- Home /
- Branches /
- Cardiology /
- Wolff–Parkinson–White syndrome (WSW syndrome)
10/13/2021 The article was checked by a cardiologist-arthymologist, Ph.D. Zhelyakov E.G. , is for general informational purposes only and does not replace specialist advice. For recommendations on diagnosis and treatment, consultation with a doctor is necessary.
At the Yauza Clinical Hospital, experienced cardiologists quickly and accurately diagnose SVC syndrome (ECG, bicycle ergometry, 24-hour ECG monitoring, ECHO-CG and stress ECHO-CG) using expert-class equipment, and, if necessary, carry out minimally invasive cardiac surgical treatment of SVC syndrome. Catheter RFA with precise identification and coagulation of the pathological focus during surgery eliminates the problem forever. The solution to the issue of surgical treatment is radiofrequency ablation, and the operation itself is carried out under the guidance of the leading Russian cardiac surgeon-arrhythmologist Prof. A.V. Ardasheva.
Make an appointment with a cardiologist
Causes of the disease
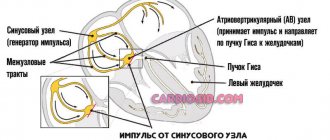
Normally, additional muscle tracts exist in all embryos at an early stage of development.
Then they shrink and disappear. In case of violations, the fibers are preserved. This leads to premature excitation of the ventricles. The pathology is congenital. Despite this, it can appear for the first time at any age. In 30% of cases, the pathology is combined with:
- congenital heart defects;
- hereditary hypertrophic cardiomyopathy;
- connective tissue dysplasia.
What happens with short PQ syndrome?
{banner_banstat0}
The PQ interval is a purely electrocardiographic criterion that allows one to evaluate the transmission time of an electrical impulse from the sinus node in the atrium to the contractile fibers located in the ventricles. In other words, it reflects the operation of the atrioventricular junction, a kind of “switch” that redirects electrical excitation from the atria to the ventricles. Normally, it is no less than 0.11 seconds and no more than 0.2 seconds:
example of shortening PQ to 0.03 s
- An increase in the interval beyond the specified time indicates a slowdown in conduction through the atrioventricular node,
- Shortening means that the excitation is carried out too quickly. In fact, there is more frequent impulse of the ventricles, with the so-called “reset” of excitation.
The shortening of this interval is due to the presence of additional conduction bundles in the conduction system of the heart.
It is through them that additional pulses are reset. Therefore, at certain moments the ventricles receive double impulses - physiological in a normal rhythm (60-80 per minute), and pathological, through bundles.
There may be several pathological bundles, and all of them are named after the names of the authors who first discovered them. Thus, the Kent and Maheim bundles are characteristic of the SVC syndrome, and the James bundles are characteristic of the CLC syndrome. In the first case, the pathological discharge of impulses goes from the atria directly to the ventricles, in the second, the James bundle passes through the atrioventricular node, that is, the node is stimulated first, and then the ventricles. Due to the “throughput” capacity of the AV node, part of the impulses conducted to the ventricles returns through the same bundle to the atria, therefore such patients have a high risk of developing paroxysmal supraventricular tachycardia.
main types of pathological pathways of additional conduction through the heart
Types of premature excitation of the ventricles
The World Health Organization distinguishes:
- The WPW phenomenon. This pathology is characterized by electrocardiographic signs of impulse conduction through additional channels without manifestations of tachycardia.
- WPW syndrome. This pathology is characterized by a combination of preexcitation and tachycardia.
There are several anatomical variants of the condition:
- With extra muscle fibers. They can go through the fibrous junction, left or right junction, from the right or left atrial appendage.
- With specialized muscle fibers that originate from vestigial tissue.
There are also several forms of pathology:
- Manifesting. This form of the disease is characterized by sinus rhythm, the presence of a delta wave and episodes of tachycardia.
- Intermittent. This form of pathology is characterized by sinus rhythm, tachycardia and transient preexcitation.
- Hidden. This form of the disease is characterized by the absence of electrocardiographic signs and episodes of tachycardia.
Why does short PQ syndrome occur?
