Violations of cardiac contractility are a common symptom of one or another pathological process. Not always of cardiac origin.
It exists in several types: from tachycardia, when the frequency of beats increases sharply to fibrillation, extrasystole, generation of abnormal electrical impulses outside the sinus node (natural pacemaker).
MES in medicine is Morgagni-Adams-Stokes syndrome, a severe, immediate violation of the contractility of an organ, as a result of hemodynamics and blood supply to the systems, leading to loss of consciousness.
The condition is urgent, directly life-threatening, requiring urgent first aid and hospitalization of the patient to determine the cause and prescribe primary treatment.
Attention:
Conservative methods are ineffective in therapy. You can only help in a radical way.
Only implantation of a pacemaker gives a chance for a quality life. It leads the rhythm artificially and does not allow pathological impulses to be generated.
The prognosis is relatively unfavorable. Not only Morgagni syndrome is dangerous, but also the main diagnosis that brought it to life.
Development mechanism
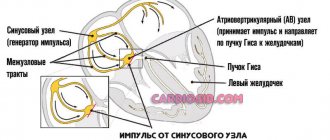
The essence of the pathological process is an acute blockade of nodes, bundle branches and other structures of the conduction system of the heart.
In 80% of cases, patients with even a single attack have AV block.
The atrioventricular node, responsible for conducting impulses to the ventricles, does not perform its function.
As a result of an acute disorder, the sinus node functions in vain. The ventricles do not contract. Compensatory activity begins in the chambers, each producing its own electrical impulse.
Chaotic movement leads to cerebral ischemia, blood circulation throughout the body is disrupted. This may result in the death of the patient. Depending on the intensity of the process.
Recovery is urgent, in a hospital setting. Mild episodes are treated on the spot with medication.
general information
Reperfusion syndrome: causes, symptoms, treatment and prevention
MAS syndrome was first studied in 1761 by the Italian physician D. Morgagni. In 1791, Irish cardiologists became interested in the syndrome: W. Stokes, R. Adams. It was these three scientists who fully studied the development, causes, and symptoms of the pathology, which is why the syndrome is named after them. The condition is a sharp violation of the contractility of the heart, resulting in a sharp disturbance of hemodynamics. Organs and systems are deprived of adequate blood flow, which leads to loss of consciousness.
The pathology is more common among people who have intracardiac conduction disturbances, heart rhythm disturbances due to the cessation or weakening of the sinoatrial node. More often, the pathology develops in men aged 45 to 60 years. People living in megacities and prone to a passive lifestyle are more susceptible to pathology. In underdeveloped countries, the syndrome is rare.
Important!
Loss of consciousness with MAS occurs when there is no contraction of the ventricles for 10-20 seconds.
Classification
Morgagni-Adams-Stokes syndrome is typified by the prevailing symptom, the type of rhythm disturbance.
- Bradyarrhythmia. Accompanied by a sharp drop in heart rate, less than 40 beats per minute. Critical levels give an unfavorable prognosis; urgent resuscitation is needed.
The patient almost immediately loses consciousness and remains in this state until correction; it is almost impossible to bring them out of this position. The brain does not receive enough nutrients and oxygen.
It is considered the most dangerous form, since it occurs suddenly and poses a particular threat to health and life.
- Tachysystole. Accompanied by acceleration of cardiac activity. Up to 150-200 beats per minute. It is not the heart rate that needs to be corrected, but the underlying pathological process. Before an acute condition develops, there are several minutes for the patient to react. Darkening in the eyes, shortness of breath, nausea, sweating and other “delights” of this situation accompany the person.
- Mixed variety. First tachycardia, then bradycardia. There are no fundamental differences in symptoms or clinical picture. Need urgent help.
All presented classifications are used after the fact to determine the etiology (root cause) of the process and develop treatment options.
At the first stage, emergency correction of the condition is needed. Only then can a diagnosis be prescribed. It’s better to go to the hospital in case the attack repeats.
Causes
Development factors are multiple. But they almost always have a cardiac origin.
- Severe tachycardia of paroxysmal type. Manifested by a heart rate of 180 or more. The higher it is, the greater the likelihood of an attack of MES. Urgent medical attention is required.
