Stage 1a uteroplacental blood flow disorder is a phenomenon in which the fetus receives insufficient oxygen. If this problem is ignored, the child may experience hypoxia, which leads to disruption of the development of internal organs or death of part of the cerebral cortex. To prevent the formation of negative consequences, it is necessary to start treatment on time.
Normal uteroplacental blood flow
Pregnant women often do not even suspect the existence of Doppler ultrasound
. This study helps determine the volume and strength of blood flow using ultrasound radiation. Usually Doppler testing is carried out in the third semester of pregnancy, but in some cases this study can be carried out earlier.
With the help of Dopplemetry, it is possible to identify any pathologies of blood vessels in the uterus or placenta in the early stages. It also helps to identify abnormalities in the fetal carotid and cerebral arteries. Based on the results, the doctor will be able to determine whether the baby is experiencing a lack of blood flow or not.
If a woman’s uteroplacental blood flow is disrupted, her fetus is in constant deficiency of oxygen and nutrients.
Doppler ultrasound examination
, which helps determine blood flow in the pelvis. It can also be used to determine the resistance index, compliance with which is necessary for the normal functioning of the fetus. Having received accurate data from such an analysis, doctors use special mathematical formulas to calculate the speed and volume of blood flow. Based on the results, it can be concluded whether the woman suffers from BMD violations or not.
Squamous epithelium is the cells that form the mucous layer of the internal genital organs. They can be found in the vagina, urethra and cervix. The main function of the epithelium is the secretion of a special type of cells that prevent infection and protect against injury. Read more in the article: “epithelium: the norm in women.”
Types and causes of placental insufficiency
Doctors distinguish between acute and chronic placental insufficiency:
Acute placental insufficiency
This is a condition that requires emergency medical intervention. It is characterized by a rapid deterioration of placental blood flow. Acute placental insufficiency occurs mainly as a result of placental abruption or death of individual areas of placental tissue, for example, due to the formation of blood clots in blood vessels. The cause of detachment may be abdominal trauma or antiphospholipid syndrome.
Phospholipids are complex fats that are part of the membranes of all cells in the body. In some cases, the body's immune system produces large amounts of antibodies to some of its own phospholipids and proteins that bind these lipids. They are called antiphospholipid antibodies and when interacting with the cells of the body, they cause cell damage and activation of the blood coagulation system, which leads to blood clots.
Antiphospholipid syndrome is the most common cause of thrombotic complications during pregnancy, including placental abruption and acute placental insufficiency. Placental abruption can also be caused by severe gestosis, a dangerous complication of the second half of pregnancy, manifested by edema, increased pressure and the appearance of protein in the urine.
Acute placental insufficiency develops when more than 2/3 of the surface of the placenta is detached.
If acute placental insufficiency develops, it is necessary to perform a cesarean section as quickly as possible to save the life of the baby and mother.
Chronic placental insufficiency
Chronic placental insufficiency occurs much more often in pregnant women. In this case, the formation and maturation of the placenta is disrupted, uteroplacental and fetal-placental blood flows are reduced, gas exchange and metabolism in the placenta is limited, and the synthesis of placental hormones is reduced. All these changes determine the insufficient supply of oxygen and nutrients to the baby and cause retarded growth and development of the fetus.
The causes of placental insufficiency most often are previous abortions, especially surgical abortion during the first pregnancy, smoking, while the number and strength of cigarettes smoked do not matter, since tobacco smoke, not nicotine, has a negative effect on the formation of defective blood vessels of the placenta.
The risk group for the development of placental insufficiency also includes women with chronic diseases, such as arterial hypertension, iron deficiency anemia, pyelonephritis, diabetes mellitus, and thyroid diseases. In recent years, there has been a significant increase in placental insufficiency caused by bacteria, viruses, and fungi. The reason for this may be either an acute infection suffered by the expectant mother during pregnancy or the activation of a chronic infectious process in the body of a pregnant woman.
Uterine pathology plays an important role in the formation of chronic placental insufficiency: endometriosis, uterine malformations (saddle-shaped, bicornuate). Doctors also consider uterine fibroids to be a risk factor. Of course, a number of medications have an adverse effect on the formation of the placenta and fetal development. Currently, a list of drugs that are not approved for use during pregnancy has been determined.
Also of great importance in the development of placental insufficiency is thrombophilia - an increased tendency of the body to form blood clots - thrombi in the vessels.
