Magnetic resonance imaging is an informative non-invasive way to study cerebral structures. Diagnosis of pathological processes in the brain using other methods is complicated by the presence of the skull, which performs a protective function. Scanning using an induction field allows you to identify the slightest changes. Foci of gliosis are most accurately detected on MRI of the brain; a specialist can determine the nature and localization of the process.
Various forms of gliosis on MRI images of the brain
The study is carried out using a tomograph consisting of a mobile table and a wide tunnel. The device generates a magnetic field, under the influence of which the hydrogen atoms in water molecules are aligned in a special way. Sensitive sensors read the response of scanned tissues, obtaining information about the degree of fluid saturation of brain cells.
A computer program converts the signal into a series of layer-by-layer images taken in axial, sagittal and frontal projections. Based on the images obtained, the doctor can, if necessary, reconstruct a 3D model of the brain.
General information
Gliosis of the brain is a pathological process manifested by the replacement of neurons with glial elements.
Gliosis is not an independent disease; rather, it is a protective reaction to the death of neurons, that is, a secondary process. At the same time, the process of destruction of neurons stimulates the filling of the resulting voids with glial cells, which leads to a change in the quantitative ratio of elements of the nervous tissue. Brain tissue consists of a collection of neurons, ependymal membrane and glial cells. Normally, glial tissue is responsible for trophic/secretory functions and metabolism in brain cells, and also performs the function of protecting neurons. It accounts for about 40% of the total brain mass. The proliferation of glial cells forms foci of gliosis in the white matter of the brain, which, depending on the etiology of the primary disease, can be focal/diffuse in nature. Foci of gliosis can be located in any area (structures) of the brain. And the more glia are formed, the less efficiently the central nervous system functions. With a large proliferation of glia, a cystic-gliotic atrophied area of brain tissue can form. The more glia are formed in the white matter, the worse the functioning of the entire nervous system. A cystic-glial-atrophic area is formed.
There are no statistical data on the incidence of various types of gliosis. It can only be noted that supratentorial foci of gliosis are most common.
Supratentorial lesions - what are they? Supratentorial are foci of gliosis of vascular origin. Various pathological processes in the vessels of the brain ( thrombosis , fibrosis , necrosis ) that cause circulatory disorders contribute to the formation of small hyper/hypertensive areas, which are accompanied by such disorders as poor coordination, dizziness , and changes in handwriting.
Single foci of gliosis
Focal gliosis is characterized by single, clearly defined islands in the white matter, the size and location of which is determined by the causes of neuronal death. They occur in people of any age and, perhaps, as a manifestation of natural age-related degenerative processes in brain tissue, ischemia of cerebral structures, local inflammatory process, chronic hypertension demyelination process , and as a consequence of injuries during childbirth in infants. Typically, single (limited foci) of gliosis of the brain are an accidental finding on CT/MRI, since in most cases they are not clinically manifested and do not cause discomfort, with the exception of their localization in the frontal lobe, where the centers associated with feelings and sensations are located, which can manifested by the appearance of hallucinations. A single gliosis of the brain is not prone to proliferation.
Multiple foci of gliosis
The appearance of multiple foci of gliosis is caused by injuries and acute/chronic circulatory disorders of the brain, that is, of vascular origin. As the pathology/disease that causes neuronal death develops, both the number and size of the altered areas increase. They occur predominantly against the background of severe atherosclerosis , stroke , cerebral infarction , with compression of cerebral vessels and as a result of age-related changes. Multiple foci of gliosis for the most part enhance the clinical symptoms of the underlying disease and cause dysfunction of the central nervous system.
