms:
- Ischemic stroke (infarction) of the spinal cord - cessation of blood supply to a certain area of the brain and hypoxia.
- Hemorrhagic stroke is a rupture of a blood vessel and bleeding into the spinal cord.
Transient disorders of the spinal circulation and transient ischemic attacks (mini-strokes) can also be observed.
A distinctive feature of a spinal stroke is that it usually occurs at a younger age than a cerebral stroke, at 30-50 years. Without adequate treatment, it is extremely rarely fatal, but often leads to disability.
| Treatment in a hospital setting | |
| Complex treatment in the rehabilitation department of the 3rd category of complexity (1 day)* | 6600,00 |
| Complex treatment in a rehabilitation center of category 2 (1 day)* | 7900,00 |
| Complex treatment in a rehabilitation center of 1st category of complexity (1 day)* | 12300,00 |
| Accommodation of an accompanying person in the ward (1 day) | 1750,00 |
| Stay in the department (1 hour) | 110,00 |
| Individual care from a nanny at home (1 day) | 2300 |
| Additional care by a junior nurse (1 day) | 600,00 |
| Individual post of a junior nurse (1 day) | 1100,00 |
| Mechanotherapy | |
| Stander BALANS (duration 30 min.) | 600,00 |
| Motomed (duration 30 min.) | 600,00 |
| KRD (cardio training, duration 30 min.) | 600,00 |
| Rehabilitation therapy | |
| Locomotor therapy (duration 60 min.) | 750,00 |
| Locomotor therapy (duration 30 min.) | 580,00 |
| Kinesiotherapy (duration 60 min.) | 750,00 |
| Kinesiotherapy (duration 30 min.) | 630,00 |
| Occupational therapy (duration 60 min.) | 630,00 |
| Occupational therapy (duration 30 min.) | 520,00 |
| Speech therapy (duration 60 min.) | 550,00 |
| Speech therapy (duration 30 min.) | 450,00 |
| Speech therapy in the department | 450,00 |
| Psychological correction | 550,00 |
*Comprehensive treatment in the department includes:
- comfortable stay in the ward;
- balanced individual nutrition;
- constant medical and advisory assistance from the attending physician;
- classes in kinesiotherapy and ergotherapy halls using special equipment (balance trainer, bobat tables, motomed, wheelchair).
The Center also provides services:
- consultations with narrow specialists;
- laboratory diagnostic examinations;
- injections, manipulations and procedures.
Mechanism of pathogenesis
Spinal stroke accounts for approximately 1–1.5% of all CNS pathologies associated with acute hemodynamic disorders. The greatest prevalence occurs in the age category from 30 to 70 years, regardless of gender. The bulk of spinal strokes are of the ischemic type, and the overwhelming majority of lesions occur in the lower thoracic and/or lumbar region.
Impaired blood flow in the vessels causes oxygen deficiency (hypoxia), neural metabolic failures and hemorrhages in the pathological area. The sudden development of such conditions does not give the body time to react adequately, launch compensatory processes and rebuild the metabolism of neurons. A hemorrhagic zone is formed, the consequence of which is neurological necrosis. This condition is called “spinal stroke.”
Precursor stage
The first stage, the precursor stage, can last from a few minutes to several months. A short stage is inherent in the case of unexpected and rapid blockage of blood vessels by blood clots or in the case of a pinched artery, which is often observed with spinal injuries.
Speaking about a longer period of this stage, a gradual and slow cessation of blood circulation is assumed (for example, in the case of tumor growth or an increase in the size of an atherosclerotic plaque).
Preceding symptoms of this disease may be:
- occasional lameness;
- pain in the spine area;
- numbness of the limbs;
- feeling of crawling “goosebumps”;
- discomfort in the direction of branching of the spinal roots.
Intermittent claudication in neurology is a condition in which the patient feels a characteristic numbness of the lower extremities, weakness when standing for a long time or walking for a long time. The latter is explained by the resulting oxygen starvation in the spinal region, which is responsible for the mobility of the legs. In addition, the cause of such lameness may be poor blood circulation in the vessels.
Causes
Acute disorders of blood circulation in the spinal cord have a multifaceted etiology, but all factors, one way or another, lead to vascular damage - spasms, ruptures, compression, and the development of thromboembolism. Spinal stroke is divided into two main categories based on its causes:
- Primary vascular damage.
- Secondary hemodynamic disturbance.