- The reverse process is bradycardia. A drop in contraction frequency to a level of 50 or less ends with a violation of contractility and a damping of the intensity of bioelectric impulse generation. It is possible that intra-atrial conduction may slow down as a possible deviation from the norm.
- Ventricular fibrillation. Generation of its own signal by chambers (ventricles). An abnormal source of activity occurs outside the sinus node. Usually this is the result of some organic pathology. Less often functional. An extremely life-threatening condition that can result in cardiac arrest even before the formation of a Morgagni-Adams-Stokes attack or as a logical addition to it.
- Total atrioventricular block (AV). Accompanied by the impossibility of signal movement from the sinus cluster to other structures.
- Previous heart attack, myocarditis and other conditions leading to the death of active heart tissues and their severe scarring (cardiosclerosis).
- Disruption of the central nervous system as a result of brain tumors, infectious processes and other conditions.
The reasons are assessed in the system. The exclusion is being carried out gradually. Primary phenomena are identified relatively simply, within the framework of minimal diagnostics using ECG, echocardiography and daily monitoring.
Symptoms
Manifestations of Morgagni-Adams-Stokes syndrome are specific. The clinical picture develops according to the same pattern with minor differences.
Deploying the full list of features takes 1 to 3 minutes on average. Sometimes seconds count. All manifestations can be divided into preceding and accompanying ones.
Previous signs
- Dyspnea. Not associated with physical activity. The patient can sit peacefully in a chair or stand in line. Accompanied by an increase in the number of movements, tachypnea is caused by a sharp drop in the intensity of gas exchange. This is a compensatory mechanism aimed at restoring oxygen concentration in the blood.
- Darkening in the eyes. Prevents the onset of fainting. In addition to the visual impairment itself, there is a painful tinnitus, all surrounding sounds are irritating and painful. Weakness, drowsiness. The patient cannot stand on his feet, the muscles lose tone.
- Dizziness. Vertigo leads to the inability to navigate in space. The world is going round and round. If you do not sit down, you may fall and get injured.
- Severe bursting pain in the chest. It felt like sewing up a heavy stone. This is the result of a rhythm disturbance in cardiac structures. Specific sign.
- Acute cephalalgia. Pain in the eyes, forehead, crown. Can squeeze, pull, knock.
Next comes the attack of MES (MAS): accompanied by cardiac symptoms, but the patient no longer feels anything. After 30-60 seconds, loss of consciousness occurs. Next, objective moments are recorded.
Associated symptoms
- Pale skin all over the body. The result of narrowing of peripheral vessels, insufficient blood circulation at a generalized level. The color of the mucous membranes of the gums also changes.
- Cyanosis of the nasolabial triangle. The area around the mouth is framed by a bluish ring. The shade is typical for the corners of the lips.
- Consciousness is consistently absent. Deep fainting occurs. It will not be possible to bring the patient out of such a state either by calling out or using physical force. Ammonia will also have no effect. When providing first aid, this must be taken into account and not waste time on useless manipulations.
- Breathing becomes shallow. It is impossible to detect it without special tools. The chest hardly moves.
- When measuring vital signs, a drop in blood pressure to critical levels is detected. This is an unstable level. Then comes growth. Such “swings” are the result of the body’s convulsive attempts to restore its own state. It is necessary to bring blood pressure back to normal to prevent it from getting worse.
- No visible pulse. It cannot be felt or is detected with great difficulty. An assessment of the condition using instrumental methods is required. Stopping cardiac activity is the basis for urgent resuscitation measures.
- Cramps. The muscles of the arms and legs move. These are spontaneous contractions, an alarming symptom. It speaks of the transition of the condition to a more severe phase.
- Emptying the bladder and bowels. The same. The unequal system suffers.
Without qualified correction, the patient's death may occur. Only a doctor can prevent such an outcome. All possible assistance in normalization is required from others.
Symptoms
A classic seizure is characterized by rapid development and a certain sequence of changes. Within 3-5 seconds from the moment the arrhythmia or blockade occurs, the patient develops a pre-fainting state. Suddenly dizziness, headache, incoordination, disorientation, and pallor appear. Profuse cold sweat appears on the skin. Palpation of the pulse reveals pronounced tachycardia, bradycardia or an uneven rhythm.