The best medications for therapy
For all the measures described above to be effective, you need to support the sick body with special medications. Doctors have mixed opinions about which medications are best to use to treat cerebral gliosis. But they agree on one thing - treatment should be medicinal, not folk. The five most popular prescribed drugs include the following:
| Drug name | Active substance | Manufacturer |
| Cavinton | Vinpocetine | Hungary |
| Cinnarizine | Cinnarizinum | Bulgaria and Russia |
| Actovegin | Deproteinized calf blood haemoderivative | Austria |
| Glitsed | Glycine | Ukraine |
| Vinpocetine | Vinpocetine | Russia, India, Belarus |
To the described vasoactive drugs, you need to add antiplatelet agents to improve blood flow, amino acids, and nootropics. Vitamins E or B provide good support for treatment. But the most important thing is to choose the right main medicine. To do this, you should familiarize yourself with contraindications and side effects, and also consult your doctor. As stated earlier, his decision should be based only on complete brain studies.
Cavinton
Cavinton increases the consumption of glucose and oxygen by the tissues of the frontal lobes. That is why it is used in the treatment of the consequences of ischemic stroke, vascular dementia, atherosclerosis and other diseases. Sometimes the drug is used in ophthalmology: it treats chronic diseases of the blood vessels of the eye and its retina. The medicine should only be used after consultation with a doctor, otherwise the risk of side effects is too high. Know that:
- distributed in the form of tablets or concentrates for infusion;
- the dosage is determined strictly on an individual basis;
- the medicine costs from 228 to 850 Russian rubles.
With the correct dosage, the drug rarely produces side effects. But sleep disturbances, dizziness, tachycardia, nausea, and heartburn may occur. Less common are increased sweating, rapidly passing allergic skin reactions and general weakness. By the way, it may be a manifestation of an underlying disease.
The medicine does not have a negative effect on patients with kidney or liver diseases.
Cavinton is strictly prohibited for patients with severe coronary heart disease, serious arrhythmias, and the acute phase of a stroke. It is dangerous to prescribe it to pregnant women or nursing mothers. But this is acceptable if the risk to the mother’s health is more serious than the likely side effects for the child. Pregnant women may experience placental bleeding from taking it, and there is a risk of spontaneous abortion.
Cinnarizine
A selective blocker of slow calcium channels called Cinnarizine is used not only in the treatment of gliosis and its consequences. It is used in the treatment of post-stroke conditions, traumatic brain injuries, migraines, vestibular disorders, kinetosis, and encephalopathy. The medicine quickly relieves dizziness, tinnitus, nausea and vomiting. Cinnarizine has the following characteristics:
- Available in the form of tablets of 50 milligrams;
- tablets are taken orally after meals, the exact dose depends on the severity of the patient’s condition;
- It is difficult to answer exactly how much Cinnarizine costs, but usually its price ranges between 37 and 101 rubles.
Cinnarizine has few contraindications. It is not given only to pregnant, lactating women, and people with allergies. The medicine should be used with caution if a person is diagnosed with Parkinson's disease. But side effects are possible. Among the most common are drowsiness, lack of hunger, fatigue, dyspepsia and dry mouth. In exceptional cases, lichen planus and serious weight gain are recorded.
- Treatment of cerebral vessels: folk remedies, traditional medicine
Actovegin
This medicine is prescribed for cognitive impairment, which includes dementia and the consequences of strokes. It is occasionally used for diabetic polyneuropathy or circulatory disorders. Thanks to the active substance, the medicine increases the rate of blood flow in the capillaries. After systemic use, it improves the morphological and physiological state of the central nervous system. Remember, that:
- Available in the form of digestible tablets or injection solutions;
- first, the body should receive 10-20 milliliters of Actovegin, and then five milliliters per day;
- packaging of the drug will cost 568-1928 Russian rubles.
Actovegin rarely leads to side effects. But in particularly sensitive patients, drug fever, symptoms of shock, urticaria, and sudden redness in the injection area are recorded. Sometimes doctors observe myalgia, but the exact frequency is unknown. Actovegin is prohibited in case of pulmonary edema, decompensated heart failure, oliguria, anuria or long-term fluid retention in the body.