The first group includes pathologies affecting the functioning of blood vessels:
- rare anomalies - aneurysms, defects of venous and arterial development with slow blood flow. Thinning of the tissues of the vascular walls leads to rupture and hemorrhage;
- deformation of the walls of blood vessels - atherosclerotic, varicose and similar disorders most often become the cause of ischemic stroke of the spinal cord;
- ruptures - damage as a result of spinal injuries, as a consequence of surgery, anesthesia, or puncture of the spinal column.
The second group consists of hemodynamic failures:
- anatomical and neurological abnormalities (hernias, displacements, osteochondrosis, spondylolisthesis, etc.);
- tumor formations on the spine and spinal cord with compression of nearby vessels, metastasis, hemorrhages;
- diseases of the hematopoietic system with impaired hemostasis (hemophilia, coagulopathy, etc.).
Often the cause of a spinal stroke consists of various factors, the most common in importance. As a rule, this applies to obesity, arterial hypertension, nicotine addiction, etc.
Treatment of spinal cord stroke
The choice of treatment tactics depends on the cause of the disorder and the location of the lesion. The primary task of the doctor is to determine the type of stroke and identify the etiological factor. If an acute circulatory disorder is caused by a neoplasm, a herniated disc, or a vascular aneurysm, the question of urgent surgical intervention is raised.
Conservative therapy for ischemic stroke involves the use of a number of pharmacological drugs - anticoagulants, antiplatelet agents, venotonics, vasoactive drugs, angio- and neuroprotectors, decongestants (diuretics) and NSAIDs. Hemodilution is also indicated - infusion of plasma-substituting solutions, as well as fresh frozen plasma. To improve neuromuscular conduction, B vitamins and cholinesterase inhibitors are prescribed, and muscle relaxants are used to combat muscle hypertonicity.
Additionally, skeletal traction and immobilization of the spinal segment where the focus of ischemia is located can be used.
Treatment of hemorrhagic strokes involves the use of medications that strengthen the vascular walls. In parallel, drugs are prescribed to prevent vasospasm, angioprotectors and neuroprotectors.
For neoplasms and injuries, surgical treatment is indicated. Surgical intervention to remove the hematoma is also used when conservative methods are ineffective.
Symptoms of spinal strokes
A pronounced clinical picture of ischemic spinal stroke develops suddenly, within a few minutes, sometimes hours. During the prodromal period, the following symptoms appear:
- intermittent claudication;
- spinal pain (occasionally);
- signs of radiculitis;
- short-term pelvic disorders;
- paresthesia.
At the initial stage, symptoms appear in increasing order, with the disappearance of pain as the sensory spinal areas are damaged.
When moving to the next stage (due to spinal injuries, physical strain, etc.), hematomyelia develops:
- acute spinal pain of the girdling type;
- cephalgia;
- depression of the central nervous system and other signs of hematorahis.
Symptoms of the disease are characterized by a scattered clinical picture depending on the location of the lesion, the extent and neglect of the process. The patient's condition is complicated by loss of motor functions, without adequate therapy leading to irreversible restrictions on movement with often associated genitourinary infections (with the threat of sepsis and death) and the formation of bedsores.
Help without delay. Beware, spinal stroke!
Numbness of the skin, impaired movement in the leg... One of the diseases in which such manifestations occur is stroke. The connection is firmly established in the mind: if there is a stroke, it means the brain.
However, it can also be spinal, affecting the “main cable” of the body - the spinal cord. We are talking with Irina Vladimirovna Vlasova, a neurologist at the Expert Voronezh Clinic, about this pathology. Spinal stroke is the topic of our interview.
— Irina Vladimirovna, now in many cities of Russia there is a campaign aimed at informing people about the first signs of a stroke. But in addition to cerebral stroke, there is an equally dangerous disease - spinal stroke. Tell me what it is?
This is an acute disorder of spinal circulation, which can develop due to compression, blockage or rupture of the spinal artery. In this case, two scenarios are possible: ischemia or hemorrhage. Based on this, spinal stroke is divided into ischemic and hemorrhagic. The first form is more common.
Read material on the topic: Ischemic and hemorrhagic stroke: what is the difference?
— Is spinal stroke reflected in ICD-10?
Yes, its code is G95.1
— How often does this pathology occur among Russians and who is at risk?
It is relatively rare: in the structure of neurological diseases it accounts for 1-1.5%. The risk of occurrence in women and men is generally the same. Most often, this diagnosis is made in the age range of 30-70 years.
IN THE STRUCTURE OF NEUROLOGICAL DISEASES, SPINAL STROKE IS 1-1.5%
What are the causes of spinal stroke? There are several groups, including:
- pathological changes in the vessels supplying blood to the spinal cord (can be congenital - for example, aneurysms, malformations, underdevelopment, and acquired - for example, atherosclerosis);
Read the material on the topic: Will traditional methods of treatment help in the treatment of atherosclerosis?