In some cases, placental insufficiency may be due to the presence of chromosomal abnormalities in the fetus, in particular with Down syndrome (the presence of an additional 21st chromosome in the fetus) or Edwards syndrome (an additional 18th chromosome in the fetus), a dysfunction of the placenta is diagnosed already in the early stages of pregnancy.
It should be noted that among the pregnancy complications that most often lead to the development of chronic placental insufficiency, a significant factor is preeclampsia (or late gestosis) - these are complications of the second half of pregnancy, manifested by edema, increased pressure and the appearance of protein in the urine. Regardless of the factors contributing to the development of placental insufficiency, it is based on circulatory disorders in the uteroplacental complex, leading to disruption of all functions of the placenta. Consequently, symptoms of chronic placental insufficiency will be caused by a lack of oxygen and nutrients to the fetus.
This is, first of all, intrauterine growth retardation - a lag in the size of the fetus and a slowdown in its growth rate. There are often changes in fetal motor activity. At first there may be some increase in movements, and then a decrease. Violation of the protective function of the placenta leads to intrauterine infection of the fetus under the influence of pathogenic (disease-causing) microorganisms penetrating the placenta. The fetus, whose development occurs under conditions of placental insufficiency, is at a much greater risk of trauma during childbirth; they have impaired adaptation to extrauterine life and increased morbidity in the first year of life.
Based on the time of occurrence, doctors divide placental insufficiency into early and late.
Early (or primary) placental insufficiency
Develops before 16 weeks of pregnancy. It occurs already at the stage of placenta formation and is associated with diseases of a pregnant woman that existed before pregnancy, for example, pathology of the uterus, chronic arterial hypertension, and endocrinological diseases. In this case, the formation of defective vessels in the placenta occurs.
Late (or secondary) placental insufficiency
Occurs after 16 weeks of pregnancy and is most often associated with diseases that arose during pregnancy. Most often, these are iron deficiency anemia (that is, a decrease in the concentration of hemoglobin and iron in the blood), gestational diabetes mellitus (that is, a violation of the body's absorption of glucose that occurs during pregnancy), and previous viral and bacterial infections.
It is important to divide placental insufficiency into compensated and decompensated forms.
Compensated placental insufficiency
It develops, for example, when there is a threat of miscarriage and mild forms of late gestosis, if these complications can be successfully corrected with medication.
Decompensated placental insufficiency
Causes development of delayed fetal development, chronic intrauterine hypoxia, up to fetal death.
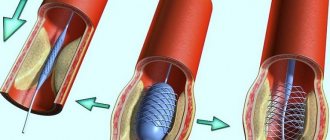
Structure of the uteroplacental blood flow
Mother and child are connected not only by the placenta, but also by a complex system of blood vessels. Therefore, all joint blood circulation is usually divided into levels that cannot exist in isolation, but work only in combination. The central part of the system is the placenta. It ensures the absorption of products from the maternal blood through villi that have grown deep into the wall of the uterus.
At the same time, the blood of mother and child does not mix.
Several rows of special cells form a hematoplacental barrier, which is a serious obstacle to substances unnecessary for the fetus. Through it, the waste blood returns to the mother's venous system. The second part of the blood flow consists of the branches of the uterine arteries. If before pregnancy in the female body they are in a collapsed state and are called spiral, then from the period of 1 month they lose the muscle layer that can cause spasm.
And by four months, the arteries transform into full-fledged trunks, filled with blood and heading to the placenta area. It is this mechanism, useful for feeding the fetus, that can turn out to be fatal during uterine bleeding: the walls of the vessels can no longer contract. The vessels in the umbilical cord form the third pathway of blood flow. There are 2 arteries and a vein here. They connect the baby with the placenta and form the fetal-placental circle. Reduced blood flow at this level causes the most severe damage to the fetus.
Female breast tumors are a group of life-threatening diseases. If the formation is oncological in nature, without treatment it metastasizes and leads to death. Read more in the article: “symptoms of a breast tumor.”
How is BMD impairment determined during pregnancy?
The Doppler ultrasound method allows for an objective assessment of blood flow indicators in the “uterus-placenta-fetus” chain. A woman is invited to the study three times during her pregnancy.
During the study:
- measure blood flow by determining the speed of movement of blood cells;
- check the direction of blood flow in arteries and veins;
- changes are recorded before obvious symptoms of pathology appear.