Glitsed
Glitsed is prescribed for cerebral circulatory disorders, traumatic brain injuries, and neurocirculatory dystonia. It helps in the fight against psychological overload, improves memory, relieves insomnia and facilitates vigorous physical activity. As part of the treatment of cerebral gliosis, the drug has only an auxiliary effect. A brief description of Glitsed is as follows:
- sold in the form of flat white or cream tablets;
- as a rule, one tablet is prescribed three times a day;
- the cost starts from 136 rubles, but you can find cheaper offers on the Internet.
The medicine rarely has side effects, especially if used in the treatment of cystic glial changes in the brain. But allergic reactions on the skin are possible; indigestion, headache, and nausea occur less frequently. In exceptional cases, increased irritation and poor concentration are observed. The overdose was either not recorded or not observed.
Vinpocetine
According to the instructions, Vinpocetine is prescribed for insufficient cerebral circulation, for damage to the blood vessels and retina. Sometimes they treat vegetative-vascular dystonia against the background of climatic syndrome. For patients with gliosis of the brain, Vinpocetine is prescribed to improve metabolism in the affected organ and normalize blood flow. It is important to remember the following characteristics of the medicine:
- the drug is available in the form of tablets for oral administration or solution for injection;
- The dosage regimen is individual, since the dosage varies depending on the severity of the patient’s condition;
- the average price is 50-164 rubles.
Vinpocetine is contraindicated in case of coronary heart disease, stroke or severe signs of arrhythmia. It is dangerous to give it during pregnancy or lactation. Even if the dosage and rules of administration are followed, side effects are possible. Typically, adults experience insomnia, dizziness, increased heart rate, surges in blood pressure, profuse sweating, or allergic reactions.
Classification
The classification is based on the nature of the proliferation of glial cells and their localization.
Based on morphological characteristics, the following are distinguished:
- The isomorphic form is characterized by an ordered proliferation of neuroglia.
- Anisomorphic form - has a pronounced cellular structure and is characterized by chaotic growth; most often localized subcortically/paraventricularly. Periventricular gliosis - formed in the ventricles of the brain. Often periventricular gliosis is accompanied by the development of cysts. Fibrous form—the predominance of the fibrous type structure is noted.
According to the localization of the pathological process, the following are distinguished:
- Periventricular gliosis - glial cells are formed in the ventricles of the brain. Periventricular gliosis is often accompanied by the development of cysts.
- Perivascular (vascular) gliosis is the growth of glia along atherosclerotic vessels. It is often diagnosed on MRI as microangiopathy with the presence of foci of gliosis.
- Subependymal gliosis is predominantly localized on the inner lining of the ventricles of the brain.
- Marginal gliosis - located on the surface of the brain.
- Marginal gliosis - foci of degeneration are localized in the intrathecal region.
Based on quantitative criteria, single and multiple foci of gliosis are distinguished. Histologically, hypodense (without a definite structure, cannot be stained) and hyperintense (clearly structured, well stained) areas of gliosis are distinguished.
Based on the nature of the process/prevalence, the following are distinguished:
- A focal type of flow, involving a limited area of the brain (usually in the temporal/parietal regions).
- Diffuse type of course - characterized by multiple lesions of various sizes/localizations. Most often of vascular origin and may have the appearance of a cystic-gliotic formation.
Turning to traditional methods of therapy
No matter how many medications are prescribed to the patient, additional maintenance of the body through the use of folk remedies will help improve the general condition.
- At the initial stage, in the presence of a few lesions, herbs perfectly support the human body, which help stabilize the blood supply system and increase metabolism.
- If a patient develops obesity, a diet based on a raw food diet is recommended; fasting days with periodic fasting are also required. This will contribute to the overall cleansing of the body from various substances that interfere with its healthy functioning.
- Taking tinctures and various decoctions, the action of which is aimed at combating the symptoms of the disease. At the pharmacy you can buy ready-made preparations that are balanced for treatment.
It must be emphasized that treatment using traditional methods can only be effective as a complement to traditional therapy, which should be prescribed by specialists. A long-term effect from the use of medications and treatment using traditional methods will not be achieved until the cause of glial formation is eliminated. Next, we will find out what preventive measures will help people avoid developing this disease.