{banner_banstat2}
As already indicated, the anatomical substrate of this syndrome in adults is a congenital feature, since additional conduction bundles are formed in the prenatal period
. People with such bundles differ from ordinary people only in that they have an additional tiny “thread” in the heart, which takes an active part in conducting the impulse. But how the heart behaves with this beam will be discovered as the person grows and matures. For example, in children, CLC syndrome may begin to manifest itself both in infancy and adolescence, that is, during the rapid growth of the body. Or it may not manifest itself at all, remaining only an electrocardiographic phenomenon throughout adult life until old age.
No one can name the reason why the syndrome begins to manifest itself as paroxysmal tachycardia. However, it is known that in patients with organic pathology of the myocardium (myocarditis, heart attack, hypertrophic cardiomyopathy, heart disease, etc.) attacks of tachycardia occur much more often and clinically occur with a more pronounced clinical picture and with a severe general condition of the patient.
But the provoking factors that can cause paroxysm can be listed:
- Physical activity that is significantly or not significantly greater than the patient’s usual physical activity,
- Psycho-emotional stress, stressful situation,
- Hypertensive crisis,
- Eating large amounts of food at one time, drinking very hot or very cold liquids,
- Visiting a bathhouse, sauna,
- Changes in external temperatures, for example, going out into severe frost from a very hot room,
- Increased intra-abdominal pressure, for example, during severe coughing, sneezing, defecation, pushing during childbirth, lifting heavy objects, etc.
Symptoms of pathology
The course of premature excitation of the ventricles before the first manifestation may be asymptomatic.
Symptoms of the pathology include:
- supraventricular tachycardia;
- atrial flutter and fibrillation;
- specific arrhythmia.
As a rule, attacks occur after physical or emotional stress, as well as alcohol abuse. In some cases, the manifestations of pathology have no apparent cause.
The attack is characterized by:
- feeling of lack of air;
- feeling of a sinking heart;
- dizziness;
- shortness of breath;
- fainting;
- increased blood pressure.
Ventricular fibrillation can cause sudden death.
The main danger of the pathology is heart rhythm disturbances. They significantly reduce the standard of living.
SVC syndrome and pregnancy
SVC syndrome , which does not manifest itself clinically, does not require additional treatment. But during pregnancy, the disease can manifest itself with paroxysmal heart rhythm disturbances. Then a consultation with a cardiologist and selection of effective treatment is necessary.
With very frequent attacks of tachycardia against the background of WPW syndrome, pregnancy is contraindicated. This is explained by the fact that the disease at any period can develop into a life-threatening rhythm disorder. In addition, tachycardia often provokes insufficient blood circulation in organs and tissues, which negatively affects not only the condition of the mother, but also the development of the fetus.
Diagnosis of the syndrome
Diagnosis of pathology is carried out using a number of techniques.
Among them:
- ECG in 12 leads. The study indicators make it possible to detect the disease even if it is asymptomatic. Heart rate (heart rate) in patients can reach 220 and even 360 beats per minute. Tachycardia stops abruptly. On the ECG, pathology is detected due to a shortened PR interval, the manifestation of a delta wave and a widening of the QRS complex.
- Transesophageal electrical stimulation. This technique is more accurate. The study is carried out by placing an electrode on the wall of the esophagus. Thanks to it, the heart contracts at the required frequency. When the indicators reach 100-150 beats per minute, the activity of the Kent beam stops. Thanks to this, the disease is quickly diagnosed.
Also, to diagnose pathology, methods such as:
- Daily ECG monitoring. Such a study is carried out to quickly identify a transient form of pathology.
- Ultrasound of the heart. This study is carried out with Doppler ultrasound. It allows you to identify concomitant pathologies of the cardiovascular system. A specialist can quickly identify defects and other lesions of the heart muscle.
- Endocardial EPI. This technique involves inserting catheters with electrodes into the heart muscle through the venous system. The examination is carried out to detail the location and determine the number of abnormal impulse paths. Using the technique, you can quickly assess the effectiveness of prescribed medications.
A consultation with a cardiologist or cardiac surgeon is also mandatory. Only an experienced doctor is able to correctly assess each symptom, compare the various signs of pathology and draw conclusions about the upcoming therapy. Important! Examinations are also carried out during therapy. This is due to the fact that patients constantly take antiarrhythmic drugs. Their dosages may vary to achieve maximum effect.