- processes leading to compression of blood vessels supplying the spinal cord from the outside (tumors, other space-occupying formations in the chest or abdominal cavity, enlarged lymph nodes, vertebral fragments due to injuries);
- complications that arise during operations on the spine or nearby vessels (in particular, on the aorta).
WHEN SYMPTOMS OF A SPINAL STROKE APPEAR, A PERSON NEEDS URGENT MEDICAL CARE AND EMERGENCY HOSPITALIZATION TO A VASCULAR CENTER. CALL AN AMBULANCE
Most often, this pathology develops due to a combination of several factors.
— What are the symptoms of a spinal stroke?
Signs appear quite quickly (from several minutes to several hours, less often - days). They are quite diverse, which is explained by the location of the lesion and its prevalence.
At the level and below the site of the lesion, disturbances in movement (paresis), sensitivity and functions of the pelvic organs are noted.
Ischemic stroke develops more often against the background of “precursors”. These can be various short-term sensitivity disorders (numbness, tingling, mainly in the lower extremities), transient motor disturbances in the form of paresis.
With a hemorrhagic spinal stroke, severe pain in the spine is noted, with radicular symptoms, as well as the motor and other disorders listed above.
— What should be done if there are signs of a spinal stroke? What is first aid?
If a person experiences any of the above symptoms, he needs urgent medical care and emergency hospitalization at a vascular center. Call an ambulance.
— In order to help a patient with a cerebral stroke, doctors have only four hours. How quickly should a patient with suspected spinal stroke be admitted to hospital?
We are talking about the so-called “therapeutic window”. It is up to 4-6 hours (the sooner the better). The sooner help is provided, the smaller the area and severity of the lesion will be.
After this time, the chances of reversing the changes that occur decrease.
— What is included in the “gold standard” for diagnosing spinal stroke?
A collection of complaints and medical history and a neurological examination are required.
Computed and magnetic resonance imaging, spinal angiography, lumbar puncture and electroneuromyography are used.
You can sign up for an MRI of the spine here
A general and biochemical blood test, coagulogram (study of the characteristics of the blood coagulation system), glucose and lipid levels are performed. Consultations with other specialists are carried out.
— What diseases are differentiated between spinal strokes?
The range of pathologies for differential diagnosis includes acute inflammation of the spinal cord, its tumors and space-occupying formations, epidural abscesses, and syringomyelia.
— How is spinal stroke treated? What are its principles?
Regardless of its type, nonspecific therapy is carried out aimed at reducing edema, maintaining metabolic processes in nerve cells, and preventing complications.
For ischemic spinal stroke, neuroprotective therapy is carried out, anticoagulants and antiplatelet agents are prescribed.
If this is a hemorrhagic spinal stroke, drugs are used to stop the bleeding, and, if indicated, surgery is performed to eliminate its source.
— Irina Vladimirovna, what is the prognosis for patients with spinal stroke? Has modern medicine learned to successfully treat this disease and rehabilitate such patients?
This pathology has a mostly favorable outcome, but sometimes it can result in disability or death. This can be, in particular, in case of malignant tumors, a severe general somatic background (for example, the presence of diabetes), or the addition of an infection (for example, the development of pneumonia).
The outcome is also influenced by factors such as the cause that led to the development of the stroke, the anatomical and physiological characteristics of the “bypass” blood circulation. Early treatment improves the prognosis of the disease.
SPINAL STROKE MOSTLY HAS A FAVORABLE OUTCOME. EARLY TREATMENT IMPROVES THE DISEASE PROGNOSIS
Recovery after a spinal stroke is ensured by rehabilitation measures. Early rehabilitation includes the use of physical therapy, kinesiotherapy and physiotherapy, massage, and ergotherapy.
The success of rehabilitation also depends on the extent of damage to the spinal cord tissue and the timeliness of seeking help (within the “therapeutic window”).
— Our material will be incomplete if we do not talk about disease prevention. How to avoid spinal stroke?
Its prevention lies in timely diagnosis and treatment of vascular pathologies; detection and elimination of malformations, aneurysms; treatment of intervertebral hernias; prevention of spinal column injuries.
Read material on the topic: What are hernias and protrusions of the spine?
It is important to lead an active lifestyle, normalize weight, eat rationally, and get rid of bad habits.
Other materials on topics:
Let's pull and pull! Who can benefit from spinal traction?
What will an MRI of the spinal column show?