How long do adults with cerebral gliosis live? This is a common question. More on this later.
Causes
The pathological process of replacing neurons with neuroglial cells may be based on a variety of reasons:
- Age-related changes caused by the natural process of neuron death.
- Diseases of hereditary origin - lysosomal storage disease ( Tay-Sachs disease ), inherited in an autosomal recessive manner, characterized by massive death of neurons in children, which is the cause of their death); genetically determined pathology - tuberous sclerosis .
- Birth injuries at birth.
- Traumatic brain injuries.
- Multiple sclerosis (destruction of myelin and the formation of foci of demyelination in various brain structures).
- Cerebral infarction (ischemic stroke).
- Hemorrhagic stroke is a hemorrhage into the structures of the brain, which forms foci of gliosis of vascular origin.
- Brain swelling.
- Epilepsy.
- Arterial hypertension/encephalopathy caused by a persistent increase in blood pressure.
- Neuroinfections ( encephalitis , meningitis ). oxygen starvation of brain tissue ( hypoxia ).
- Hypoglycemia (low blood sugar).
- Surgical interventions on brain structures.
- Atherosclerosis of cerebral arteries.
- Abuse of products containing animal fat.
Types of changes
In medicine, dystrophic manifestations in the brain substance are divided into two types:
- Diffuse.
- Focal.
In the first case, pathological changes spread evenly to the entire brain, and not to its individual areas. They are caused either by general disturbances in the functioning of the blood supply system or by infections (meningitis, encephalitis, etc.).
An important cause of this condition is thought to be changes in blood flow to the area around the ventricles of the brain, which is fragile and prone to injury, especially before 32 weeks of gestation. Premature babies with intraventricular hemorrhage are also at increased risk of developing this condition
Exams used to diagnose periventricular leukomalacia include ultrasound scanning and MRI of the head. The cardiac, pulmonary, intestinal and renal activity of premature infants is carefully monitored and treated in the Neonatal Intensive Care Unit.
Diffuse changes are manifested mainly by a decrease in a person’s performance, a dull headache, difficulty switching to another type of activity, a narrowing of the patient’s range of interests, apathy and sleep disorders.
And what a focal change in the brain substance of a dystrophic nature is can be understood by the fact that it can be caused by various minor pathologies:
These problems often arise during the first or second year of life. This condition can cause cerebral palsy, especially stiffness or increased muscle tone in the legs. These will likely be those that compromise movements such as sitting, crawling, walking, and weapon movement. These children may require physical therapy. Extremely premature babies have more problems with learning than with movement.
The child should visit his regular pediatrician for scheduled exams. Neonatal diseases of prenatal and perinatal origin. Hypoxico-ischemic encephalopathy: neuropathology and pathogenesis. Introduction. The predominant semiologic picture should be considered in conjunction with the patient's clinical context and epidemiological data to reach a diagnostic conclusion.
- cysts (small cavities that form in the brain),
- small foci of necrosis (tissue death in certain areas caused by lack of nutrients);
- gliomesodermal (intracerebral) scars that occur after injuries and concussions;
- minor changes in the structure of the brain matter.
That is, these are pathologies that cause disturbances in the blood supply in a small area. True, they can be either single or multiple.
The microcirculation of the brain forms a very complex vascular network of anatomy and varies among individuals. The vesicular arteries, in their deep course in the white matter, establish very little capillary anastomosis with adjacent nutritional arterioles, constituting relatively independent arterial metabolic units. On the other hand, the deep subepidemic arteries, which occur in the choroidal arteries, give penetrating branches to the white matter, although its path is shorter than that of the parade ground arteries.
There is a second terminal system of cortical and subepidemic arteries that supply the basal ganglia. There is very little anastomosis between the superficial and deep arteriolar systems. The arterial and venous systems are anatomically quite parallel. The perivascular space surrounds the wall of arteries and arterioles, as well as veins and venules, from the subarachnoid space to its intraparenchymal path.