Wolff-Parkinson-White syndrome (WPW) is a syndrome with preexcitation of the ventricles of the heart through an additional (abnormal) atrioventricular connection (AVJ) and supraventricular tachyarrhythmia through the re-entry mechanism.
| WPW syndrome. Mechanisms | ||
| Diagnostics | ||
| Treatment |
Definition
Wolff-Parkinson-White syndrome (WPW) is a syndrome with preexcitation of the ventricles of the heart through an additional (abnormal) atrioventricular connection (AVJ) and supraventricular tachyarrhythmia through the re-entry mechanism.
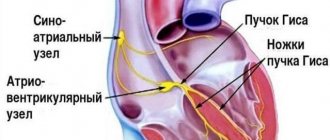
What is DPZHS
In WPW syndrome, the substrate of the arrhythmia is the accessory atrioventricular junction (ASJ). DPVS is an abnormal fast-conducting muscle strip of the myocardium that connects the atrium and ventricle in the area of the atrioventricular groove, bypassing the structures of the normal conduction system of the heart.
The impulse propagates through the ventricular ventricle more quickly than through the normal conduction system of the heart, which leads to pre-excitation (pre-exitation) of the ventricles. With the occurrence of ventricular pre-excitation, a Δ-wave (delta wave) is recorded on the ECG.
ECG for WPW syndrome. Faster propagation of the impulse through the accessory pathway (APP) leads to earlier excitation of part of the ventricles - a Δ wave appears, causing a shortening of the PR interval (PQ) and expansion of the QRS complex.
Prevalence
According to various authors, the prevalence of WPW syndrome in the general population ranges from 0.15 to 0.25%. The ratio between men and women is 3:2.
WPW syndrome occurs in all age groups. In most cases, the clinical manifestation of WPW syndrome occurs at a young age (from 10 to 20 years) and much less often in people of the older age group.
WPW syndrome is not associated with structural heart disease. In some cases, WPW syndrome is combined with congenital heart defects (atrial and ventricular septal defect, tetralogy of Fallot, Ebstein's anomaly).
Forecast
An attack of tachycardia in WPW syndrome is rarely associated with the threat of circulatory arrest.
Atrial fibrillation is life-threatening in patients with WPW syndrome. In this case, with AF, conduction to the ventricles is carried out in a 1:1 ratio with a high frequency (up to 340 per minute), which can lead to the development of ventricular fibrillation (VF). The incidence of sudden death among patients with WPW syndrome varies from 0.15 to 0.39% during a follow-up period of 3 to 10 years.
Mechanisms
Pre-excitation syndromes are based on the participation of additional conducting structures, which are the knee of the macroreentrant atrioventricular tachycardia. In WPW syndrome, the substrate of the pathology is the accessory atrioventricular junction (ADJ), which is usually a muscular strip of the myocardium connecting the atrium and ventricle in the area of the atrioventricular groove.
Accessory atrioventricular junctions (AAVCs) can be classified according to:
1. Location relative to the fibrous rings of the mitral or tricuspid valves.
Anatomical classification of the localization of accessory atrioventricular junctions (ADJ) in WPW syndrome according to F. Cosio, 1999. The right side of the figure shows the schematic location of the tricuspid and mitral valves (view from the ventricles) and their relationship with the area of localization of the ventricular ventricle. Abbreviations: TC - tricuspid valve, MK - mitral valve.
2. Type of conduction: – decremental – increasing slowdown of conduction along an additional pathway in response to an increase in stimulation frequency, – non-decremental.
3. Abilities for antegrade, retrograde conduction, or a combination thereof. DPVCs capable of only retrograde conduction are considered “hidden”, and those DPVAs that function antegrade are “manifesting”; with the occurrence of ventricular pre-excitation, a Δ-wave (delta wave) is recorded on the ECG in standard leads. “Manifesting” DPVS can usually conduct impulses in both directions - anterograde and retrograde. Additional pathways with only anterograde conduction are rare, but with retrograde conduction, on the contrary, they are common.
Atrioventricular reciprocal tachycardia (AVRT) in WPW syndrome
Atrioventricular tachycardia in WPW syndrome according to the re-entry mechanism is divided into orthodromic and antidromic.