For reference:
Vlasova Irina Vladimirovna
Graduate of the Faculty of General Medicine of the Voronezh State Medical Academy in 2007.
From 2007 to 2009 she completed clinical residency in the specialty “Neurology”.
Currently holds the position of neurologist at Clinic Expert Voronezh. Receives at the address: st. Pushkinskaya, 11.
Diagnostics
When diagnosing spinal strokes, it is important to determine the stage of development of the pathological process and the mechanism of its triggering. The list of instrumental examinations includes:
- computed tomography of the spinal column;
- collection of cerebrospinal fluid (lumbar puncture);
- spinal angiography;
- electroneuromyography of muscle tissue.
The reason against which the disease began to develop is determined together with highly specialized doctors and general practitioners (therapist, hematologist, endocrinologist, etc.). Laboratory diagnostics involves a detailed blood test, coagulogram, etc.
Surgery for hemorrhagic stroke
The second stage of the treatment process is neurosurgical intervention. Its goal is to remove the life-threatening hematoma to improve survival and achieve the best possible satisfactory functional outcome. The sooner the operation is performed, the better prognosis can be expected. However, early surgery, as a rule, involves performing surgical procedures no earlier than 7-12 hours after the stroke. In the ultra-early period, it can lead to repeated bleeding.
When it is wiser to begin removing blood clots is decided by highly competent neurosurgeons. It was noted that operations performed even 2-3 weeks (inclusive) after the GI procedure can also lead to a positive effect. So the question of when to operate on a patient is entirely the responsibility of the doctor. Let us consider the fundamental surgical methods widely used for hemorrhagic strokes.
- Open decompressive craniotomy is indicated for medium and large subcortical, as well as large putamental and cerebellar hemorrhages. It is also addressed in case of pronounced displacement and increasing swelling of the cerebral component, deterioration of the patient’s neurological status. Open surgery is performed under complete general anesthesia using microsurgical optics. Removal of the accumulated clot is carried out through classic trepanation access. Next, an economical encephalotomy is performed, then the pathological component is sucked out with a special device. Dense accumulations are removed with fenestrated tweezers. At the end, the surgical field is thoroughly washed with sodium chloride solution, and thorough hemostasis is performed through coagulation and antihemorrhagic agents.
- The puncture-aspiration procedure is recommended for small hemorrhages of the thalamic, putamental, cerebellar location. The method consists of creating a small hole in the skull, puncturing the hematoma, and then freeing the brain from its liquid mass through aspiration. This technology can be implemented using one of two minimally invasive techniques: based on the principle of stereotactic or neuroendoscopic aspiration. Sometimes it is advisable to combine them with local fibrinolysis. Fibrinolysis involves installing drainage after puncture and aspiration into the hematoma cavity. Fibrinolytics are administered through the drainage over several days to activate the dissolution (liquefaction) of the blood clot and the removal of lysed blood elements.
Unfortunately, the functions of the central nervous system cannot be completely restored after hemorrhagic strokes. But in any case, it would be in the patient’s interests to go to a clinic where international-level doctors work in the diagnosis and surgical treatment of intracerebral lesions. This is the only way to ensure adequate and safe surgical support. Consequently, minimizing complications leads to more productive results in restoring quality of life.
We emphasize that the ideal execution of the operation in the right time increases the survival rate by 2-4 times. Proper postoperative care reduces the likelihood of relapse. It must be warned that a repeated stroke with hemorrhage in 99.99% of patients leads to death.
As a recommendation, we consider it important to say that the Czech Republic shows good results in the level of development of the field of brain neurosurgery in Europe. Czech medical centers are famous for their impeccable reputation and excellent rates of successful recovery of even the most difficult patients. And that’s not all: the Czech Republic has the lowest prices for neurosurgical care and one of the best postoperative rehabilitation. The choice of a medical institution for undergoing surgery, of course, remains with the patient and his relatives.
Medical therapy
Treatment is aimed at preventing critical conditions of the patient, stopping the growth of the area of spinal lesions, and saving neurons.
A set of treatment procedures is prescribed according to the type of spinal stroke:
- nonspecific - decongestant, maintaining tissue condition;
- specific - treatment of ischemia and hemorrhage.
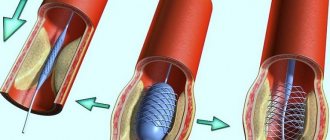
For ruptures of vascular walls, blood clots, tumors, surgical treatment methods are used:
- vascular reconstruction (stenting, thromboembolectomy, elimination of defects);
- antiangioplasia (removal of malformations, resection of aneurysms, etc.);
- removal of compression (disectomy of hernias, tumors, rigid vertebral fixation).