Taking into account normal indicators, the doctor identifies the degree of impairment of MPC. Failure of a complex system can occur in the vessels:
- umbilical cord;
- uterus;
- fetus
In some cases, Doppler ultrasound (a type of Doppler sonography) is used to diagnose MPK during pregnancy. Indications for such a study are:
- signs of acute lack of oxygen in the baby;
- genetic diseases in any of the blood relatives of the expectant mother;
- polyhydramnios or oligohydramnios;
- symptoms of premature aging of the placenta or disruption of the placental barrier;
- the presence of reliable information that the fetus is lagging behind in development, has a tendency or has already acquired certain congenital defects.
Doppler testing helps identify the following problems:
- thinning of the walls of the placenta;
- excessive growth of the placenta;
- intrauterine infection of the fetus;
Clinical picture of the disorder
The symptoms of blood flow disorders depend on how pronounced the changes in the vascular bed are. On the part of the pregnant woman herself, there may be no signs of pathology at all or only gestosis. Often, hemodynamic disorders are detected due to the fact that a woman is undergoing examination due to the threat of miscarriage or premature onset of labor, which manifests itself:
- pain in the abdomen and groin area.
- the appearance of bloody-mucous discharge from the genital opening.
- Often in pregnant women with a similar pathology, colpitis appears or worsens during gestation.
Advertising:
On the part of the fetus, the symptoms of hemodynamic disorders are more pronounced. With the development of hypoxia, the frequency of the child’s movements decreases. During examinations at an appointment with an obstetrician-gynecologist, a specialist may pay attention to an increase or decrease in the child’s heart rate. The doctor may also note that the volume of the abdomen and the height of the uterine fundus are not correlated with gestational age.
Classification
These deviations have varying degrees of damage and development. Mainly the following are distinguished.
| Failure of blood flow 1a degree | Accompanied by the presence of abnormalities in the uterus and placental arrangement of blood vessels. The fruit is not affected. At this stage, the pathology is not significant. Therefore, it can be easily eliminated. After timely diagnosis, you should definitely undergo a routine examination |
| Violation 1b degree | The child’s condition with this pathology remains satisfied. But the risk of danger increases |
| Development of stages 2 and 3 of the disease | Severe abnormalities in all systems. Serious complications can lead to fetal death |
Causes of blood flow disorders in the pelvis
A huge number of factors can provoke circulatory failure in the pelvis. Separately, there are those that provoke disturbances during the formation of the placenta, and those that occur at a later date. Thus, it is customary to distinguish between primary and secondary forms of pathology. If the problem is ignored for a long time, the woman’s risk of miscarriage increases, and the fetus cannot develop its endocrine glands, metabolism, and immune functions normally. This phenomenon can be caused by:
- serious infectious diseases;
- genetic abnormalities of the fetus;
- tumors and other diseases of the uterus;
- sudden changes in hormonal levels;
- late toxicosis;
- diabetes;
- heart problems;
- thrombosis and atherosclerosis;
- consequences of surgery on the uterus;
- anomalies of the structure of the uterus on the left and right;
- diseases of the endocrine glands.
Advertising:
The risk of developing uteroplacental insufficiency increases even if one of the above factors is present. If there are several reasons, a woman needs to visit the treating specialist more often in order to identify deviations in time. Your doctor will send you for periodic screenings and other tests.
MPC during pregnancy: what is it?
The growth and development of a child in the womb is possible thanks to the utero-placental-fetal blood flow (UPF). This system is considered as an important factor necessary for the normal course of gestation.
Violation of uterine hemodynamics provokes the development of such a dangerous condition for the baby as placental insufficiency. If this deviation is present, there is a high probability of abruption, miscarriage or fetal death. To find out the cause of the violation of MPC, the expectant mother is sent for screening at different stages of pregnancy.
Symptoms of uteroplacental disorder
Like any other pathology, BMD disorder has a number of features in its manifestation. If you know exactly the signs of this deviation, a woman will be able to identify the disease in the early stages, which will allow her to consult a doctor in time. The main danger of stage 1a uteroplacental blood flow disturbance is that the fetus experiences oxygen starvation. Such hypoxia interferes with the normal development of its internal organs and can cause miscarriage or fading of pregnancy. Pathology can be recognized by the following changes:
- the child's heart rate increases significantly;
- the fetus periodically becomes either active or lethargic;
- the volume of the abdomen does not correspond to normal readings - it is ahead of them.