During orthodromic AVRT, impulses are conducted anterogradely through the AV node and specialized conduction system from the atrium to the ventricles, and retrogradely from the ventricles to the atria along the ventricular ventricle.
During antidromic AVRT, impulses travel in the opposite direction, with anterograde conduction from the atria to the ventricles through the ventricular ventricular junction, and retrograde conduction through the AV node or second ventricular junction. Antidromic AVRT occurs in only 5-10% of patients with WPW syndrome.
Scheme of the mechanisms of formation of antidromic and orthodromic atrioventricular tachycardia in WPW syndrome. A – mechanism of formation of orthodromic atrioventricular tachycardia during antegrade blockade of atrial extrasystole (ES) in the right-sided accessory atrioventricular junction. The excitation propagates antegradely through the atrioventricular node (AVN) and retrogradely activates the atria through the accessory anomalous pathway (ASTP); B – formation of antidromic atrioventricular tachycardia with blockade of atrial extrasystole in the RV and antegrade conduction of the impulse along the left-sided additional anomalous pathway. The retrograde impulse activates the atria through the RVA; B – antidromic atrioventricular tachycardia with the participation of two additional contralateral abnormal pathways (right-sided - DPHS1, left-sided - DPHS2). Below are diagrams of electrograms of the right (EG RA) and left (EG LA) atria and an ECG in standard lead II during tachycardia.
Classification of WPW syndrome
Manifesting WPW syndrome is diagnosed in patients with a combination of ventricular preexcitation syndrome (delta wave on ECG) and tachyarrhythmia. Among patients with WPW syndrome, the most common arrhythmia is atrioventricular reentrant tachycardia (AVRT). The term “reciprocal” is synonymous with the term “re-entry” - the mechanism of this tachycardia.
Latent WPW syndrome is established if, against the background of sinus rhythm, the patient has no signs of ventricular preexcitation (the PQ interval is normal, there are no signs of ∆-wave), but nevertheless there is tachycardia (AVRT with retrograde conduction through the RPV).
Multiple WPW syndrome is established if 2 or more DPVs are verified that are involved in maintaining re-entry during AVRT.
Intermittent WPW syndrome is characterized by transient signs of ventricular preexcitation against the background of sinus rhythm and verified AVRT. The WPW phenomenon. Despite the presence of a delta wave on the ECG, some patients may not have an arrhythmia. In this case, the diagnosis is WPW phenomenon (rather than WPW syndrome).
Only one third of asymptomatic patients under 40 years of age who have ventricular preexcitation syndrome (delta wave) on ECG eventually develop arrhythmia symptoms. At the same time, none of the patients with ventricular preexcitation syndrome, first identified after the age of 40 years, developed arrhythmia.
Most asymptomatic patients have a good prognosis; Cardiac arrest is rarely the first manifestation of the disease. The need for endo-EPI and RFA in this group of patients is controversial.
Clinical manifestations of WPW syndrome
The disease occurs in the form of attacks of frequent rhythmic heartbeat, which begins and stops suddenly. The duration of the attack is from several seconds to several hours, and the frequency of their occurrence is from daily attacks of arrhythmia to 1-2 times a year. An attack of tachycardia is accompanied by palpitations, dizziness, lightheadedness, and fainting.
As a rule, outside of attacks, patients do not show signs of structural heart pathology or symptoms of any other diseases.
Diagnosis of WPW syndrome
12-lead electrocardiography (ECG)
ECG manifestations outside of an attack of tachyarrhythmia depend on the nature of antegrade conduction along the DPVS.
With WPW syndrome, during sinus rhythm the following may be recorded on the ECG:
1. Faster propagation of the impulse through the accessory pathway (APP) leads to earlier excitation of part of the ventricles - a Δ wave appears, causing a shortening of the PR interval (PQ) and expansion of the QRS complex. This variant of the ECG corresponds to the manifesting form of WPW syndrome; the ventricular veins function antegrade and are characterized by the constant presence of a Δ wave against the background of sinus rhythm.
ECG for WPW syndrome. Faster propagation of the impulse through the accessory pathway (APP) leads to earlier excitation of part of the ventricles - a Δ wave appears, causing a shortening of the PR interval (PQ) and expansion of the QRS complex.