Symptoms
Clinical symptoms vary widely and are determined mainly by the symptoms of the underlying disease that caused gliosis. As a rule, single small foci of gliosis do not produce specific neurosymptoms and are discovered by chance during an MRI examination of the brain. At the same time, multiple (extensive) foci of gliosis almost always manifest neurosymptoms in the form of:
- Unreasonable long-term intense headaches that are not controlled by taking antispasmodics.
- Blood pressure instability (sudden changes in a short period of time).
- Periodically occurring dizziness .
- Decreased performance/increased fatigue.
- Changes in visual/auditory perception.
- Disorders of coordination, attention and memory.
- Motor disorders (with large lesions, up to convulsive conditions).
Clinical symptoms are largely determined by the localization of the focus of gliosis:
- Localization of foci of gliosis in the temporal lobes is characterized by frequent, intense, long-term headaches. With the vascular genesis of the process, the pain syndrome is combined with sudden changes in blood pressure.
- Supratentorial gliosis manifests itself mainly with visual disturbances – hallucinations; distortion of the outlines, sizes, shapes of objects; loss of visual fields, difficulty recognizing an object by appearance.
- Gliotic foci in the white matter of the brain can cause dizziness , an episyndrome characterized by increased convulsive activity with the possible development of epileptic seizures. Such symptoms develop as a complication of traumatic brain injury/surgery.
The localization of gliosis foci in the frontal lobes is often due to age-related changes. It is generally accepted that if diseases that can cause the death of neurons and the proliferation of glial cells have not been identified, then such a process should be considered a primary pathology that develops as the body ages and manifests itself as impaired concentration, attention, memory, fine motor disorders, and slowed reactions.
Symptoms
Clinical manifestations are divided into general and focal. The latter manifest themselves depending on which part of the brain the pathological formation is formed.
General symptoms
General signs of brain cancer (or a benign tumor) arise due to increased pressure inside the skull, compression of neighboring tissues by the tumor body and the negative influence of its metabolites. Common symptoms include:
- dizziness, headache, discomfort in the head;
- dyspeptic manifestations not related to food intake or poisoning;
- loss of appetite, weight loss;
- blurred vision;
- changing the psycho-emotional behavior habitual for a person;
- memory problems, weakening of mental activity;
- signs of epilepsy.
It's important to understand. That general symptoms are not specific. If they bother you regularly, you need to urgently visit a doctor.
The pathological process in the early stages, as a rule, occurs latently or its signs are weak. Often neoplasms are found by chance, when examining a patient for another disease or for preventive purposes.
Focal symptoms
These are specific signs that arise as a result of damage to the cerebral structures of the central nervous system. The clinical picture depends on the location of the pathological focus:
- Glioma of the optic nerve is formed from cells of its trunk. Tissue growth is slow, accompanied by infiltration, but does not grow into the dura mater. The neoplasm is considered benign; it can form along the entire length of the nerve, but is more often located in the orbital part. Symptoms of optic nerve glioma: first, visual acuity decreases (as the nerve and elements of the eye are damaged), then bulging eyes develop.
- Diffuse glioma of the brainstem is highly malignant. Since diffuse dysplasia is formed in the area where the nerves responsible for the functioning of the limbs are located, when they are damaged, the coordination of the arms and legs is disrupted, up to paresis and paralysis. Clinical signs of diffuse pontine glioma are significant even with small sizes of dysplasia. There are many nerve cords passing through the bridge, so the clinic can be more diverse.
- Glioma of the frontal lobe of the brain is manifested by apathy, mental changes, the person becomes nervous, hot-tempered, and sudden mood changes are characteristic. The later stages of the disease are characterized by the onset of paralysis.
- Glioma of the temporal region causes impaired coordination of movements, memory deteriorates, and diction suffers. In addition, temporal lobe glioma negatively affects the sense of smell.
- Glioma of the cerebellum and cerebellar vermis leads to movement abnormalities. The gait is disturbed, it seems that the person is drunk. This is because it becomes difficult for the patient to maintain balance, his arms and legs do not obey, and maintaining the body in space becomes problematic.