Signs of degree 1a BMD impairment usually appear in the decompensated form. However, in some cases there are no manifestations of this pathology at all. It is possible to find out about its presence only after the next examination.
Diagnosis of placental insufficiency
It is almost impossible to treat already developed placental insufficiency, so doctors are actively seeking to identify pregnant women at risk of developing placental dysfunction. If placental insufficiency is detected in the 3rd trimester of pregnancy, unfortunately, there is no effective treatment. Therefore, all methods of identifying in the early stages of pregnancy those women whose placenta formation has undergone disturbances are being very actively used.
First of all, when registering for pregnancy, the most significant risk factors are identified - smoking, previous abortions, family history (low birth weight, tendency to thrombosis), the presence of chronic heart disease, vascular disease, diabetes mellitus.
Preventive measures against the development of placental insufficiency are especially relevant and necessary until 16-17 weeks of pregnancy, when the formation of placental structures occurs.
Prenatal screening, which is carried out at 11-14 weeks of pregnancy, provides significant assistance in assessing the risk of developing placental insufficiency. It is carried out to identify Down syndrome, Edwards syndrome and other chromosomal diseases in the fetus. Currently, the most urgent thing is to conduct comprehensive early screening of pregnant women to predict the risk of developing placental insufficiency, preeclampsia and intrauterine growth retardation. Since this type of diagnostics is one of the most modern and advanced, unfortunately, it is not yet included in the list of services provided in the antenatal clinic as part of compulsory medical insurance, but is available to everyone at prenatal diagnostic centers.
Determination of proteins produced by the placenta
First of all, the PAPP-A protein is determined; it is also a marker of fetal chromosomal abnormalities. A decrease in the concentration of PAPP-A in the blood at 11-14 weeks of pregnancy occurs in pregnant women who have a high risk of placental insufficiency and fetal growth retardation.
The second placental hormone that helps in assessing the risk of placental insufficiency is PIGF (placental growth factor). Its concentration in the blood decreases long before the first manifestations of placental insufficiency. Its definition is not used as widely as PAPP-A, but nevertheless, many laboratories have already included this protein in prenatal screening of the 1st trimester. Measuring blood flow in the vessels of the uterus is extremely important when conducting 1st trimester screening. It has been unequivocally proven that the narrowing of the vessels of the uterus, determined during the study, indicates the inferiority of the formation of the placenta, which will worsen with increasing gestational age and will lead to a decrease in the baby’s nutrition and oxygen supply, that is, to the development of placental insufficiency and delayed fetal development. With normal sizes of the uterine vessels at 11-14 weeks of pregnancy, the risk of severe placental insufficiency is negligible.
The next mandatory screening ultrasound examination is carried out at 20-21 weeks of pregnancy. In this case, it is necessary to take measurements of the fetus to assess whether there is growth retardation. Indeed, with oxygen starvation, the growth rate of the fetus slows down and its size begins to lag behind the norm for each stage of pregnancy. In addition, the doctor must evaluate the condition and maturity of the placenta. During ultrasound, Doppler measurements of the uterine vessels are also performed to identify early changes that precede the clinical manifestations of placental insufficiency.
In patients belonging to the high-risk group, in addition to ultrasound and Doppler measurements, daily monitoring of blood pressure fluctuations is also carried out, determination of the amount of protein in a urine test collected per day, and evaluation of blood coagulation system parameters.
The third ultrasound is performed for all expectant mothers at 30–34 weeks of pregnancy. The doctor measures the circumference of the baby's head and abdomen, the length of the bones of his arms and legs, and calculates the estimated weight of the fetus. These measurements allow the doctor to make sure that the baby is developing normally. Also important is the structure of the placenta, the presence of signs of aging in it, as a result of which it usually ceases to fully supply the baby with blood, which means that he ceases to have enough oxygen and nutrients and the child’s development is disrupted. During an ultrasound, the amount and type of amniotic fluid is assessed, which can also change with intrauterine fetal suffering.
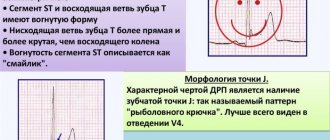
Doppler
Doppler testing of the vessels of the placenta and umbilical cord (a method for studying the speed of blood flow in these vessels) also allows you to assess the baby’s well-being. The doctor examines the blood flow in the arteries of the uterus, umbilical cord, heart and brain of the child. This study allows you to determine whether the placenta is working well, whether there are signs of a lack of oxygen in the baby, or the development of gestosis in the mother. When the speed of blood flow in any vessel decreases, we can talk about fetal nutritional disorders of varying degrees of severity.