2. Signs of ventricular preexcitation against the background of sinus rhythm (Δ wave, causing a shortening of the PR interval (PQ) and widening of the QRS complex) may be transient. The alternation of an ECG with a Δ wave and an ECG without any changes corresponds to the intermittent form of WPW syndrome.
3. With normal sinus rhythm, the ECG does not reveal any changes. Hidden RPVs do not function in the antegrade direction, even when pacing close to their site of atrial penetration. Diagnosis is based on verification of episodes of tachycardia AVRT.
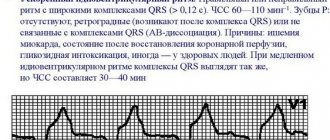
Electrocardiogram during tachycardia in WPW syndrome
Orthodromic tachycardia usually has a rate in the range of 140-240 beats/min. The QRS complex is usually narrow, in which case P waves are visible after the end of the ventricular complex with the characteristic RP WPW syndrome. ECG with orthodromic AVRT. After the QRS complex, retrograde P waves are recorded. P waves are negative in the inferior leads. DPJS has a left lower paraseptal localization.
Antidromic AVRT has a wide QRS complex and P waves are either not visible or precede the QRS complex.
WPW syndrome. ECG during antidromic AVRT. The QRS complex during tachycardia is wide and has the configuration of PNPG block. P waves are not visible.
EchoCG
Transthoracic echocardiography is performed in patients with WPW syndrome to exclude congenital anomalies and cardiac malformations (connective tissue dysplasia syndrome, mitral valve prolapse, atrial and ventricular septal defect, tetralogy of Fallot, Ebstein's anomaly).
Electrophysiological study (EPS)
Before catheter ablation of the DPVS, EPS is performed, the purpose of which is to confirm the presence of an additional pathway, determine its electrophysiological characteristics and role in the formation of tachyarrhythmia. Once the accessory pathway has been located, RFA of the RPV is performed using a steerable ablation catheter.
Treatment of an attack of tachyarrhythmia in WPW syndrome
Initial care for an episode of orthodromic AVRT consists of vagal maneuvers.
Vagal tests: Valsalva test (straining at the height of inspiration), massage of the carotid sinus (unilateral pressure in the area of the carotid triangle for no more than 10 s), cough and gag reflexes, covering the face with pieces of ice. The effectiveness of vagal tests for supraventricular tachycardia reaches 50%.
If a patient is known to have WPW syndrome, the physician may choose not to use adenosine due to its potential to induce AF. IV propafenone or procainamide can be used instead.
As an alternative, it is possible to perform immediate external electrical cardioversion. In case of hemodynamically significant symptoms during AVRT (syncope, presyncope, angina pectoris, hypotension, increasing signs of heart failure), immediate external electrical cardioversion (100 J) is indicated. If there are no associated risk factors for systemic embolization, electrical cardioversion does not require anticoagulation.
In patients with tachycardia with WPW syndrome, drugs acting on the AV node should not be used! The use of β-blockers, calcium channel blockers and cardiac glycosides is contraindicated due to the fact that they slow down conduction through the AVN and do not affect anterograde conduction through the DAVC or even enhance it. Ultimately, this is potentially dangerous with regard to the transformation of AVRT into ventricular tachycardia and/or VF.
Treatment of WPW syndrome
The method of choice in preventing recurrent tachycardia in patients with WPW is catheter ablation.
Before carrying out this procedure or in cases of refusal to perform the operation, class IC drugs (flecainide and propafenone), amiodarone, and sotalol can be used. While taking them, AVRT does not recur in 35% of patients within a year.
Drug therapy for this pathology cannot always help these patients; in addition, resistance to antiarrhythmic drugs develops in 56-70% of patients with WPW syndrome within 1-5 years after the start of therapy.
RFA DPHS
The era of interventional elimination of DPV began in 1982.
In most cases, the primary effectiveness of catheter ablation of the RPV was approximately 95%. The effectiveness of catheter ablation of DPVS localized in the lateral wall of the left ventricle is slightly higher than with catheter ablation of additional pathways of other locations. Relapses of conduction along the DPJ occur in approximately 5% of cases, which is associated with a decrease in swelling and inflammatory changes caused by the damaging effects of RF energy. Repeated RFA, as a rule, completely eliminates conduction through the ventricular vein.