At the recovery stage for spinal stroke, the possibilities of physiotherapeutic treatment, massage, and physical therapy are widely used.
Medical care in hospital
All patients receive intensive therapeutic care at an early stage in a neuro intensive care hospital. Initial treatment measures are aimed at:
- normalization of microcirculation, hemorheological disorders;
- relief of cerebral edema, treatment of obstructive hydrocephalus;
- correction of blood pressure, body temperature;
- functional regulation of the cardiovascular system;
- maintaining water and electrolyte balance;
- prevention of possible seizures;
- prevention of extracranial consequences of inflammatory and trophic nature (pneumonia, embolism, pulmonary edema, pyelonephritis, cachexia, DIC syndrome, endocarditis, bedsores, muscle atrophy, etc.);
- providing respiratory support (if the patient needs it);
- elimination of intracranial hypertension in HI with dislocation.
Forecast and preventive measures
The consequences of a spinal stroke are not as life-threatening as a cerebral stroke. An unfavorable prognosis occurs in extremely severe general somatic conditions, malignant tumors, and secondary infections.
Competent therapy triggers symptomatic regression, but with extensive damage, aggravated by other pathologies, and delayed therapy, recovery cannot be complete, the patient faces complete disability.
The basis of disease prevention is the timely detection, treatment and prevention of any vascular and vertebral pathologies. Giving up bad habits, physical activity, weight and nutrition control minimize the occurrence of predisposition factors to the disease.
If you notice any warning symptoms, call us at the numbers listed on the website. Our specialists will help make an accurate diagnosis and prevent the disease. At the Consulting and Diagnostic Center we use only modern diagnostic and treatment methods. Click the "SIGN UP" button and come see us.
Consequences
Complications of strokes include infections of the genitourinary system due to urinary and fecal incontinence, as well as pneumonia and bedsores associated with prolonged limitation of mobility. To prevent them, it is necessary to provide the patient with good care.
If the patient is unable to urinate on his own, a catheter is indicated, and in case of incontinence, it is advisable to use urinals. Special devices - rubber circles or rings - help to avoid bedsores. Careful hygiene of the external genitalia is an important measure to prevent ascending urogenital infections. Breathing exercises, which must be performed hourly for 5-10 minutes while the patient is on bed rest, help prevent pneumonia.
With a small area of the lesion and timely adequate treatment (surgical or medicinal), complete clinical recovery is possible. In some cases, consequences such as sensory disturbances, paresis of the limbs and dysfunction of the pelvic organs develop.
Sensory disorders
A spinal cord stroke causes sensory disturbances. With extensive damage, sensitivity in the segment innervated by the damaged area disappears completely. Possible dysfunction of the pelvic organs, involuntary defecation and urination, decrease or disappearance of potency.
Symptoms of spinal stroke depend on the level of nerve tissue damage
If the pathological process affects half of the transverse section of the spinal cord, Brown-Séquard syndrome develops. On one half of the body, located on the same side as the damaged area. In this case, disturbances in the motor sphere and loss of deep sensitivity are observed, that is, the patient loses the ability to feel the movements of his muscles and does not feel pressure on the body. On the opposite side of the body, the so-called superficial (pain, temperature) sensitivity disappears.
If the artery supplying the anterior side of the spinal cord is damaged, the patient loses sensitivity to pain and also develops constipation. If the artery supplying blood to the back of the spinal cord is damaged, muscle spasms and loss of vibration sensation in the legs may occur. This type of spinal cord stroke is quite rare.
Rehabilitation
After completing treatment for a spinal stroke, the patient requires long-term work with a rehabilitation physician. Rehabilitation is aimed at rapid restoration of impaired neurological functions.
In many ways, the prognosis after a spinal cord stroke depends on the rehabilitation program
The following rehabilitation measures are used:
- physical therapy classes;
- massage;
- physiotherapeutic procedures (electrical stimulation of damaged nerve fibers, acupuncture, reflexology).
Movement disorders
When hemorrhaging into the spinal cord, acute (dagger) pain appears in the spine, which can radiate to areas adjacent to the damaged area of the spinal cord. If the process affects the membranes of the spinal cord and brain, headaches, dizziness and loss of consciousness are possible.
In general, the symptoms of spinal stroke are quite diverse. Manifestations depend on the location of the damage and its extent. Movement disorders are characterized by paresis (weakness) of the muscles at the level of the affected area of the spinal cord and below it. With prolonged paresis, irreversible atrophic changes develop in the muscles.