A timely examination allows us to identify the initial stages of blood supply deficiency. In such cases, treatment can prevent serious complications, such as hypoxia and intrauterine growth retardation. Dopperometry is carried out at 20–21 weeks and at 30–32 weeks of pregnancy; if there are changes, monitoring is carried out at least every two weeks.
Cardiotocography
This is an important method for assessing the condition of the fetus. CTG is performed during pregnancy of 33 weeks or more, since only at this stage of the baby’s intrauterine development is full regulation of the activity of the fetal cardiovascular system established by the centers of the spinal cord and brain. The fetal heartbeat is recorded for 20–40 minutes, and if necessary, the study can be extended to 1.5 hours.
The device detects and records the baby's heart rate. The obstetrician-gynecologist evaluates the heartbeat recording curve, episodes of decrease and sharp increase in the fetal heart rate and, based on these data, makes a conclusion about how comfortable the baby feels in the mother’s stomach. For example, when the concentration of oxygen in the blood of the fetus decreases, its supply to the cells of the nervous system also decreases, which in turn affects the heart rate. In the normal course of pregnancy, CTG is performed after 33 weeks once every 10–14 days, sometimes more often. Some clinics currently offer the service of continuous CTG monitoring, which becomes relevant if there are signs of placental insufficiency. A pregnant woman is given a monitor that records changes in the baby’s cardiac activity and this data is transmitted via the Internet to the attending physician.
Detection of blood flow disturbances
Determining uteroplacental circulatory disorders is quite simple. To do this, the doctor uses modern diagnostic methods that make it possible to identify pathology without harm to the child. Before the specialist sends you for examination, he will collect a detailed medical history and assess the degree of manifestation of the BMD violation. In general, diagnosing this problem looks like this:
Advertising:
- physical examination of the pregnant woman;
- ultrasound examination of the pelvis and abdominal cavity;
- ultrasound fetometry;
- Dopplerometry;
- cardiotocography;
- assessment of fetal activity;
- General, biochemical and hormonal blood tests.
An experienced specialist can easily identify this pathology based on the patient’s complaints alone. To do this, he needs to collect information about her obstetric past.
, assess the general condition of the body. Based on the results of functional tests, the doctor will be able to identify the most optimal and effective treatment that will help quickly relieve the fetus from oxygen starvation.
Treatment of uterine blood flow disorders
- Almost all degrees of blood flow disorders require mandatory treatment. The question is what degree of blood flow disturbances is detected, and whether it is accompanied by fetal growth retardation. Basic methods of treating fetal blood flow disorders:
- Normalization of the lifestyle and nutrition of a pregnant woman. It is important to walk a lot in the fresh air, sleep at least 8 hours at night and try to rest for at least an hour during the day, avoid sitting for long periods in an uncomfortable position, move a lot, eat normally and nutritiously.
- Blood pressure control is one of the most important parameters determining uterine blood flow. If you have arterial hypertension, you must constantly take medications prescribed by your doctor and independently monitor your blood pressure readings.
- Treatment of intrauterine infection with antiviral drugs and antibiotics.
- The use of antispasmodics - No-shpy, Drotaverine, Papaverine. These drugs relax the wall of the uterus and spiral arteries, increasing blood flow.
- Taking magnesium supplements - magnesium has a relaxing effect on the uterine wall and a powerful protective effect on the central nervous system of the fetus. The last factor is important in the development of hypoxia.
- The use of vascular drugs is a large group of disaggregants, angioprotectors and drugs that improve microcirculation and tissue trophism. The most common drugs in obstetrics are Pentoxifylline, Dipyridamole, Actovegin and their derivatives.
- In case of Rh conflict, plasmapheresis is prescribed - purification of the mother's blood using a special device to reduce the amount of antibodies damaging the fetal red blood cells.
Advertising:
How to treat BMD disorder during pregnancy
Conservative treatment methods are effective in case of circulatory disorders of the first degree (1a and 1b). The second degree of violation is borderline, and the third is considered critical, so the expectant mother will have to undergo an emergency birth.