Complications during endo-EPI and RFA of additional pathways can be divided into 4 groups: 1) complications caused by radiation exposure; 2) complications associated with puncture and catheterization of vessels (hematoma, deep vein thrombosis, arterial perforation, arteriovenous fistula, pneumothorax); 3) complications during catheter manipulations (damage to heart valves, microembolism, perforation of the coronary sinus or myocardial wall, dissection of the coronary arteries, thrombosis); 4) complications caused by RF exposure (arterioventricular block, myocardial perforation, spasm or occlusion of the coronary arteries, transient cerebrovascular accident, cerebrovascular complications).
Mortality associated with accessory pathway ablation procedures does not exceed 0.2%.
More “frequent” serious complications are complete AV block and cardiac tamponade. The incidence of irreversible complete AV block ranges from 0.17% to 1.0%. The incidence of cardiac tamponade varies from 0.13% to 1.1%.
Sources: 1. Revishvili A. Sh. “Clinical cardiology: diagnosis and treatment”, 2011. edited by Bockeria L.A., Golukhova E.Z. 2. National recommendations of VNOA (2012)
Treatment
Special therapy for pathology in the absence of arrhythmia paroxysms is not carried out.
External electrical cardioversion or electrical stimulation of the heart muscle through the esophagus is carried out when:
- increasing heart failure;
- angina pectoris;
- hypotension.
In some cases, attacks are stopped by:
- carotid sinus massage;
- intravenous administration of calcium channel blockers or ATP;
- use of antiarrhythmic drugs.
Urgent measures to save the patient's life are usually taken by ambulance paramedics. Subsequently, patients are prescribed continuous antiarrhythmic therapy. Today, modern drugs that are highly effective can be used.
Important! You should take the funds constantly!
The best method for eliminating dangerous pathology is radiofrequency catheter amblation. This minimally invasive operation is recommended if medications are ineffective. Intervention is also prescribed if pregnancy is planned and there is a history of at least one episode of atrial fibrillation. The operation is 95% effective. It helps prevent patient disability and significantly reduce mortality risks. The intervention involves inserting a flexible catheter into the heart. All additional pathways for conducting impulses are cauterized. Thanks to this, pathological areas are destroyed. The myocardium begins to work naturally.
Do you want the therapy to be carried out by experienced specialists? Contact our clinic in Moscow. Doctors will select the appropriate technique. Prices for all services (including a consultation with a cardiologist) will pleasantly surprise you. We adhere to a loyal pricing policy. The approximate price is indicated on the website. Our specialist will help you clarify the costs of therapy.
Republican Scientific and Practical Center for Sports Medicine
President of Uzbekistan Islam Karimov signed the Resolution “On the creation of the Republican Scientific and Practical Center for Sports Medicine under the National Olympic Committee of the Republic of Uzbekistan”
- 100027, Tashkent, Shaykhantakhur district, Olmazor street 6
- +998 ( 71 ) 241-52-45 +998 ( 71 ) 241-52-46
- [email protected]
Links
News
Insurance
Articles
Prices
Prevention
If the pathology is asymptomatic, its prognosis will be favorable. Treatment and constant monitoring by a cardiologist is required if the patient has a family history or professional indications.
Prevention of pathology is secondary. It consists of ongoing therapy. Thanks to treatment, it is always possible to prevent the occurrence of arrhythmia attacks.
Important! Prevention, like therapy, should always be carried out only under the supervision of an experienced specialist. He will correctly select the means to reduce the risks of pathology and prevent the occurrence of serious complications.
Is it possible to develop complications when PQ is shortened?
{banner_banstat6}
The phenomenon of shortened PQ cannot lead to any complications. Due to the fact that the manifestation of PQ syndrome is an attack of tachyarrhythmia, there will be corresponding complications. These include the occurrence of sudden cardiac death, fatal arrhythmias (ventricular fibrillation), thromboembolism of the cerebral and pulmonary arteries, the development of myocardial infarction, arrhythmogenic shock and acute heart failure. Of course, not every patient develops such complications, but everyone needs to remember them. Prevention of complications is timely seeking medical help, as well as timely surgery if indications for it are discovered by a doctor.