The second stage lasts 10-20 seconds. The patient loses consciousness. Blood pressure and muscle tone decrease. Acrocyanosis is visually determined, and small clonic convulsions develop. With ventricular fibrillation, Hering's symptom is noted - a peculiar buzzing in the area of the xiphoid process of the sternum. After 20-40 seconds, the convulsions intensify, take on an epileptic shape, and involuntary urination and defecation occur. If the rhythm is not restored after 1-5 minutes, clinical death is observed with the disappearance of pulse, breathing, and corneal reflexes. The pupil is dilated, blood pressure is not determined, the skin is pale, marble in color.
An abortive course of the attack with a reduction in symptoms within a very short time period is possible. The cerebral cortex does not have time to undergo severe hypoxia. The main symptoms observed with this variant of the pathology are dizziness, weakness, transient blurred vision, confusion. The symptoms disappear in a few seconds without medical intervention. Such types of MAS are extremely difficult to diagnose, since similar symptoms are detected in many other conditions, including cerebrovascular disease.
First aid algorithm
The main thing to do is call the emergency team. Until the doctor or paramedic arrives. Next, it is necessary to stabilize the victim’s condition. If possible.
What needs to be done and in what order?
- If a person is outdoors in the cold season, move him indoors or, as a last resort, lay something warm under his body.
- Loosen your collar or remove your body jewelry. Pressure on the carotid sinus in the neck will cause a reflex drop in blood pressure and heart rate. This is certain death in this situation.
- Open a window or window (in the room) to ensure normal ventilation. Restoration of gas exchange is required in all cases, this is important.
- Measure blood pressure and heart rate. These indicators must be reported to arriving doctors.
- Drugs are not given to an unconscious person.
- Turn your head to the side and release your tongue in case of vomiting.
- Heart rate is constantly monitored. In the absence of cardiac activity, direct massage is indicated. The palms are folded and rhythmically pressed on the chest 100-120 times per minute.
A rib fracture is not a reason to stop resuscitation efforts. If you have no experience in artificial respiration, it is better not to do it. There will be no point.
Upon arrival of the brigade, all activities cease. Briefly provide information about the victim and his condition. If necessary, you can accompany the person to the department.
What definitely should not be done
- Leave the patient lying in the cold. Hypothermia will lead to spasm of the coronary arteries, a profound deterioration of the condition. The patient needs to be moved indoors. This will also protect against frostbite; blood flow is already minimal, and tissue damage is possible.
- Giving drugs, especially putting them in the mouth by force. Possible asphyxia if inhaled.
- Intravenous administration and injections are prohibited. It is not known what caused the condition. Even if you have a medical education, you won’t be able to establish this right away.
References
- Rodionovskaya, S.R., Nikishina, I.P. Macrophage activation syndrome in patients with systemic juvenile arthritis. Scientific and practical rheumatology, 2014. - No. 2.
- Potapenko, V.G., Pervakova, M.Yu., Lapin, S.V. and others. The role of fractional analysis of ferritin in the diagnosis of secondary hemophagocytic syndrome. Clinical laboratory diagnostics, 2018. - No. 1.
- Juvenile arthritis. Clinical recommendations. Union of Pediatricians of Russia, 2021. - 92 p.
- Kasper, D., Fauci, A., Hauseret, S. et al. Harrison's Principles of Internal Medicine 19/E. McGraw-Hill Education, 2015. - Vol. 1.
- Ravelli, A., Davì, S., Minoia, F. et al. Macrophage Activation Syndrome. HematolOncolClin North Am., 2015. - Vol. 29(5). — P. 927-41.
Possible consequences of an attack
They depend on the type of pathological process, as well as the moment of starting first aid, qualified treatment in a hospital and recovery from the condition.
Typical complications:
- Cardiac arrest as a result of complete non-conduction of the sinoatrial node, His bundle, or total dysfunction of the sinus node. Asystole is the cause of death in the majority of cases. Moreover, recurrent attacks are associated with a high risk of death.
- Heart attack. As a result of stenosis of the coronary arteries and necrosis of active tissues.