In order for the treatment to work, it is necessary to take into account all the pathological processes that together caused circulatory problems between the mother and the fetus:
- if the microcirculation disorder is insignificant, the doctor opts for Chofitol; for a more serious disorder, Actovegin or Pentoxifylline will be suitable;
- if the examination shows that the expectant mother is prone to the formation of blood clots, and the rheological properties of her blood are impaired, the patient is prescribed Curantil or Trental. These drugs improve vascular blood flow;
- if the condition of a pregnant woman is complicated by a decrease in blood pressure, medications such as Venofundin, Volecam, Voluven, Stabizol are used;
- No-shpa and Eufillin injection solutions help to quickly eliminate vascular spasm;
- Dangerous uterine tone is relieved with injections of Magnesium Sulfate, as well as Magne B6. This measure has a positive effect on the BMD of the pregnant woman;
- complex treatment of blood flow disorders during pregnancy can never be done without biologically active substances, which by their nature are antioxidants - these are vitamins C and E.
The expectant mother is always offered to undergo treatment in an inpatient medical facility. This will help the pregnant woman to remain in bed and to remain under strict medical supervision during treatment.
If conservative therapy bears fruit and the expectant mother’s condition returns to normal, the child has every chance of fully developing and being born on time. If there is no visible effect from drug treatment, doctors prepare the pregnant woman for early birth using a cesarean section.
How to help the body?
Treatment of uteroplacental disorders should be started in a timely manner to avoid negative consequences. If a woman is at increased risk of developing this pathology, then she should visit the gynecologist more often. The treatment method depends on the reasons that provoked this phenomenon. In most cases, medications that relieve uterine tone or improve blood clotting help improve blood circulation.
When the first signs of changes in blood circulation in the pelvis appear, a pregnant woman should immediately consult a doctor.
If a woman is diagnosed with a violation of the fetal-placental blood flow, she is immediately hospitalized at 36 weeks
. She will have to stay in the hospital until she gives birth. It should be noted that labor activity with such pathology requires special care. If a woman did not take any medications during pregnancy, she is prescribed a cesarean section, which means that a natural birth is impossible.
Prevention of uteroplacental pathology
To give birth to a healthy baby, a pregnant woman needs to be more careful and listen to her body. Try to watch your diet: it should be nutritious, rich and healthy. You can also take vitamin complexes or Ginipral, which will eliminate the deficiency of any element.
Advertising:
Also try to drink as much clean water as possible - at least 2 liters per day. Do not forget to control your body weight - during pregnancy it should not increase by more than 10 kg.
Doctor's recommendations will help you get rid of BMD level 1a violation
. Do not forget to regularly visit your treating specialist to monitor the development of this pathology. If normal blood flow is disrupted, the woman may be placed on preservation. Remember that you should not prescribe treatment for yourself based on the advice of friends or information from the Internet. This will lead to the development of serious complications.
Prevention of pathology
In order to avoid problems with blood flow, it is important for a woman to eat well. The diet should be enriched with vitamins to the maximum, contain the necessary microelements, as well as the right amount of proteins, fats and carbohydrates. It is important to drink enough fluids if there is no swelling.
Women from the most vulnerable groups - those under 18 years of age and over 35 years of age, those with bad habits, those suffering from chronic diseases - should take the necessary medications prophylactically to prevent problems with blood flow.
A woman should monitor her body weight. A total weight gain of more than 10 kilograms by the end of pregnancy is considered a risk factor.
In conclusion, it should be noted that placental insufficiency is a serious problem, sometimes fraught with fatal complications for both the mother and the unborn child. Therefore, it is important already at the planning stage to analyze your lifestyle and eliminate possible risks, and during pregnancy to monitor your condition and not neglect medical recommendations.
Signs of BMD impairment during pregnancy
If the body independently compensates for imperfect blood flow, the woman will not feel anything bad, and deviations will be discovered only as a result of a thorough examination.
In acute circulatory disorders, as well as chronic decompensation, obvious signs of the disorder appear:
- fetal movements suddenly become more active or disappear completely (we remind you that at week 28 the baby’s normal movements are 10 episodes per day). If such “strangeness” is detected, you need to consult a doctor right away;
- too slow growth of the abdomen in circumference. It is detected provided that the expectant mother responsibly attends all scheduled examinations in the residential complex. This symptom occurs due to a deficiency of amniotic fluid;
- gestosis;
- high blood pressure;
- excessive weight gain;
- severe swelling in the lower legs;
- the presence of protein in the urine;
- vaginal bleeding. This is the most dangerous sign indicating premature detachment of the child's place. The expectant mother needs immediate hospitalization.