Advantages of the clinic
Our clinic employs highly qualified specialists. You can use the help of not only cardiologists, but also therapists and other doctors. They will help diagnose and eliminate the underlying and associated pathologies. All professionals comply with medical ethics and guarantee high-quality examination and prescription of adequate therapy. They have wide diagnostic capabilities. Thanks to this, doctors are able to quickly make an accurate diagnosis. Team interaction of staff makes it possible to accompany the patient at all stages of examination and therapy.
Particular attention is paid to a comfortable environment, openness and warmth of the staff, as well as a loyal pricing policy. Anyone can contact our clinic (including patients with limited financial resources). In our clinic you do not spend money on therapy, you invest it in your health.
Contact us!
Our medical center provides the widest range of services. You can always contact us regarding the treatment of diseases in cardiology. We are ready to provide you with] treatment for sick sinus syndrome[/anchor] and treatment for sinoauricular block.
Treatment process
In the absence of attacks of arrhythmia and the asymptomatic course of the syndrome, therapeutic measures are not carried out. In the presence of tachycardia, cardialgia, hypotension and other signs of cardiac dysfunction, complex therapeutic treatment is indicated.
There are two ways to relieve an attack of arrhythmia in a conservative way - vagal and medicinal. The first group includes methods of vagus nerve stimulation , which help normalize heart rhythm. This is washing with ice water, taking a sharp breath with your nose closed, straining while trying to hold your breath while inhaling deeply.
If vagal tests are ineffective, antiarrhythmic drugs : Etatsizin, Ri, Amiodarone. Electrocardioversion or electrical stimulation of the heart allows you to restore the heart rhythm in advanced cases .
During the interictal period, patients are prescribed drug treatment with antiarrhythmic drugs to prevent new arrhythmic paroxysm. Long-term use of such medications has a negative effect on the body and significantly increases the risk of developing severe complications. Therefore, modern cardiologists are increasingly resorting to surgical intervention.
Radio wave catheter ablation is an operation that destroys an abnormal muscle bundle. It is indicated for people suffering from frequent paroxysms that disrupt hemocirculatory processes and can lead to the cessation of effective heart activity. Under local anesthesia or general anesthesia, a thin probe with a sensor is inserted through the large blood vessels of the thigh. Using EPI, the area of the myocardium from which pathological impulses originate and which requires destruction is determined. After ablation of accessory fibers, an ECG is recorded. The operation is considered successful if a normal heart rhythm begins to be recorded on the cardiogram. The entire progress of the surgical intervention is monitored by doctors on the monitor of modern medical equipment.
The operation is virtually painless and minimally invasive. It gives good results in terms of complete recovery and is not accompanied by postoperative complications. After the intervention, patients feel satisfactory and do not experience symptoms of the disease.
Video: personal experience of surgery for SVC syndrome
Forecasting
Wolff-Parkinson-White syndrome is quite rare. Its etiopathogenetic features and pathomorphological changes occurring in the body have not been fully studied. Diagnosis of the disease is difficult, effective therapy is still under development, and the prognosis remains ambiguous.
In people who have undergone radiofrequency ablation of “extra” muscle bundles, the condition rapidly improves, and relapses do not occur. If there is no effect of conservative treatment or refusal of surgery, dangerous complications may develop. Despite this, statistics indicate low mortality rates from the pathology.
Since the syndrome is congenital and its exact causes have not been determined, it is impossible to prevent the appearance of abnormal muscle fibers. There are measures that reduce the risk of developing pathology, but do not completely protect against it:
- Annual visit to a cardiologist and undergoing electrocardiography,
- Vigorous physical activity - gymnastics, walking, jogging, cardio training,
- Fight against smoking and alcoholism,
- Proper nutrition,
- Pregnant women - protect the body from the effects of aggressive chemicals, viruses, and stress.
Patients with SVC syndrome are monitored by a cardiologist and take antiarrhythmic drugs to prevent new attacks of arrhythmia.
SVC syndrome is a chronic pathology. If you have the slightest complaints about your heart function or the appearance of characteristic symptoms, you should consult a doctor. Treatment carried out in full, as well as compliance with all medical recommendations, will allow the patient to count on a full and long life.