- Glioma of the parietal lobe is accompanied by disturbances in fine motor skills, so a person’s handwriting changes, and over time it becomes difficult to write. Tactile sensations become dull.
- Glioma of the quadrigeminal plate or quadrigeminal plate causes visual disturbances, abnormalities in eye movement, and hearing impairment.
- Glioma of the corpus callosum is accompanied by visual hallucinations (the same ones occur in the presence of a tumor in the occipital lobe), violations of logic, as well as many other signs: changes in sensitivity, muscle weakness, and so on.
- Pontine glioma (diffuse or common) leads to disruption of conduction functions, since the nuclei of the cranial nerves are localized in this area. Therefore, the clinical picture will be quite broad. A violation of sensory perception, movements, and so on is recorded.
- Glioma of the cerebral ventricle leads to an increase in intracranial pressure due to disruption of the outflow of cerebrospinal fluid. Hydrocephalus may develop.
Tests and diagnostics
Diagnostics is based on imaging methods (MRI/CT) of the brain. These methods allow you to determine:
- location and size of pathological foci;
- the presence of marginal (perifocal) infiltration;
- structure (homogeneity) of the white matter of the brain;
- perivascular spaces of various areas;
- areas of the basal ganglia;
- the presence of other pathological formations;
- condition of the ventricles of the brain/pituitary gland, functionality/condition of the blood vessels of the brain.
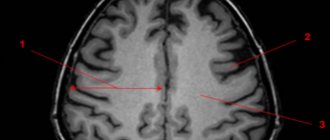
The image below shows multiple foci of gliosis.
MRI makes it possible to establish not only the presence of areas of gliotic changes, but also to identify the cause. MRI images provide a clear picture of the presence of areas in the brain that do not receive sufficient nutrition due to vascular obstruction by atherosclerotic plaques; allow you to identify inflammatory processes, areas of hematoma, and identify neoplasms. This, to a certain extent, makes it possible to eliminate the provoking factor and develop tactics to minimize the risks of further spread of the process.
Life prognosis for patients with gliosis
To talk about life prognosis, you need to remember what causes gliosis. Usually the disease is provoked by severe diseases of the cardiovascular and nervous systems. Therefore, mortality statistics from gliosis are imperfect: some patients die from primary diseases. But the average number of years that an adult with a similar diagnosis can live is two or three years.
With timely and high-quality treatment, this period can increase by almost one and a half times.
You can increase this period if you consult a doctor in time.
The fact is that only a doctor can determine how life-threatening glial tumors are. And only in a specialized clinic will it be possible to conduct a correct diagnosis and develop further therapy.
People living with gliosis experience paralysis, hearing and vision problems, and memory and attention disorders.
Unfortunately, even with proper treatment, the patient’s life is complicated by the side effects of the disease. For example, if a person develops supratentorial gliosis, it will be followed by hallucinations, the shapes and scales of objects will be distorted, and cognitive connections between the image of an object and its name will be disrupted. There is no guarantee that treatment will stop the development of gliosis completely, but this does not eliminate its need.
The internal organs and the lymphatic system are tightly connected. To stimulate the functioning of each system, regular lymph detoxification is required. Read more in the article: “stagnation of lymph in the body: symptoms and treatment.”
Diet
There is no special diet, but it is recommended to adhere to the diet recommended for the underlying disease that initiates the process of formation of glial lesions ( Diet for stroke , Diet for hypertension , atherosclerosis , diabetes mellitus , Diet for obesity , etc.). In general, it is recommended to adhere to a low-calorie diet with sufficient vitamin content (vegetables, fruits) and a minimum content of animal fats in the diet.
What is cerebral gliosis
The natural process of replacing dead neurons, which is protective in nature, is called gliosis of the white matter of the brain. Normally, over 10 years in a healthy body, about 4% of all neurocytes are destroyed, so gliosis is one of the manifestations of aging.