- Stroke. Also a likely consequence. It is considered almost a classic of the genre. Accompanied by acute malnutrition of cerebral structures. Hence the death of nerve bundles. Even with the restoration of normal functioning, neurological deficits of varying degrees of severity remain.
- Pulmonary edema. As a result of insufficient outflow of blood from the small circle, its stagnation. Restoration is carried out urgently.
The result is at least severe disability for the patient. Death is also a likely outcome.
Doctors do not always have to deal with only one complication. They develop right at the moment of the acute course of a Morgagni-Adams attack.
This presents particular difficulties when bringing a person out of a critical situation and significantly worsens the overall prognosis.
Symptoms
When a person is diagnosed with Morgagni-Morel-Stewart syndrome, there are a number of symptoms that characterize it:
- Patients begin to experience regular headaches.
- Obesity, mainly in the abdominal area.
- The skin retains its normal color, but pyoderma and weeping eczema often appear on it.
- Most patients have severe hypertrichosis.
- The skin becomes pasty, the lower extremities begin to swell, and acrocyanosis appears.
- The muscles are weakening.
- Changes occur in the cardiovascular system and respiratory organs (the boundaries of the heart expand, deafness of tones and heart failure are noted).
- Tendency to collapse, catarrh of the upper respiratory tract and bronchopneumonia.
- Changes in the endocrine glands do not have any characteristic features. Metabolism can be normal, increased or decreased.
- Tolerance to carbohydrates decreases. Diabetes mellitus often manifests itself clearly.
- The menstrual cycle is disrupted. During pregnancy during this period, the patient's condition worsens.
- Nervous and mental disorders are observed. They manifest themselves in the form of emotional lability, irritability, insomnia and a tendency to depression.
- The internal frontal plate has hyperostosis, and the bones of the skull often thicken. In some cases, the size of the sella turcica even increases.
Diagnostics
It is carried out in a hospital. But after first aid. The condition is too serious to delay.
The minimum program includes a visual assessment of the skin, mucous membranes, measurement of blood pressure, frequency of contractions of a muscle organ, and auscultation (listening to heart sounds).
Next comes first aid. It is possible to use Atropine or Epinephrine to restore adequate myocardial contraction, electrocardioversion, defibrillation to normalize the conductivity of structures.
Upon completion, already in a hospital setting, a group of activities is prescribed:
- Oral interview, history taking. What complaints, how long ago did they arise, whether there were attacks before, how severe, previous and current diseases of any profile, lifestyle, family history, operations in the past, etc.
- Auscultation (listening for a heartbeat).
- Repeated blood pressure and heart rate measurements.
- Daily monitoring. To assess heart rate and blood pressure over time, after the patient’s usual activity (as far as possible).
- Electrocardiography. Normally it shows no deviations. Changes are present in pathologies that can lead to MES syndrome.
- Echocardiography. To assess the organic state of tissues and structures.
- MRI if necessary.
- General blood test, biochemical, hormones.
The neurological status is examined as part of the identification of deficiency disorders.
Clinical picture
The main wedge, symptoms in MS—hyperostosis of the internal plate of the frontal bone, obesity (of the hypothalamic type with uniform fat deposition) and hirsutism (see)—make up the classic Morgagni triad; disorders may be observed at the same time: emotional and mental (emotional instability, memory loss, sleep disorders, increased fatigue), autonomic and neurological (bulimia, polydipsia, ptosis, ocular convergence disorders, headaches, dizziness, sweating, trophic changes in the skin and mucous membranes of the genitals organs, increased blood pressure, sometimes epileptiform seizures) and neuroendocrine (disorders of carbohydrate metabolism, ovarian-menstrual function such as opso- and amenorrhea, infertility). The exchange of calcium and phosphorus is not impaired. The central mechanism of ovarian dysfunction is confirmed by the presence of changes in the ratio of the level of excretion of gonadotropins - follicle-stimulating hormone (FSH) and luteinizing hormone (LH) of the pituitary gland. With opsomenorrhea (see Menstrual cycle), the level of excretion of FSH and LH is reduced, but cyclic fluctuations in this level are noted. With prolonged amenorrhea, the excretion of both FSH and LH is sharply reduced and there are no pronounced fluctuations in the quantitative excretion of gonadotropins.