With the development of pathological processes that cause the death of a large area of nervous tissue, gliocytes replace dead impulse cells, although they cannot generate and conduct nerve impulses. Thanks to this, the spread of the pathological process slows down, and the metabolism of the affected area is preserved in full.
What causes the development of gliosis of brain tissue, what it is and at what point the process becomes dangerous
The CNS includes three types of cells:
- Neurons are the main functional cells of the nervous system, forming and transmitting impulses from the brain to effectors (executive organs that provide a response to a specific stimulus).
- Ependymal cellular elements lining the ventricles of the brain and the central spinal canal.
- Cells of glial tissue with supporting and protective functions. They form a scar after the death of neurocytes for various reasons, including due to demyelinating diseases.
Glial tissue (neuroglia) is located between the functional elements and is the support for all cellular structures. Normally, it protects the brain from injury due to sudden movements, as well as from the development of infectious processes.
Making up about 40% of the volume of all tissues of the skull, glia creates the conditions for the normal functioning of the nervous system. In critical situations, it forms a kind of scar, which does not allow metabolic processes to stop and partially takes over the tasks of other cells. In addition, neuroglia participate in the formation of new nerve fibers that isolate the lesion and protect healthy tissue.
Prevention
No drugs or methods of specific prevention of neuronal death have been developed. To maintain the activity of neuro-processes and brain vessels, we can only recommend:
- Lead a healthy lifestyle.
- Monitor your body weight.
- Maintain age-appropriate physical activity.
- Constantly monitor blood pressure, cholesterol , and blood sugar levels.
- Minimize bad habits.
- Practice a healthy balanced diet by minimizing foods containing animal fats.
- Train brain functions: solve puzzles/crosswords, learn poetry, foreign languages.
What to do and how to treat
There are no specific medical recommendations for eliminating the tumors in question. The treatment for brain gliosis prescribed by a specialist will be aimed at combating the disease that became the “trigger” mechanism for the appearance of gliosis. Medicines must be prescribed strictly by a doctor. Drug therapy will consist of taking medications that can maintain the condition of the blood vessels. In addition, patients are often prescribed antioxidants and nootropics to neutralize oxidative processes, because with this disease there is a lack of oxygen.
Diagnostics
To diagnose the disease, CT, MRI and EEG are performed. Let's consider in what cases one or another method is used.
Magnetic resonance imaging is the most preferred method. With its help, the doctor will see foci of gliosis in the frontal lobe and understand how advanced the situation is.
Computed tomography is also sometimes used by specialists to diagnose white matter gliosis in the brain. However, this method will not provide such a necessary clinical picture as MRI. A significant disadvantage for the patient will also be the presence of radiation during the procedure.
Electroencephalography - finding out how active the brain is. Electrodes and computer processing are used. This method is often used to clarify problems when epilepsy or seizures are present.
Often, in order to get a detailed picture, it makes sense to conduct additional examinations, namely, take tests or perform other manipulations.
Medicinal methods and surgery
Among drug therapy, commonly prescribed drugs are:
- Aimed at improving brain function;
- Improving cerebral circulation;
- Vitamins.
Surgeries are also considered if treatment with medications does not bring the desired result and any other treatment has been tried without a positive effect, but the focus of gliosis remains and the disease progresses.
Traditional treatment
In addition to the usual, traditional methods of treatment, there are also so-called traditional methods of combating gliosis, or rather the source disease.
So, to improve blood circulation, you can use the following herbs:
Dandelion root. Helps strengthen blood vessels and lowers cholesterol. Used as a decoction.
Melissa. Positive effect on the cerebral cortex, strengthens vascular walls, acts as a sedative, restoring nerve cells.
Dill seeds. They can restore blood circulation and help normalize blood pressure.
St. John's wort. Positive effect on vascular lesions, tissue restoration.
Dioscorea. Indicated for vascular and cardiac problems, relieves headaches. The root is crushed and brewed, after which it is taken several times a day, a tablespoon after meals.