To identify the functions and state of the brain in M. s. electroencephalography is used (see), while in some patients the EEG in leads from the frontal and precentral parts of the brain is dominated by clearly expressed theta activity with a frequency of 5-7 oscillations per second; the reaction of depression of the basic rhythm to continuous light is weakened. Other patients have pronounced phenomena of irritation with a predominance of frequent activity in all leads from the cerebral cortex. In many patients, deviations are detected only under the influence of functions and loads. A certain relationship has been established between the symptoms of the disease and EEG data. With bulimia (see), polydipsia (see), trophic changes in the skin and mucous membranes, emotional and mental disorders, headaches, disturbances in the diencephalic region are detected on the EEG. With brainstem disorders - moderate ptosis (see), ocular convergence disorder (see) - and headaches, changes in the reticular formation of the midbrain predominate on the EEG. When the above symptoms are combined with increased blood pressure and impaired carbohydrate metabolism, the EEG shows disturbances in the meso- and diencephalic structures.
Expressiveness wedge. The picture, as a rule, is not related to age and duration of the disease, but depends on the function and activity of the pituitary gland.
Treatment methods
It is carried out under the supervision of a cardiologist. In the long term, drug therapy is ineffective, but it is used at the initial stage to ensure the stability of the patient’s condition.
The following drugs are prescribed:
- Antihypertensive drugs of various types. From ACE inhibitors to calcium antagonists and centrally acting agents. Depends on the main diagnosis and the degree of deviation of blood pressure from the standard.
- Antiarrhythmic. Amiodarone. Other drinks are strictly prohibited. Provocation of the syndrome is possible.
- Cardioprotectors. Restore normal metabolism in the tissues of cardiac structures. Mildronate.
- Cerebrovascular drugs. For adequate blood flow in the brain. Piracetam or Actovegin as the main ones.
A similar scheme is followed until the health status is normalized, heart rate and blood pressure are consistently adequate, and neurological symptoms are relieved.
Next, surgery is scheduled. The main way to eliminate the syndrome is implantation of a pacemaker. Morgagni-Adams-Stokes attacks stop developing as conduction is artificially normalized. Exceptions are extremely rare (no more than 5% of situations).
Establishing diagnosis
Loss of consciousness is possible with various diseases. Therefore, when conducting diagnostics, Adams-Stokes-Morgagni syndrome must be differentiated from the following conditions:
- Meniere's syndrome;
- hypoglycemic state;
- stroke;
- hysteria;
- orthostatic hypotension;
- attack of transistor ischemic attack of the brain;
- severe aortic stenosis;
- pulmonary embolism;
- thrombosis of the heart chambers;
- epilepsy.
To determine the syndrome, the following diagnostic methods are used:
- electrocardiogram (ECG) in dynamics;
- ECG monitoring using a Holter device (allows you to identify temporary changes, a combination of atrial flutter and fibrillation);
- long-term electroencephalogram monitoring;
- contrast coronography of vessels;
- myocardial biopsy.
Forecast
Depends on the quality of first aid, the moment of the start of emergency measures of a qualified plan.
Many factors need to be taken into account: age, general health, gender, history of illness, chances of undergoing radical treatment and implantation of a pacemaker, bad habits, family history and other points.
The ability to undergo surgery is associated with maximum survival. Almost 95%. Only 5% of patients have a worse prognosis, and not in absolute terms. It just requires additional correction. Stroke, heart attack, and other complications significantly worsen the outcome.
Questions of this nature should be addressed to your primary physician. Outsiders do not know the patient well enough, so they are unlikely to say anything right away. It is also impossible to take into account all the nuances on your own.
What does this mean?
The severity of the consequences directly depends on the frequency of seizures and their duration. Frequent and prolonged brain hypoxia entails a negative prognosis for the disease.
Hypoxia lasting more than 4 minutes causes irreversible brain damage. The absence of resuscitation measures (indirect cardiac massage, artificial respiration) can lead to cessation of cardiac activity, disappearance of bioelectrical activity and death.
The prognosis for surgery is positive. Implantation of a pacemaker allows you to restore the patient’s quality of life, ability to work and health.