Forecast
The prognosis of life with cerebral gliosis is largely determined by the underlying disease and can vary significantly depending on the volume of gliosis foci and the intensity of neuronal replacement. As a rule, the prognosis for life with single foci outside important brain structures is relatively favorable, while extensive foci of gliosis in areas of the brain responsible for important functions of the central nervous system can be unfavorable, for example, in the temporal lobe, initiating frequent epileptic seizures.
Treatment
currently no effective treatments for cerebral gliosis. This disease is not independent, but occurs as a consequence of the development of another disease. It is necessary to accurately diagnose the cause of nerve cell death and treat it.
If the cause is not identified or ignored, the glial fibers will grow as much as the brain will be affected. This condition is considered serious, and nothing can change the situation.
When this disease occurs in older , it is necessary to take preventive measures to slow down this pathological process. It is important to reduce blood pressure in a timely manner so that foci of gliosis do not grow.
Preparations:
- Medicines to improve brain activity.
- Drugs that improve blood circulation in the brain.
- Medicines to improve brain function.
- Vitamins , in particular, group B.
Having cured the cause of gliosis, there is no need for therapy aimed at inhibiting neuronal death.
List of sources
- Vereshchagin N.V., Gulevskaya T.S. Pathology of the brain in atherosclerosis and arterial hypertension. – M.: Medicine, 1997. – 228 p.
- Vasiliev V.N., Kindyashova V.V., Kozhevnikova V.V., Tikhomirova O.V., Lomova I.P., Serebryakova S.V. Clinical and diagnostic significance of microfocal brain lesions of vascular origin among management specialists // Medical, biological and socio-psychological problems of safety in emergency situations. 2014. No. 3. pp. 27-32.
- Gladky P. A., Sergeeva I. G., Tulupov A. A. Infectious lesions of the brain. Tutorial. Novosibirsk 2015. – 24 p.
- Putilina M.V. Chronic cerebral ischemia//Attending physician. 2005. No. 5.
- Yanishevsky S.N. Brain damage in patients with type 2 diabetes // International Journal of Endocrinology. No. 8(64). 2014 pp. 89-97.
Recovery period and life prognosis
The prognosis for life with benign glioma depends on the timeliness of treatment and the degree of malignancy of the tumor. The necessary information about the tumor can only be obtained through a comprehensive and thorough diagnosis.
Low-grade gliomas are attempted to be completely removed surgically. Usually this does not cause any difficulties due to the localized nature of the pathological focus. Surgical treatment is the gold standard of neurosurgery.
It is impossible to indicate the exact life expectancy after surgery for brain glioma. If the patient seeks help on time, and the neurosurgeon manages to completely remove the tumor, the prognosis for glioma will be favorable. Life expectancy can be increased with subsequent radiation therapy. It allows you to increase the five-year survival rate after surgery to 60%.
It is also important to follow all doctor’s recommendations during the rehabilitation period. During recovery after removal of a brain glioma, the patient is under the supervision of specialists of a narrow and broad profile. They monitor important indicators of the body’s functioning, help normalize overall well-being and restore impaired functions of the nervous system.
Which doctor should I contact?
If you suspect the presence of gliosis, you should consult a neurologist. After the studies have been carried out, consultation with specialists may be required to confirm the diagnosis and determine treatment tactics:
- cardiologist - if gliosis of vascular origin is suspected;
- general practitioner or family doctor - to determine chronic diseases;
- endocrinologist – for diabetes mellitus;
- neurosurgeon - if surgical treatment is necessary.
In children, a neonatologist can suspect the development of glial changes during the first month after birth. Later, developmental changes are identified by a pediatrician who will refer the child to a consultation with a pediatric neurologist.
Complications and consequences
The presence of extensive areas of replacement of neurons with gliocytes threatens with dangerous consequences:
- persistent headaches that cannot be controlled by medications;
- mental disorders;
- permanent loss of speech, vision or hearing;
- convulsions and epileptic seizures;
- paralysis (partial or complete);
- mental disorders;
- impaired coordination of movements;
In extremely rare cases, gliosis of non-genetic origin causes death.